Endocrine Physiology
HORMONES
What is a hormone?
A chemical substance, formed in a tissue or organ and carried in the blood, that stimulates or inhibits the growth or function of one or more other tissues or organs
What is an endocrine pathway?
A hormone secreted into blood that acts on distant target cells
What is a paracrine pathway?
A hormone released from one cell that acts on neighboring cells
What is an autocrine pathway?
A hormone released that acts on the cell that secreted it
What is the fundamental mechanism of all hormone action?
Reversible, noncovalent binding to specific receptors on or in target cell
What are the three major classes of hormones?
- Peptide hormones
- Steroid hormones
- Amine hormones
How are polypeptide hormones synthesized?
Peptide hormones are produced en masse during times of quiet and subsequently released into circulation in response to stimuli
Preprohormone produced from mRNA
↓ proteins cleaved
Prohormone↓ cleaved
Hormone (Golgi apparatus)
↓
Packaged into secretory granules for release
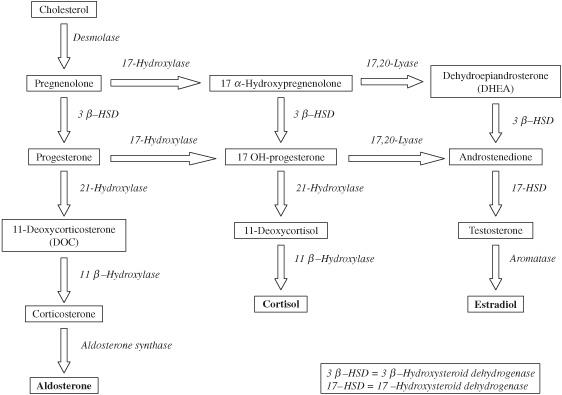
How are steroid hormones synthesized?
Steroid hormones are not stored in intracellular vesicles and must be synthesized on demand. They use the following general pathway:
Cholesterol
↓
Pregnenolone (mitochondria)
↓
Side chain modifications (in the endoplasmic reticulum)
↓
Various hormones
How are amino acid hormones synthesized?
Production is similar to peptide hormones in that they are synthesized and stored, but tend to be smaller, generally simpler, molecules
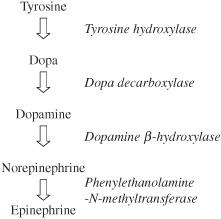
Tyrosine
↓ hydroxylation
↓ decarboxylation
Dopamine
↓ (many steps)
Various hormones
Where are polypeptide hormone receptors?
On the surface of target cell membranes
Where are steroid hormone receptors?
In the target cell cytoplasm
Where are amino acid hormone receptors?
These can be either on or inside the target cells. Two examples are:
Catecholamines: on target cell membrane
Thyroid hormones: in target cell cytoplasm
From Chap. 2, what is meant by “second messenger cascade”?
These are the systems that are used by receptors (of various types) that utilize intermediaries to cause intracellular changes
What are G-proteins?
A second messenger system; guanosine 5’-triphosphate (GTP)-binding proteins that couple hormone receptors on the cell surface to a secondary messenger system inside the cell
What type of intrinsic property do G-proteins have?
GTPase activity
What types of G-proteins are there?
Either stimulatory (Gs) or inhibitory (Gi)
What are G-proteins comprised of and what determines activity?
Three subunits: alpha, beta, and gamma. When the alpha subunit is bound to GTP, the G-protein is activated. It is inactivated when bound to GDP.
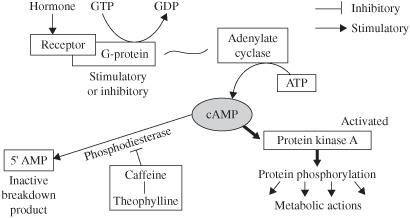
Describe, in words, the mechanism of the cyclic adenosine monophosphate (cAMP) second messenger system.
Hormone binds G-protein-coupled
receptor on membrane
↓
GDP replaced by GTP to activate G-protein
↓
Activation of adenylate cyclase
↓
↑[cAMP]intracellular
↑protein kinase A phosphorylation of proteins
↓
Activation/inhibition of a metabolic process
Figure 7.1 cAMP pathway. Note that caffeine and theophylline both inhibit phosphodiesterase, thereby maintaining cAMP as active.
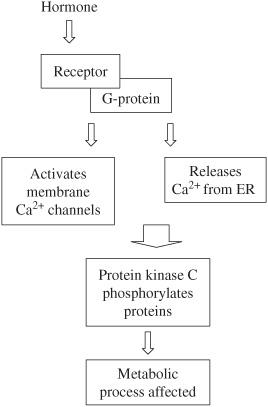
Describe, in words, the mechanism of the inositol triphosphate (IP3) second messenger system.
Hormone binds G-protein-coupled receptor
↓
Activates phospholipase C
↓
Frees diacylglycerol (DAG) + IP3 from membrane
↓
Ca2+ release from ER
↓
Activates protein kinase C
phosphorylation of proteins
↓
Activation/inhibition of a metabolic process
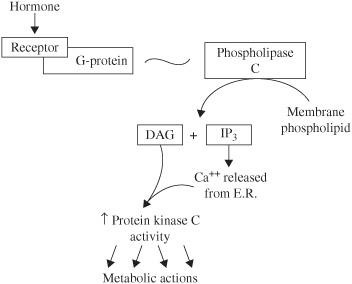
Figure 7.2 IP3 pathway.
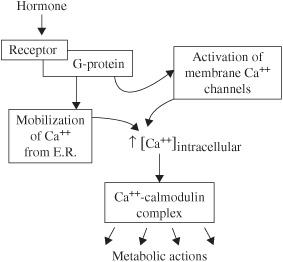
Describe, in words, the mechanism of the intracellular Ca2+-calmodulin second messenger system.
Hormone binds G-protein-coupled receptor
↓
Activates membrane Ca2+ channel and also releases Ca2+ from ER
↓
↑intracellular Ca2+
↓
↑ Ca2+ -calmodulin complex
↓
Regulation of other enzyme activities
Figure 7.3 Ca2+-calmodulin pathway.
Describe the mechanism of the steroid hormone activation.
Steroid hormone crosses cell membrane (readily soluble in lipid bilayer)
↓
Binds to cytoplasmic receptor
↓
Hormone-receptor complex enters nucleus
↓
Exposes DNA-binding domain on receptor
↓
Complex interacts with DNA to initiate or upregulate transcription
↓
Protein is then synthesized which activates physiologic pathways
What are the two principles of hormone receptor reregulation?
- Down-regulation: ↓ number or affinity of receptor for a hormone
- Up-regulation: ↑ number or affinity of a receptor for a hormone
Generally speaking, why does reregulation occur?
It occurs in response to over- or understimulation. An overstimulated receptor will be down regulated to limit activation and vice versa.
What are the two principles of regulation of hormone secretion?
- Negative feedback (most common)
- Positive feedback (rare)
A hormone’s actions directly or indirectly inhibit its own secretion—a self-terminating cycle
What is positive feedback?
A hormone’s actions directly or indirectly promote its own secretion—a self-perpetuating cycle. These cycles are far rarer than negative feedback cycles.
HYPOTHALAMUS AND PITUITARY GLAND
Name the hormones of the:
Anterior pituitary
Thyroid stimulating hormone (TSH)
Luteinizing hormone (LH)
Follicle stimulating hormone (FSH)
Growth hormone (GH)
Prolactin (PRL)
Adrenocorticotropic hormone (ACTH)
Posterior pituitary
Oxytocin
Antidiuretic hormone (ADH)
The following hormones are released from the hypothalamus, name the corresponding pituitary hormones and their respective functions:
Thyrotropin-releasing hormone (TRH)
↑ TSH, PRL secretion; encourages thyroid synthesis and secretion, as well as prolactin secretion
Gonadotropin-releasing hormone (GnRH)
↑ LH, FSH secretion; important regulatory elements of the sex hormones
Corticotropin-releasing hormone (CRH)
↑ ACTH secretion (and α-[MSH], β-endorphin); stimulates the adrenal cortex to release cortisol
Growth hormone-releasing hormone (GHRH)
↑ GH secretion; a complex hormone that influences catabolism throughout the body.
Somatostatin (SS)
↓ release of GH, TSH (among others); a counterregulatory hormone
Prolactin inhibitory factor (PIF)
↓ release of prolactin; another regulatory hormone
Name the anatomic connection between the hypothalamus and the following:
Anterior pituitary
Hypothalamic-hypophysial portal system
Posterior pituitary
Hypothalamic tract
What is unique about the posterior lobe?
It is a collection of nerve axons whose cell bodies are located within the hypothalamus
What is the hypothalamic-hypophysial portal system?
Capillaries that carry blood from the hypothalamus to the anterior pituitary and from the anterior pituitary back to the hypothalamus
What is meant by retrograde blood flow in the hypophysial portal system?
Blood flow traveling from the pituitary back to the hypothalamus
What is the significance of the retrograde blood flow?
Feedback to the hypothalamus
How are the anterior pituitary hormones categorized?
GH-related hormones
Glycoprotein hormones
Corticotropin-related hormones
What is unique about the homology of the following?
GH-related hormones
GH is a polypeptide and is homologous with PRL and HPL
Glycoprotein hormones
All contain α- and β-subunits—α-subunits are similar; hormonal activity comes from β-subunits
Corticotropin related hormones
All are from the same precursor, proopiomelanocortin (POMC)
Describe the POMC protein.
It is a long protein that can be variably cleaved into different proteins, depending on the stage of development and the needs of the organism
Figure 7.4 POMC processing. The portion of POMC that is cleaved determines the metabolic activity.
Name the actions of the anterior pituitary hormones.
TSH
↑ T3 and T4 production (see thyroid section)
LH
↑ estrogen, androgen production
FSH
↑ oocyte and sperm maturation (see Chap. 8)
GH
↓ general growth
↑ glucose uptake into cells → diabetogenic
↑ protein synthesis
↑ lipolysis
↑ IGF production in liver
PRL
↑ milk production
↑ breast development
Inhibition of ovulation and spermatogenesis via ↓ GnRH
ACTH
↑ glucocorticoid production (see adrenal section)
What hormone is downstream to GH that is imperative in growth and development?
Insulin-like growth factor (IGF)
Name the actions of GH that are mediated through IGF.
↑ protein synthesis in bone, muscle, and organs → ↑ linear growth, ↑ lean body mass, and ↑ organ size
When during a lifetime is GH release greatest?
During the “growth spurt” of puberty
During a 24-hour period, when is GH the highest?
Around midnight
What factors ↓ GH secretion?
- GHRH
- Sleep
- Stress
- Exercise
- Starvation
- Hypoglycemia
What factors ↓ GH secretion?
- GH and IGF (negative feedback)
- Obesity
- Hyperglycemia
- Somatostatins
Diagram the GH feedback loop.
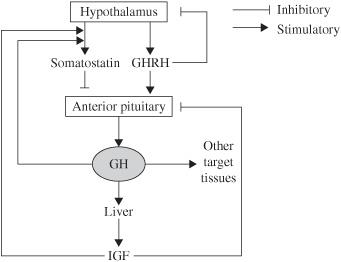
Figure 7.5 GH feedback loop.
In children, what do we call the clinical condition wherein excess GH is released?
Gigantism. The epiphyseal plates are open and children experience linear growth in excess of expected. In adults this leads to acromegaly.
What factors ↑ prolactin secretion?
Breast-feeding (most important stimulus)
Stress
TRH
Dopamine antagonists
What factors ↓ prolactin secretion?
Dopamine (PIF)- tonic inhibition prolactin (negative feedback)
Dopamine agonists (e.g., bromocriptine)
SS
Diagram prolactin secretion and negative feedback.
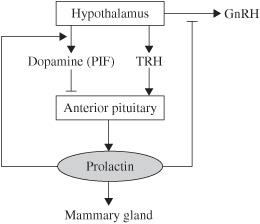
Figure 7.6 Prolactin secretion. Prolactin also inhibits GnRH which discourages the gonadal hormones and thereby pregnancy.
Name the actions of the posterior pituitary hormones.
Oxytocin
↑ contraction of myoepithelial cells in breasts (↑ milk ejection)
↑ contraction of uterus
ADH
↑ H2O permeability of the distal tubule and collecting duct
Constricts vascular smooth muscle
What type of hormones are oxytocin and ADH?
Polypeptide hormones
Supraoptic nuclei of the hypothalamus
Where are oxytocin and ADH stored and released?
Posterior pituitary
How are oxytocin and ADH synthesized and secreted?
Precursor protein
↓
Cleaved and packaged into secretory
granules with neurophysins
(carrier proteins)
↓
Transported by axoplasmic flow to posterior pituitary
What is the ADH receptor used in the kidney and in vascular tissue? What is its second messenger system?
Renal effect: V2 receptor → cAMP
Smooth muscle effect: V1 receptor → IP3
What factors ↑ ADH secretion? (See also Chap. 5)
High serum osmolarity (directly)
Volume depletion (indirectly)
Pain (minor)
Nausea (minor)
Hypoglycemia (minor)
Nicotine (minor)
Opiates (minor)
What factors ↓ ADH secretion? (See also Chap. 5)
Low serum osmolarity
Atrial natriuretic peptide (ANP)
α-Agonists
Ethanol
How does the hypothalamus sense osmolarity changes of serum?
Specialized vessels in the region lack the standard blood-brain barrier, perivascular cells swell or shrink according to the tonicity of serum. This provides information via specialized mechanoreceptors
Where is oxytocin synthesized?
Paraventricular nuclei of the hypothalamus
What factors regulate oxytocin secretion?
Breast-feeding
Sight or sound of infant
Dilation of cervix
What effect does lithium have on the body’s response to ADH?
Decreases the response through nephrogenic resistance
ADRENAL GLAND
What are the three zones of the adrenal cortex (from outer to inner zones) and what do they produce?
Zona Glomerulosa—Mineralocorticoids
Zona Fasciculata—Glucocorticoids
Zona Reticularis—Androgens
*Remember: “GFR” makes “salt, sugar, sex”
What are the special cells of the adrenal medulla called?
Chromaffin cells
What are the embryological origins of chromaffin cells?
Neural crest cells
What is the product of the adrenal medulla?
Catecholamines: epinephrine (Epi), norepinephrine (NE)
What controls the release of catecholamines from the medulla?
Discussed at length in Chap. 2, but recall that the chromaffin cells, derived from neural crest cells, are simply modified postganglionic sympathetic neurons, so release of catecholamines is a consequence of CNS sympathetic discharge.
From what are the adrenocortical (steroid) hormones derived?
Cholesterol
Figure 7.7 Steroid hormone pathway.
’Remember, individual layers of cortex have the portion of the pathway necessary to produce their primary hormone.
Which zone of the adrenal gland is the only producer of aldosterone synthase?
The zona glomerulosa, that is why it is the only zone to produce aldosterone
What happens when there is an enzyme deficiency in the pathway?
Steroid intermediates will accumulate above the level of the missing enzyme, and will be shunted down an alternative pathway.
What is the most common enzyme deficiency?
21 β-Hydroxylase
What steroids will be produced in excess if there is a deficiency in:
21 β-Hydroxylase
Mineralocorticoid and glucocorticoid production is halted, and adrenal androgen production will be increased.
17α-Hydroxylase
Decreased glucocorticoid and androgen production, increased mineralocorticoid production
What is special about the enzymes of the steroid hormone pathway?
Most are members of the cytochrome P 450 system
What is the rate-limiting step in the synthetic pathway?
Cholesterol desmolase; the initial step in all steroid pathways.
How is this step regulated?
ACTH
Name the actions of ACTH.
- ↑ activation of desmolase
- preferential expression of enzymes leading to cortisol synthesis
- ↑ cholesterol uptake into adrenal cortex
- ↑ proliferation of zona fasciculata if ACTH elevation is prolonged
What factors ↑ ACTH secretion?
- CRH
- Circadian rhythm-peak in the early morning
- Emotions/stress
- Central nervous system (CNS) trauma
What factors ↓ ACTH secretion?
Cortisol (negative feedback)
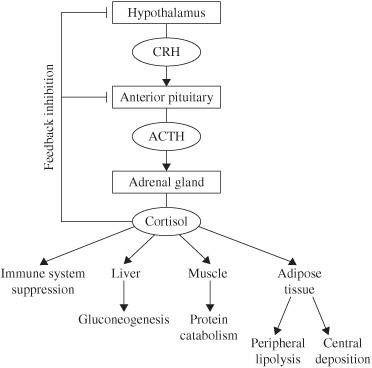
Figure 7.8 CRH, ACTH, cortisol loop.
Clinically, what is the most important stimulus for cortisol secretion?
Stress and illness; through all of the mechanisms discussed below it is the predominate counter-regulatory hormone for acute inflammation.
Name the actions of cortisol.
↑ hepatic gluconeogenesis
↓ protein synthesis
↑ protein degradation
↓ bone formation
↓ insulin sensitivity
↓ immune/inflammatory response
↓ ACTH secretion (negative feedback)
Facilitate vasoconstrictive properties of arterioles to catecholamines via alpha-1 receptor up-regulation
How does cortisol suppress the immune/inflammatory response?
Induces the synthesis of lipocortin, which inhibits the formation of arachidonic acid
Inhibits IL-2 production
Inhibits the release of histamine and serotonin from mast cells and platelets
Name the primary actions of aldosterone.
↑ Na+ resorption in renal distal tubules and ↑ K+ and H+ excretion
What factors regulate aldosterone synthesis?
- Renin-angiotensin II-aldosterone system
- ↑ K+
- Some tonic control by ACTH
Describe the renin-angiotensin-aldosterone pathway.
Decreased perfusion of the juxtaglomerular apparatus (JGA) in the kidney stimulates the release of renin. Renin cleaves the inactive peptide angiotensinogen to angiotensin I. The angiotensin converting enzyme (ACE) converts angiotensin I to the active peptide, angiotensin II, which acts as a potent vasoconstrictor and stimulates the release of aldosterone from the adrenal cortex. Aldosterone, in turn, stimulates the reabsorption of Na+ and water, increasing blood volume.
When is the renin-angiotensin II-aldosterone system activated?
- ↓ blood volume
- ↓ serum Na+
What cells monitor hyponatremia and hypovolemia to regulate renin release?
Hypovolemia is detected by arterial baroreceptors which communicate with the JGA via the nervous system. The macula densa of the distal tubule monitors sodium concentrations and communicates with the juxtaglomerular cells to release renin when that value falls.
Where is ACE found?
Lungs (major) and vasculature (minor)
What other systems are influenced by aldosterone?
Many, aldosterone works nearly everywhere sodium can be lost, so in addition to the vascular and renal systems, the GI tract and even sweat glands are affected.
How are all the above steroid hormones inactivated and excreted?
- Catabolized by liver (majority)
- Excreted through urine and bile/stool
From what precursor are the catecholamines derived?
Tyrosine
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree