, Kyu Eun Lee1 and June Young Choi1
(1)
Department of Surgery, Seoul National University Hospital, Seoul, Korea, Republic of (South Korea)
Abstract
The operating theater for endoscopic thyroidectomy is similar to that of open thyroidectomy. The room is a clean and sterile space to perform the operation in aseptic manners.
Electronic supplementary material
The online version of this chapter (doi:10.1007/978-3-642-37262-9_3) contains supplementary material, which is available to authorized users.
3.1 Basic Equipment and Instruments of Endoscopic Thyroidectomy
3.1.1 The Operating Theater
The operating theater for endoscopic thyroidectomy is similar to that of open thyroidectomy. The room is a clean and sterile space to perform the operation in aseptic manners.
3.1.2 Instruments
3.1.2.1 Endoscope
5-mm 30° endoscope (Karl Storz Endoscopy Inc., California, USA)


Fig. 3.1
5-mm 30° endoscope
3.1.2.2 Thyroid Pillow (Emtas, Korea)

Fig. 3.2
Thyroid pillow
3.1.2.3 Harmonic® (Ethicon Endo-Surgery, Cincinnati, Ohio, USA)
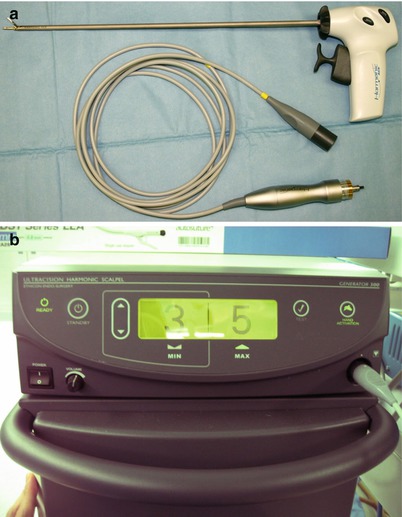
Fig. 3.3
Harmonic® (a) handpiece, (b) generator
3.1.2.4 Vascular Tunneler (Gore-Tex)

Fig. 3.4
Vascular tunneler
3.1.2.5 Suction-Irrigator

Fig. 3.5
Suction-irrigator
3.1.2.6 Trocar (Ethicon Endo-Surgery, XCEL: B12XT, B5XT)
1 trocar, Ф12 mm, 15 cm long
3 trocars, Ф5 mm, 15 cm long
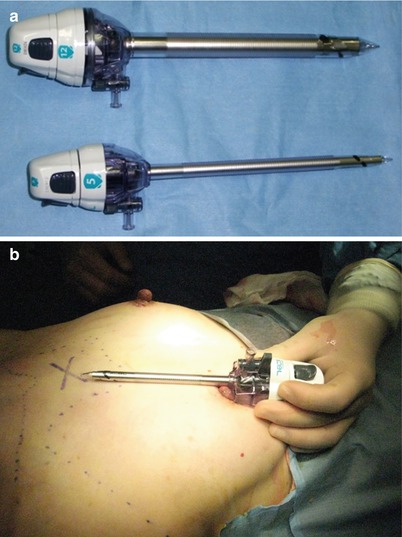
Fig. 3.6
Trocars. (a) Ф12-mm trocar (upper), Ф5-mm trocar (lower), and (b) 15-cm long trocar are needed to reach the operative field
3.1.2.7 Snake Retractor, Ф5 mm
Right and left snake retractors
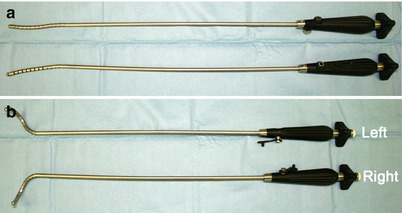
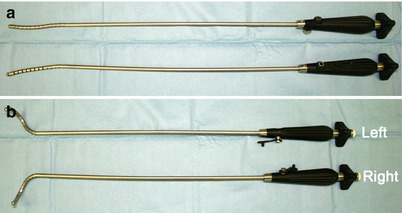
Fig. 3.7
Snake retractor. (a) open, (b) closed
3.1.2.8 Endobag, Ф10 mm
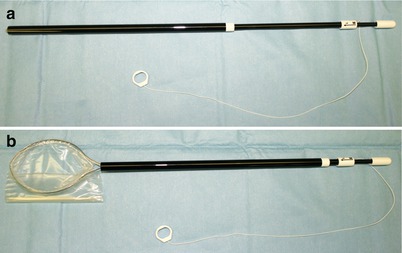
Fig. 3.8
Endobag. (a) closed, (b) open
3.1.2.9 Endo-suture and Endo-needle Holder, Ф5 mm
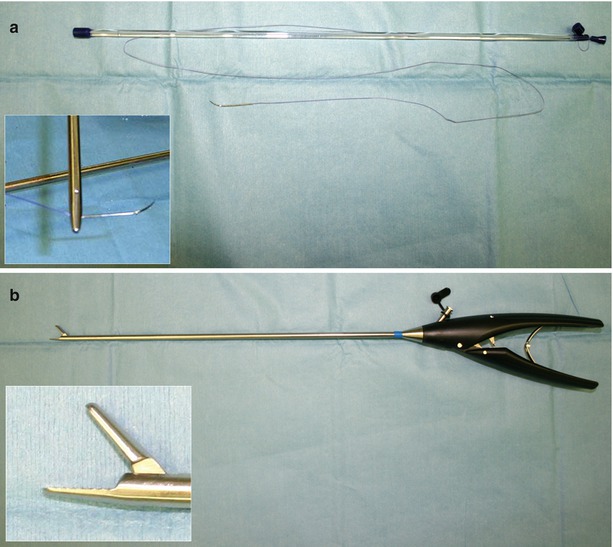
Fig. 3.9
(a) Endo-suture, (b) endo-needle holder
3.1.2.10 Basic Instruments
1 Endo-clinch, Ф5 mm
1 Endo-Maryland forceps, Ф5 mm
1 Endo-right-angled forceps, Ф5 mm
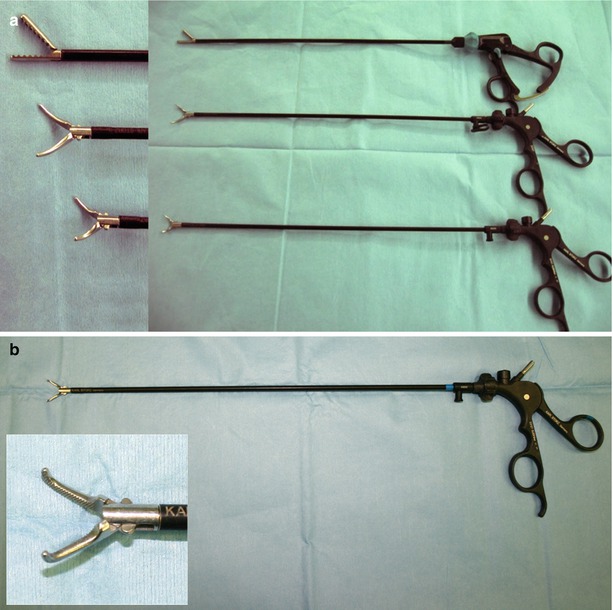
Fig. 3.10
Endoscopic instruments. (a) Endo-clinch and endo-Maryland forceps, (b) endo-right-angled forceps
3.1.2.11 Two 10-mL Syringes with 22-G Spinal Needle
200 mL of normal saline with 1 mL of 1 % epinephrine (1:200,000)


Fig. 3.11
200 mL of epinephrine-saline
3.2 Patient Selection: Indications and Contraindications
Indications for endoscopic thyroidectomy are as follows: (1) benign thyroid nodules that are needed to be excised (the size of nodule is not considered to be important, but for beginners, the nodule less than 3–4 cm in diameter is preferable), (2) for diagnosis for the nodules of suspicious for follicular neoplasm or Hurthle cell neoplasm, and (3) completion thyroidectomy of the patient diagnosed with follicular carcinoma or Hurthle cell carcinoma of previous diagnostic lobectomy.
Absolute contraindications for endoscopic thyroidectomy are the patient with previous open neck surgery, thyroid malignancy which expected to recur easily (i.e., medullary thyroid cancer, advanced papillary thyroid cancer, and poorly differentiated thyroid cancer), and overt breast malignancy.
Relatively not recommended patients for endoscopic thyroidectomy are with large size thyroid nodules over 5 cm in diameter, male patient (due to the prominent clavicle and no breast mound which allows movability of the instruments), with Graves’ disease, and with well-differentiated thyroid carcinoma over 1 cm in diameter.
3.3 Procedures of Bilateral Axillo-Breast Approach (BABA) Endoscopic Thyroidectomy
3.3.1 Patient Positioning
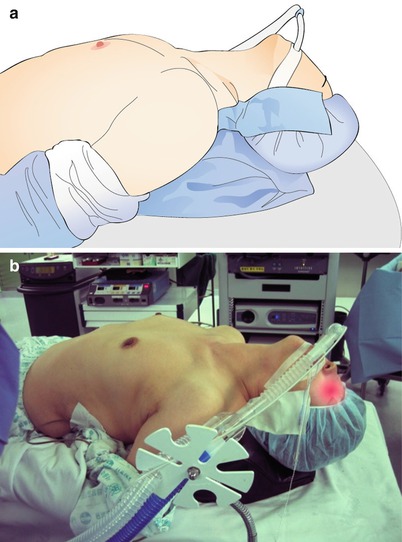
Fig. 3.12
Position of patient. (a) illustration, (b) photo
The patient is placed in supine position on the operating table with the Q-pillow underneath his/her shoulders. Extend the patient’s neck to expose the operative field (i.e., anterior neck).
Arms should be fixed in the abducted position in order to expose the axillae.
The blood pressure cuff is placed on the patient’s ankle.
3.3.2 Skin Preparation

Fig. 3.13
Skin preparation
Antiseptic solution is applied to the patient’s skin from the patient’s chin to the xiphoid process. Axillae and proximal regions of arms are also prepared with antiseptic solution.
3.3.3 Draping
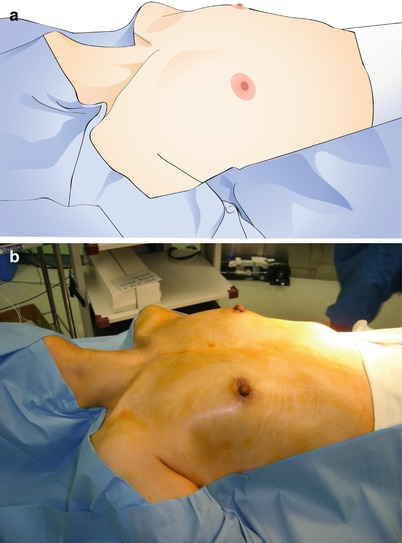
Fig. 3.14
Draping of the operative field. (a) illustration, (b) photo
Cover the patient with sterile universal drapes, except the anterior neck and both axillae and breasts.
3.3.4 Field Setup
Sterilized devices and lines should be installed on the operative field:
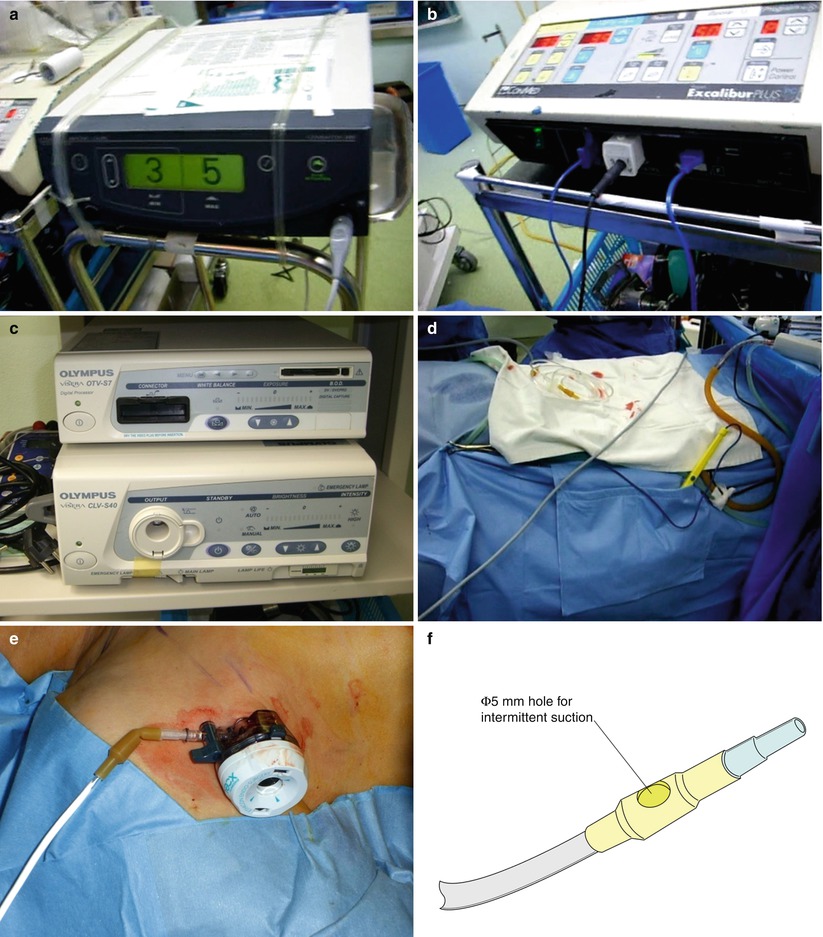
Harmonic® and endo-electrocautery
Camera line
CO2, suction, and irrigation lines
Air vent
Bovie pedal
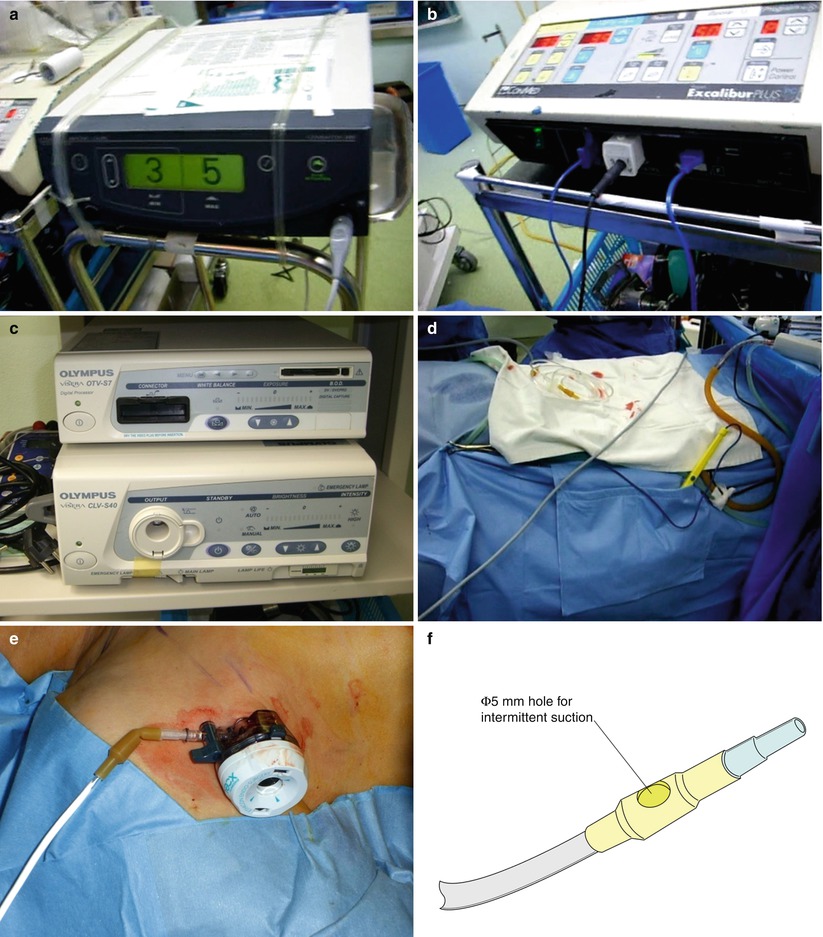
Fig. 3.15
Field setup. (a) Harmonic®, (b) electrocautery, (c) camera and light source, (d) operative field setup, (e) air vent, and (f) making air vent with IV extension
3.3.5 Operating Room Setup
Fig. 3.16
Operating room setup (for right lobectomy)
Fig. 3.17
Operating room setup (for left lobectomy)
Here is the schematic depiction of the aerial view of the operating room setting for endoscopic thyroidectomy. For right lobectomy, the operator stands on the left side of the patient and vice versa for left lobectomy.
3.3.6 Drawing Guidelines on the Body
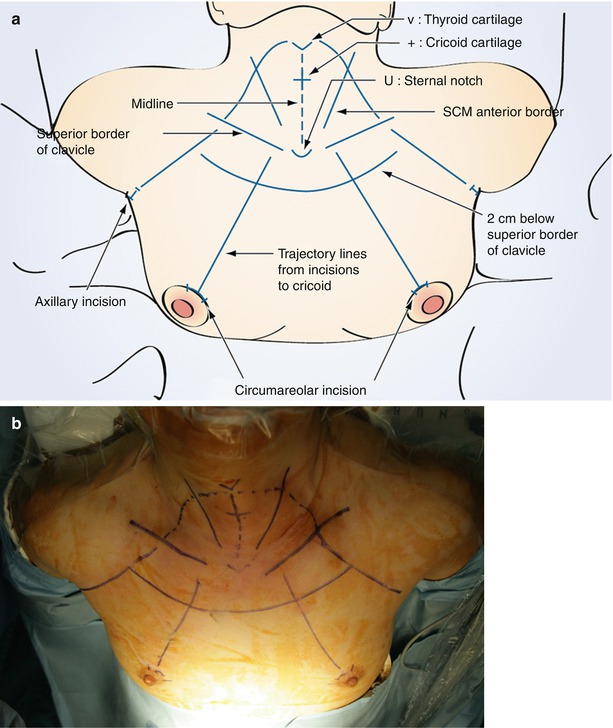
Fig. 3.18
Guidelines of BABA endoscopic thyroidectomy. (a) illustration, (b) photo
Draw marking lines along the landmarks of the chest and the neck – midline, thyroid cartilage (V), cricoids cartilage (+), anterior border of the SCM muscle, superior border of the clavicles, suprasternal notch (U), incisions, trajectory lines from the port site to the thyroid gland, and the working spaces as well.
3.3.7 Saline Injection
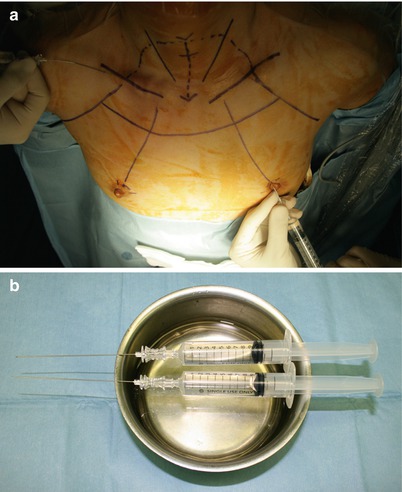
Fig. 3.19
(a) Epinephrine-saline injection in the chest, (b) epinephrine-saline and syringe
Diluted epinephrine solution (1:200,000) is injected in the working area under the platysma in the neck and subcutaneously in the anterior chest. In the neck area, a “pinch and raise” maneuver of the skin facilitates the injection of saline into the subplatysmal area. This “hydrodissection” technique results in the formation of a saline pocket in the subplatysmal layer, which decreases the bleeding in the flap area and makes the subsequent dissection easier (Fig. 3.20).
Note: Drawing the plunger backward before making the injection will prevent intravenous injection of the solution which may cause high blood pressure and tachycardia.
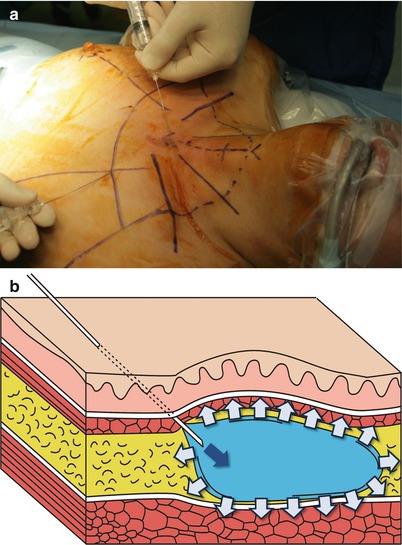

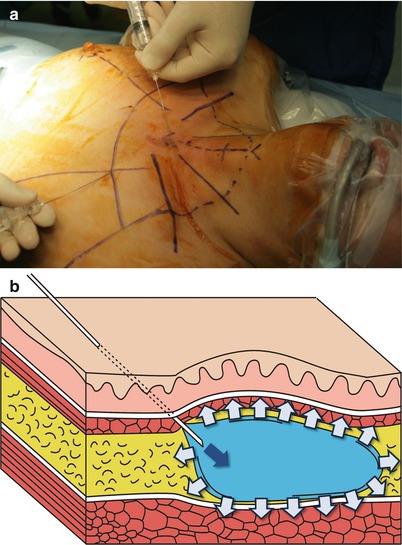
Fig. 3.20
(a) Epinephrine-saline injection in the neck, (b) the concept of hydrodissection

Fig. 3.21
Pinch and raise technique
Pinch and raise technique is a useful method to avoid the needle injury to the trachea and the major vessels.
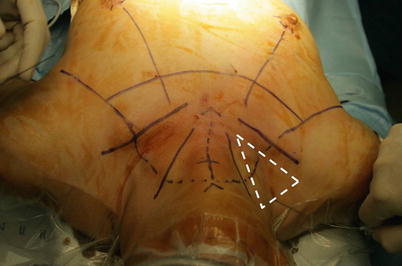
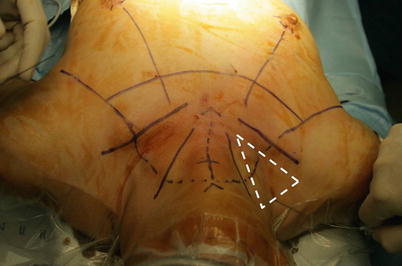
Fig. 3.22
Dangerous zone of puncture
Injecting saline in the supraclavicular area should be avoided because of the risk of pneumothorax.
3.3.8 Skin Incision and Blunt Dissection
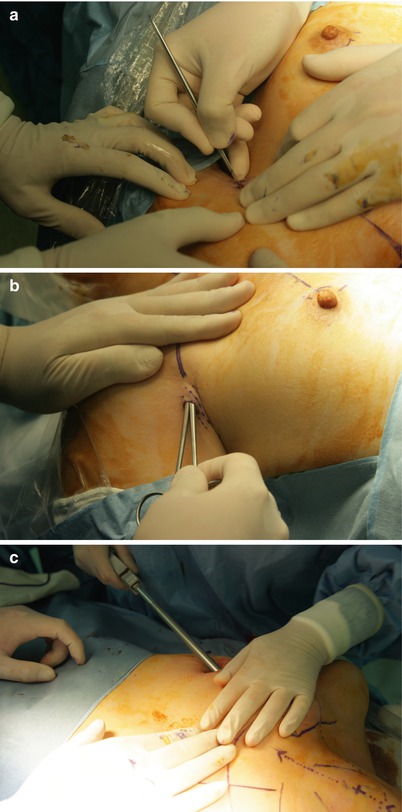
Fig. 3.23
(a) Skin incision, (b) blunt dissection with mosquito hemostats, and (c) blunt dissection with vascular tunneler
Make incisions in the superomedial margin of the areolar of the breasts and left and right axillary folds. Make a blunt dissection and elevate the flap, and make working spaces with straight mosquito hemostats, long Kelly clamps, and a vascular tunneler through the incisions subsequently.
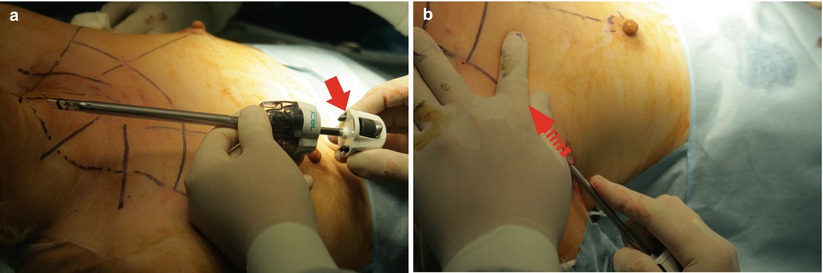
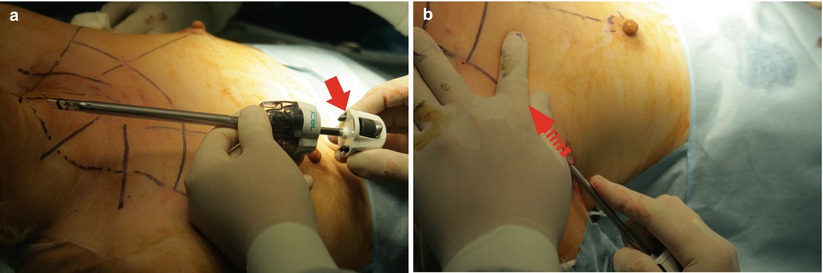
Fig. 3.24
(a, b) An alternative technique; blunt dissection using an obturator of 5-mm trocar (marked by arrow)
3.3.9 Trocar Insertion
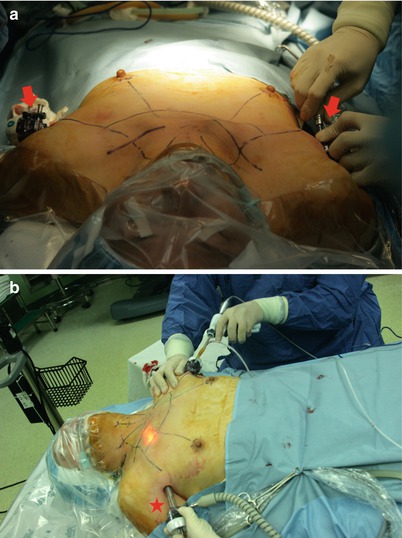
Fig. 3.25
(a) Axillary port insertion and (b) sharp dissection with Harmonic®. A 12-mm port is made on the right axilla (marked by star)
After elevating the flap from the port sites up towards the cricoids cartilage, the trocars are inserted through the incisions. For two breast incisions and the left axillary incision, 5-mm trocars are used, while for the right axillary incision, a 12-mm trocar is inserted (Fig. 3.25). A 12-mm port is usually made to the lesion side to extract the specimen.


Fig. 3.26
Breast port insertion
Fig. 3.27
Port (incision) size of BABA endoscopic thyroidectomy. Dissection should start at “area 2” (marked by red star) and elongate to “area 1”
The working space is insufflated with CO2 gas at the pressure of 5–6 mmHg via a 12-mm port. The dissection should start in area 2 and the flap is extended to area 1, up to the thyroid cartilage in the cephalad direction, and laterally towards the anterior border of the SCM muscle (Fig. 3.27).
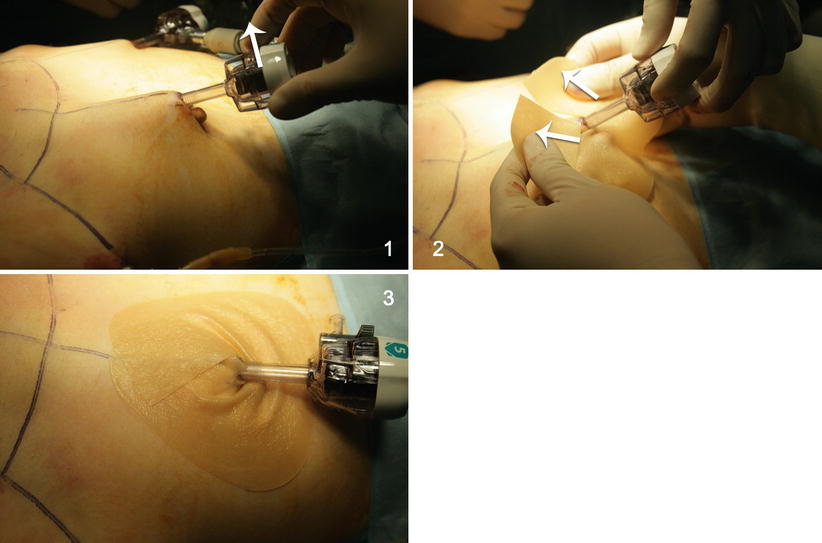
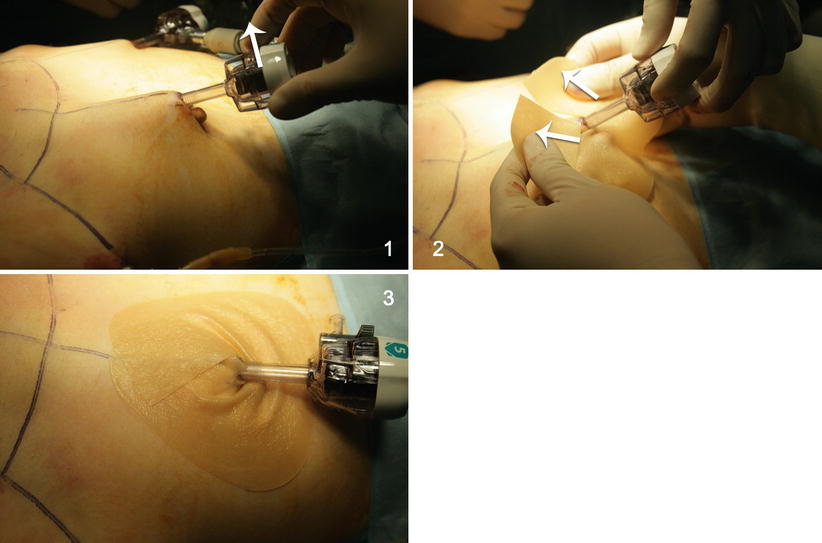
Fig. 3.28
DuoDERM® application to protect the nipple
DuoDERM® is applied on bilateral breast incisions in order to protect the nipples before inserting the trocars.
3.3.10 Midline Incision
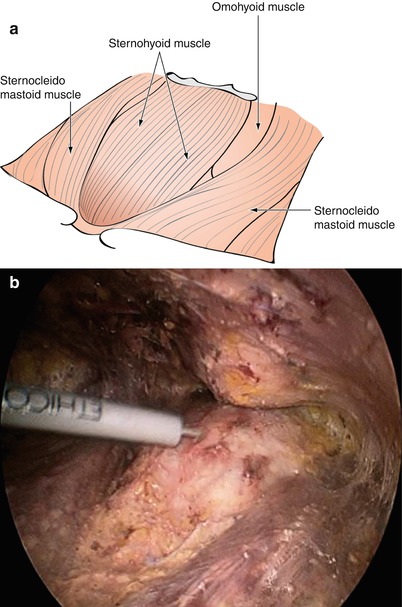
Fig. 3.29




Basic structures of the operative field and identification of the midline by external palpation. (a) illustration, (b) photo
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


