Endovascular Brachiocephalic Revascularization
Timothy M. Sullivan
Introduction
Occlusive arterial disease involving the arteries to the head and arms is relatively common; the Joint Study of Arterial Occlusions noted that one-third of patients having arteriograms were found to have lesions involving at least one of these vessels. Those affecting the brachiocephalic trunks (supra-aortic trunks [SATs]) were relatively uncommon, however. The practicing vascular specialist will likely encounter patients with symptomatic brachiocephalic disease in clinical practice, but compared to other conditions requiring surgical repair of the cerebral and upper extremity vasculature like carotid endarterectomy, operations involving the SAT are less common.
The mainstay of revascularization of these vessels has traditionally involved endarterectomy and bypass, using both direct reconstruction and extra-anatomic procedures. Although the durability of these techniques remains exemplary, they have, in many instances, been supplanted by minimally invasive endovascular interventions. This chapter focuses on the indications, technique, and results of endovascular repair (balloon angioplasty and stenting) of the brachiocephalic vessels.
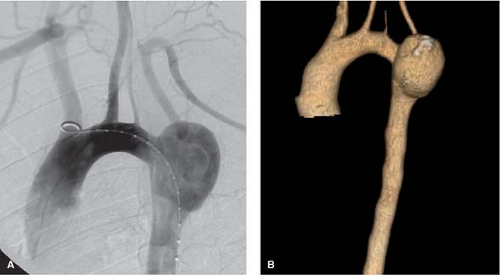
The typical configuration of the SAT includes three principal branches: the brachiocephalic trunk (innominate artery), the left common carotid artery (CCA), and the left subclavian artery. The innominate gives rise to the right common carotid and right subclavian arteries, and the vertebral arteries typically originate from the subclavians. Developmental anomalies and anatomic variations to this classic configuration are frequent, encountered in up to 30% of cases. The most common variant, which occurs in approximately 20% of patients, is the bovine arch. In this configuration, the left common carotid arises directly from the innominate artery or as part of a single ostium from the arch. Next in frequency (5%), the left vertebral may originate as a separate branch from the aortic arch, typically between the left common carotid and the left subclavian arteries (Fig. 1). Finally, the right subclavian artery may arise as the terminal branch of the arch (0.5%), typically passing posterior to the esophagus. Before considering endovascular intervention, the aortic arch should be visualized with standard contrast angiography (typically an aortic arch injection with a pigtail catheter in the 30-degree left anterior oblique projection), computed tomography angiography, or magnetic resonance angiography (MRA) to define anatomy and its possible variations.
Most patients with brachiocephalic occlusive disease will be asymptomatic due to the extensive collateral network that exists around the head and the neck. The vast majority of these patients should be treated conservatively (i.e., without surgical or endovascular intervention) until symptoms develop. There is some controversy regarding the treatment of asymptomatic high-grade stenosis of the left CCA, given the excellent results of open surgical therapy. It is the authors’ preference to treat these lesions, even in asymptomatic patients, if in fact the stenosis is critical (<80% angiographic stenosis) in a fit patient with a reasonable life expectancy.
As the left subclavian artery is the SAT most frequently affected by atherosclerotic occlusive disease, the most common presenting symptom complex is typically exercise-induced ischemia (“claudication”) of the left arm. This may occur with limited activity, depending on the abundance (or lack thereof) of collateral circulation, such as combing the hair. While angiographic subclavian steal (retrograde flow in the left vertebral artery secondary to occlusion/stenosis of the proximal left subclavian) is relatively common, symptomatic vertebral-basilar ischemia is less common. Patients with ulcerated atheroma may present with embolic lesions to the left upper extremity or to the posterior cerebral circulation via the vertebral artery; in the absence of fresh thrombus within the offending plaque, these lesions are typically amenable to endovascular intervention. Patients having
coronary bypass using the internal mammary artery (IMA) may present with acute and chronic coronary syndromes secondary to IMA-subclavian steal. Patients with occlusive disease of the left CCA may present with hemispheric transient ischemic attack (TIA) or stroke. Lesions of the innominate artery can cause symptoms referable to the right upper extremity, the right cerebral hemisphere, or both. Indications for endovascular repair of the brachiocephalic trunks in 83 consecutive patients treated at the Cleveland Clinic Foundation are listed in Table 1. Relative contraindications to endovascular intervention are listed in Table 2. Chronic occlusions of the innominate and left common carotid arteries are typically best suited to open surgical repair because of the high incidence of embolization associated with endovascular intervention; short-segment occlusions of the left subclavian artery, however, are typically safely treated with angioplasty and stenting if the lesion can be traversed with a guidewire. Extremely calcified lesions should be approached with caution because of an increased risk of rupture with aggressive balloon inflation and an inability to achieve complete stent expansion.
coronary bypass using the internal mammary artery (IMA) may present with acute and chronic coronary syndromes secondary to IMA-subclavian steal. Patients with occlusive disease of the left CCA may present with hemispheric transient ischemic attack (TIA) or stroke. Lesions of the innominate artery can cause symptoms referable to the right upper extremity, the right cerebral hemisphere, or both. Indications for endovascular repair of the brachiocephalic trunks in 83 consecutive patients treated at the Cleveland Clinic Foundation are listed in Table 1. Relative contraindications to endovascular intervention are listed in Table 2. Chronic occlusions of the innominate and left common carotid arteries are typically best suited to open surgical repair because of the high incidence of embolization associated with endovascular intervention; short-segment occlusions of the left subclavian artery, however, are typically safely treated with angioplasty and stenting if the lesion can be traversed with a guidewire. Extremely calcified lesions should be approached with caution because of an increased risk of rupture with aggressive balloon inflation and an inability to achieve complete stent expansion.
Table 1 Indications for Endovascular Repair of the Brachiocephalic Trunks in 83 Consecutive Patients | ||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree