FIGURE 11-1
(A) Glucagon
(B) Insulin
(C) Pancreatic polypeptide
(D) Somatostatin
(E) Vasoactive intestinal polypeptide
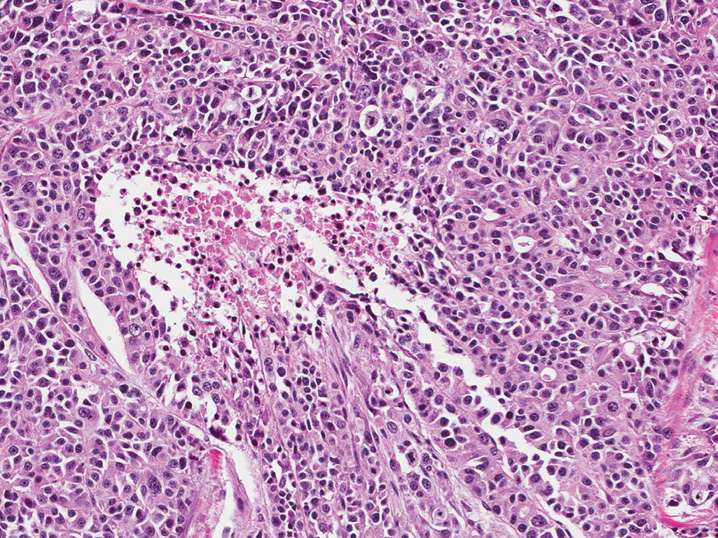
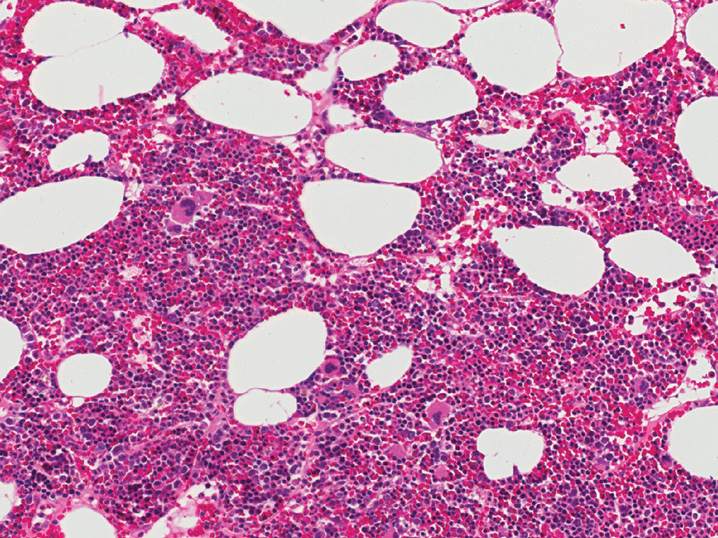
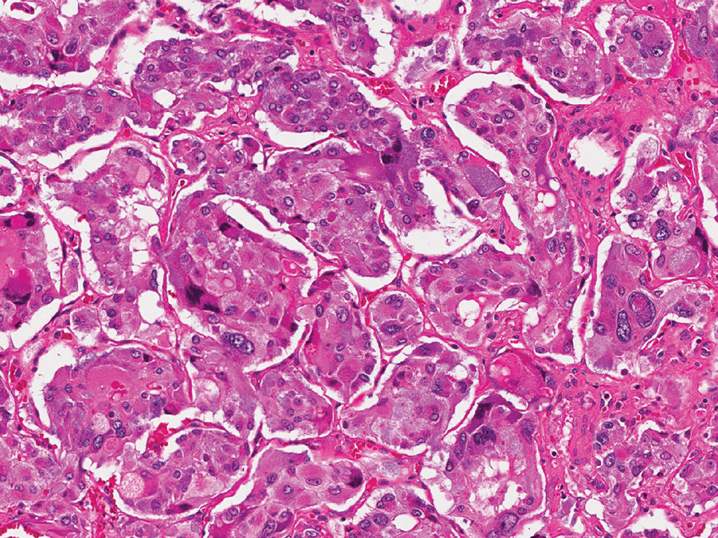
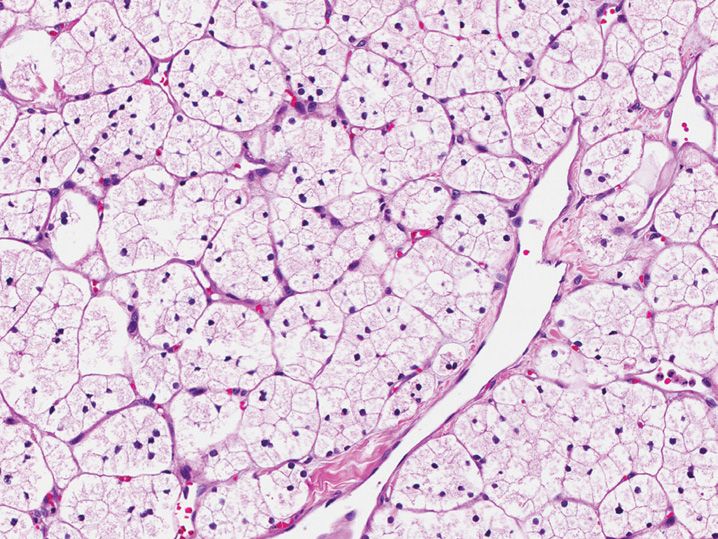
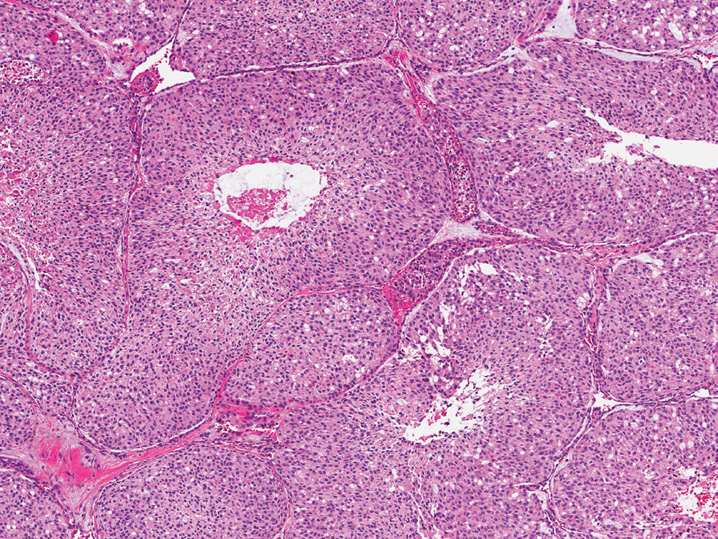
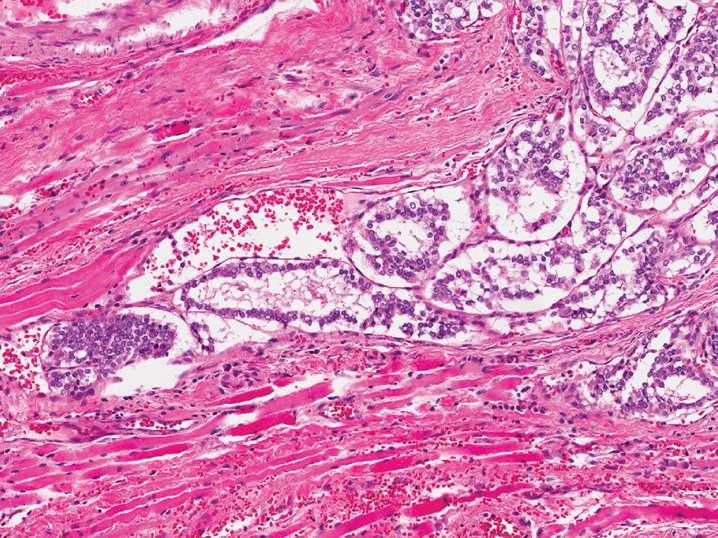
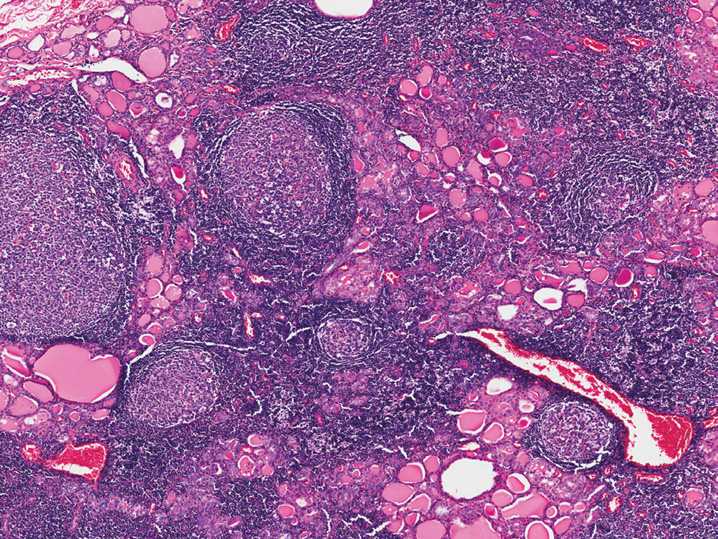
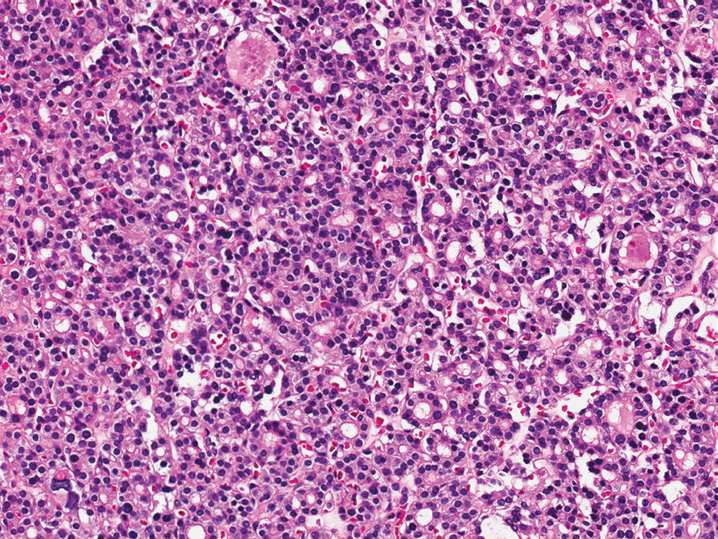
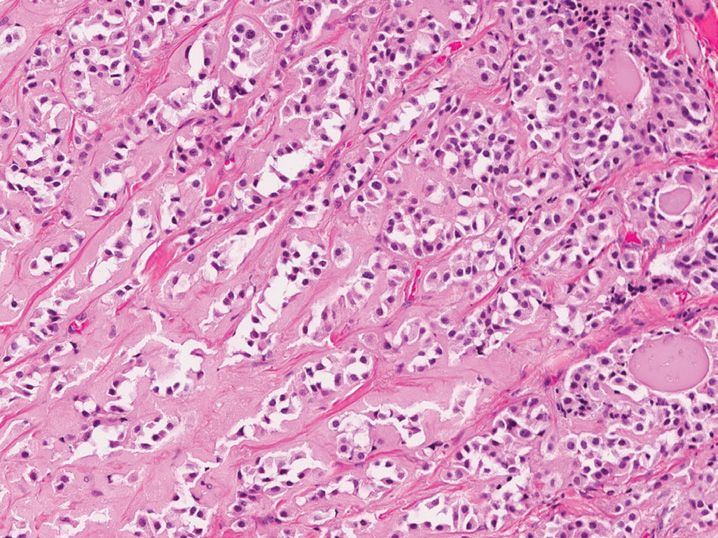
2. A 75-year-old man has a large pancreatic mass on imaging. No other lesions are identified in the chest or abdomen. A biopsy is performed (see Figure 11-2). The tumor has a high mitotic rate, with over 35 mitotic figures per 10 high-power fields. Immunohistochemical staining for synaptophysin and chromogranin are positive within the neoplastic cells. What is the best diagnosis for this lesion?
(A) Metastatic small cell undifferentiated carcinoma of the lung
(B) Pancreatic neuroendocrine carcinoma, large cell type
(C) Pancreatic neuroendocrine tumor, grade 1
(D) Pancreatic neuroendocrine tumor, grade 2
(E) Pancreatic neuroendocrine tumor, grade 3
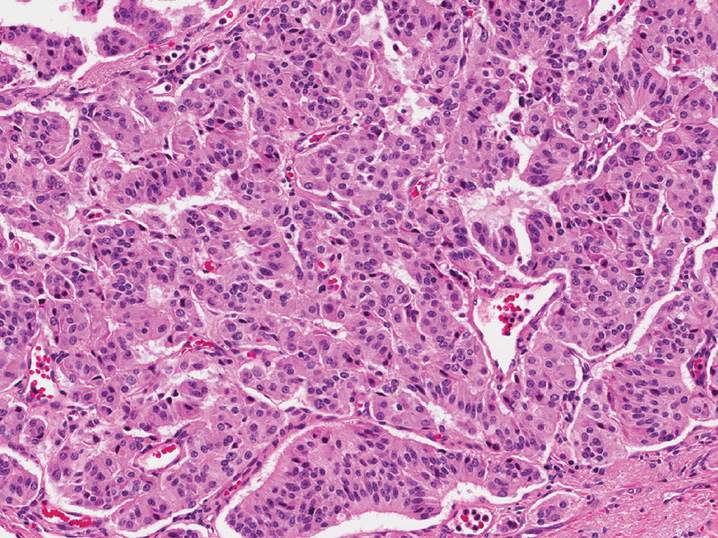
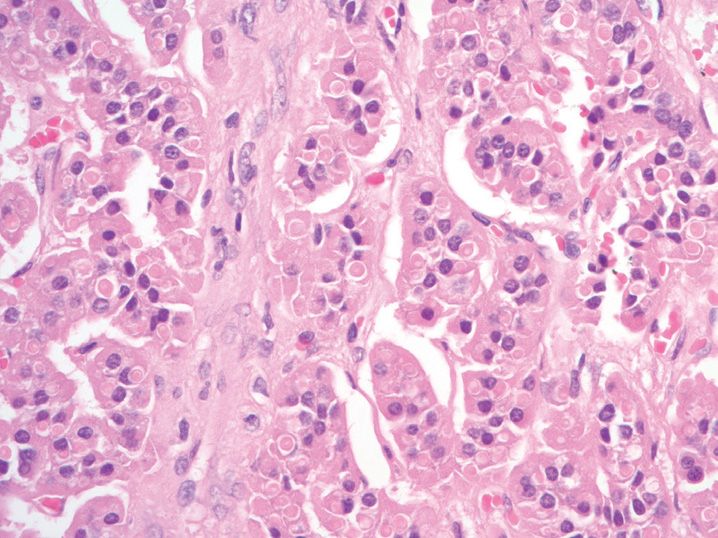
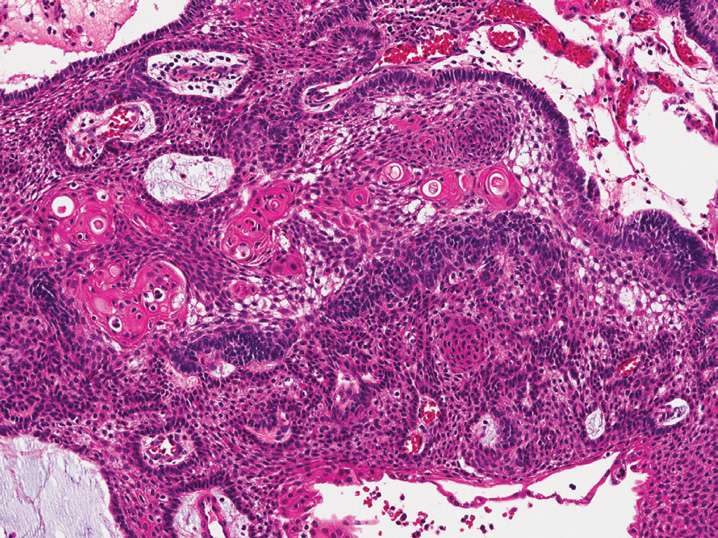
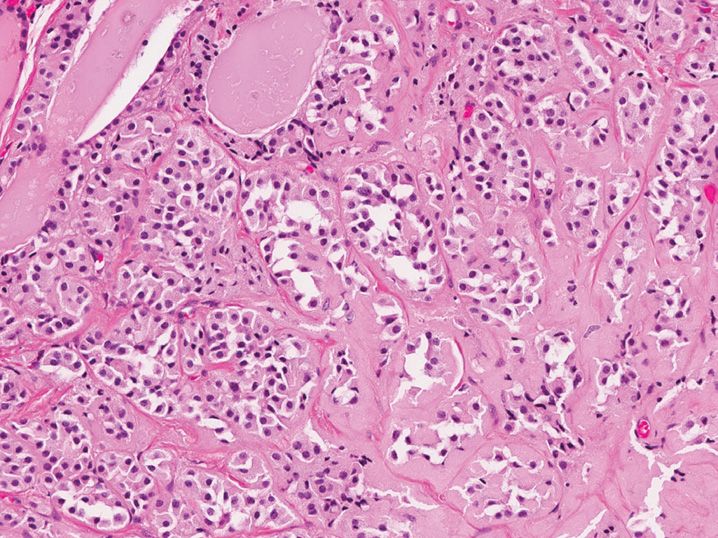
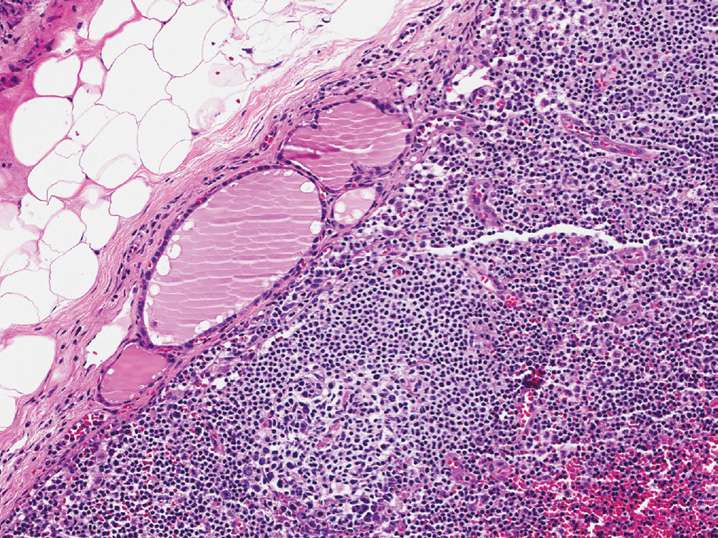
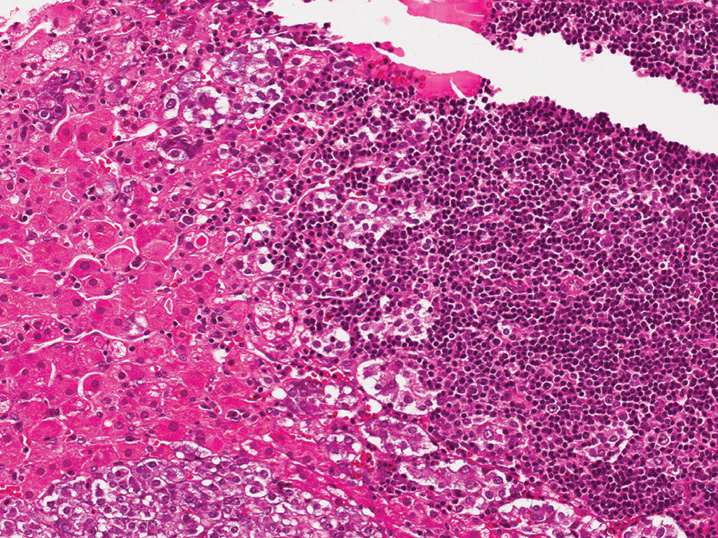
3. A 55-year-old man has a 3 cm pancreatic body mass that is biopsied (see Figure 11-3). All of the following immunohistochemical stains would be positive in this tumor except
(A) β-catenin (nuclear)
(B) CD56
(C) Chromogranin
(D) Cytokeratin
(E) Synaptophysin
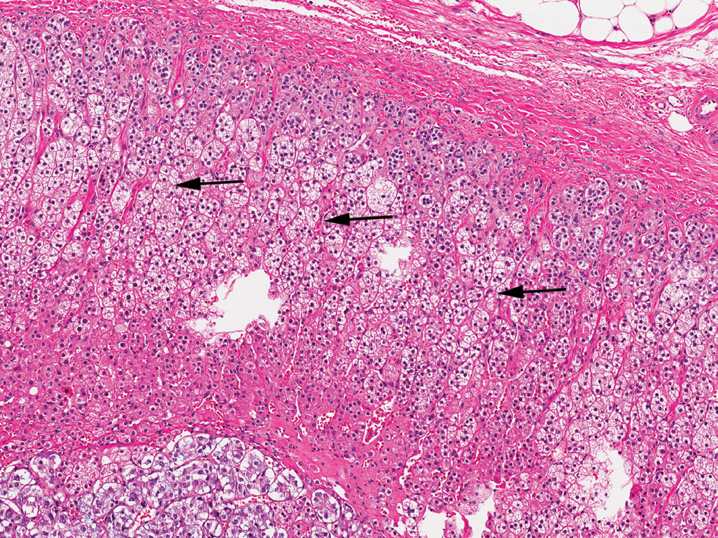
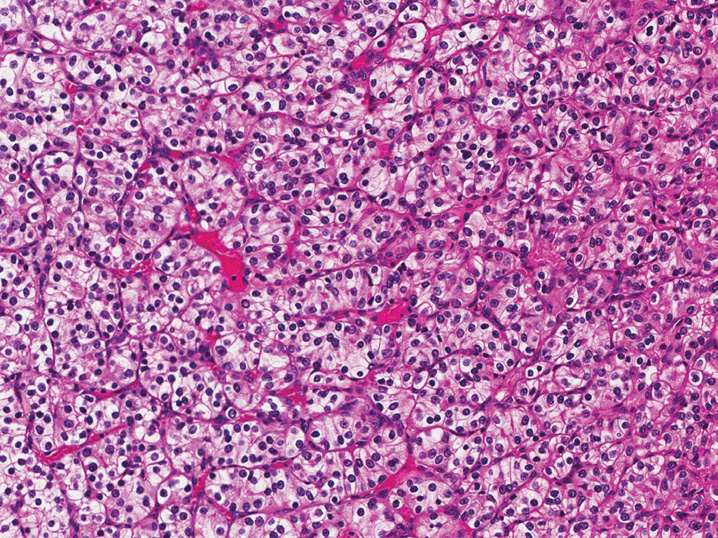
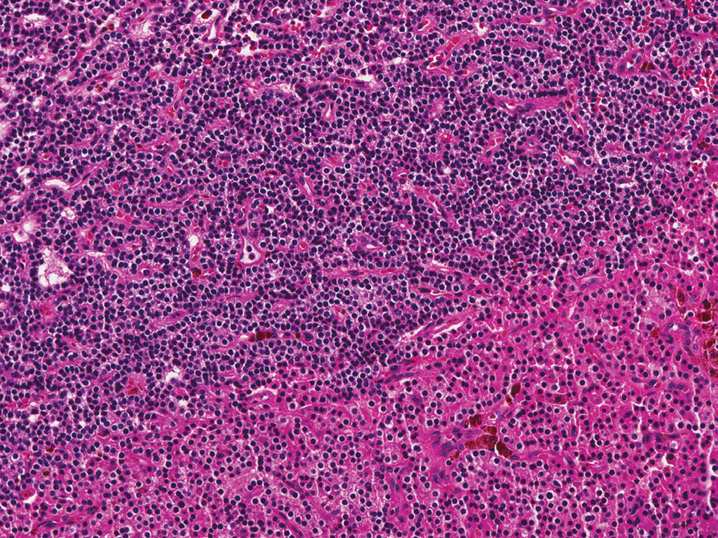
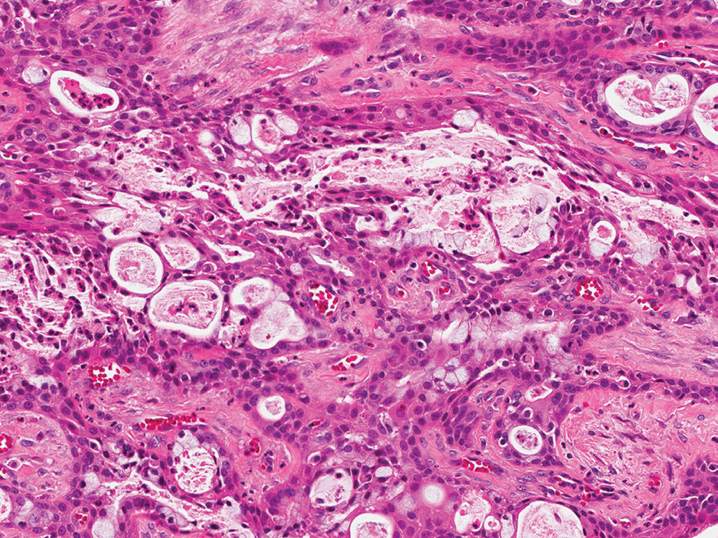
4. The photomicrograph demonstrates a section of normal adrenal gland. What is the main secretory product of the cells at the arrows (see Figure 11-4)?
(A) Aldosterone
(B) Cortisol
(C) Epinephrine
(D) Estrogen
(E) Testosterone
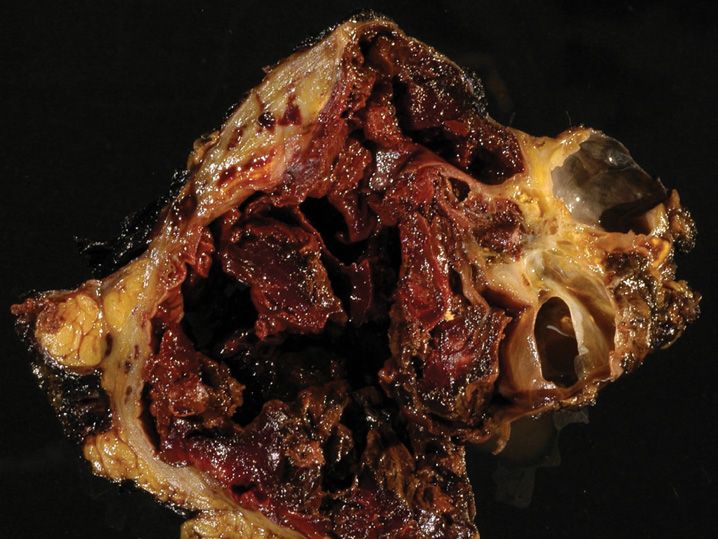
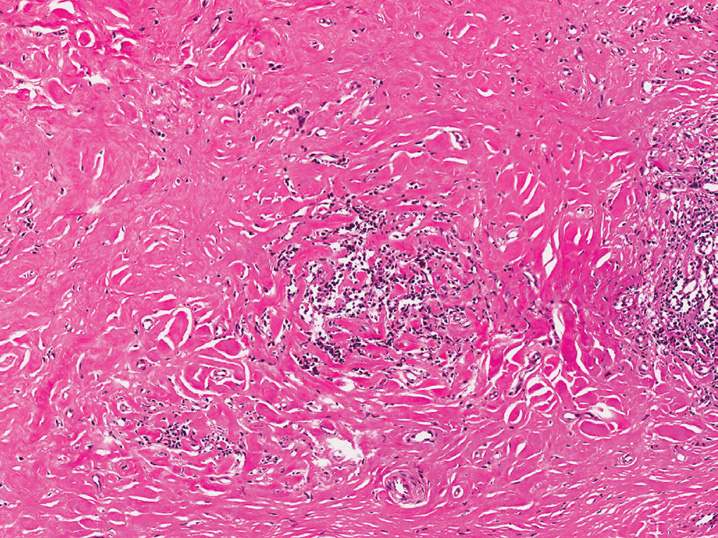
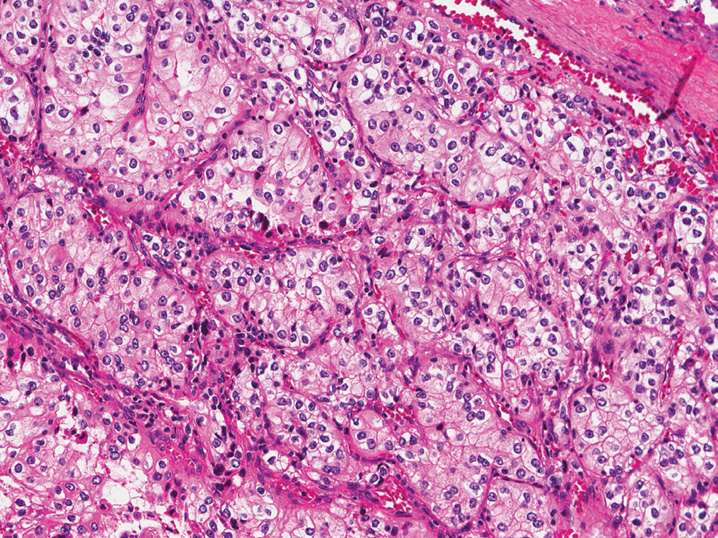
5. A 17-year-old high school student presents with severe neck pain, photophobia, fevers, and confusion. He is hospitalized with a presumptive diagnosis of bacterial meningitis. Several hours later, he develops severe hypotension and shock, along with purpura of the skin, and dies. At autopsy, his adrenals have the following appearance (see Figure 11-5). These findings are consistent with what clinical syndrome?
(A) Addison disease
(B) Beckwith–Wiedemann syndrome
(C) Cushing disease
(D) Cushing syndrome
(E) Waterhouse–Friderichsen syndrome
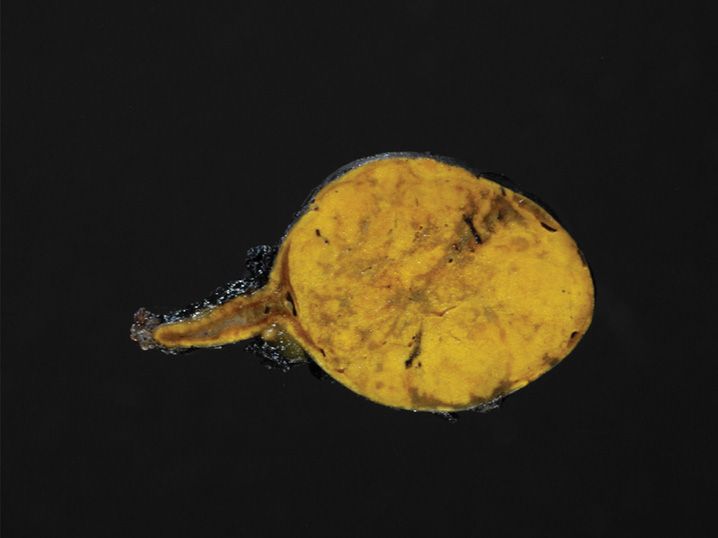
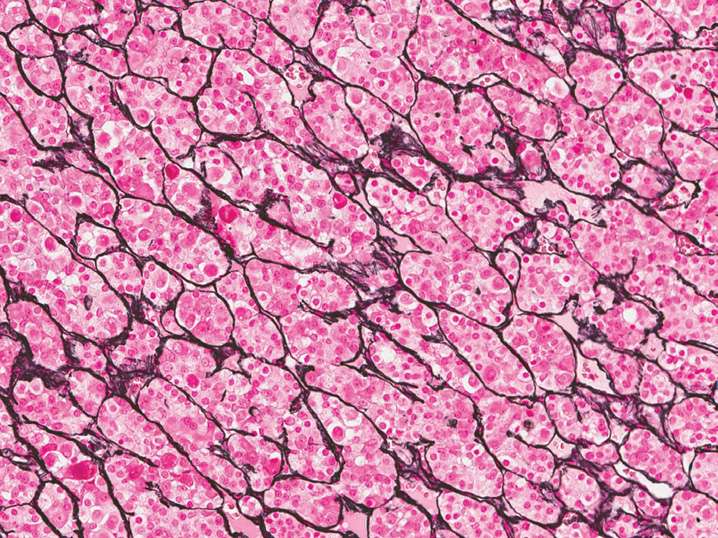
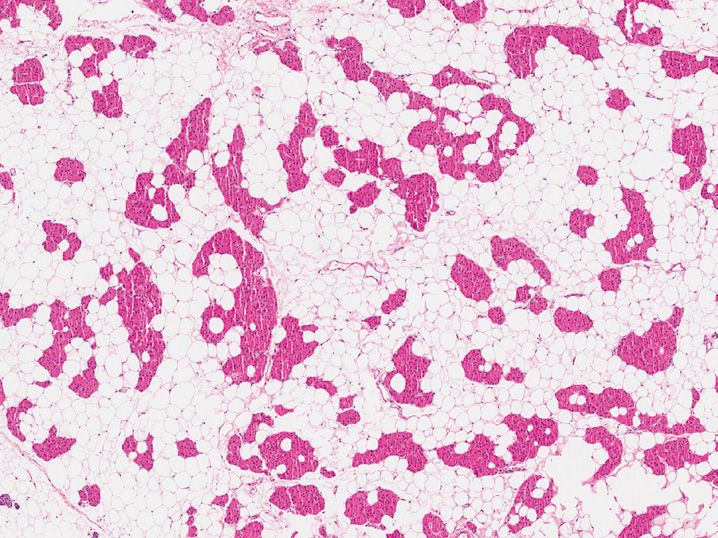
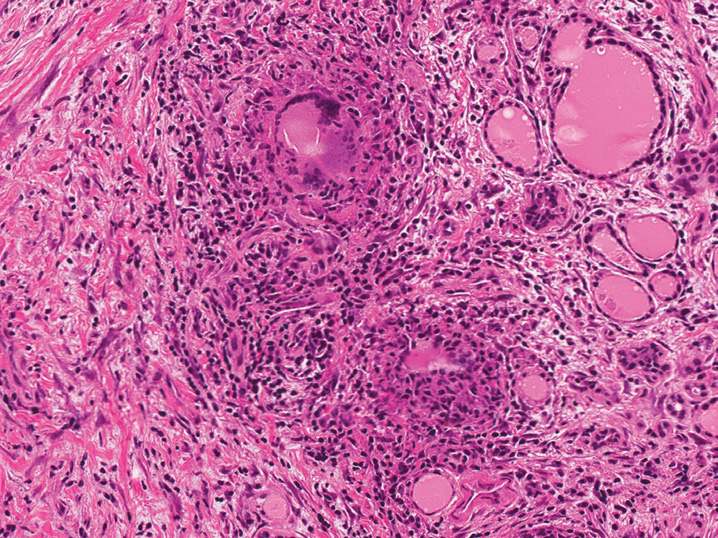
6. A 50-year-old woman has a computed tomography (CT) scan, and an incidental 4 cm unilateral adrenal mass is identified. Adrenalectomy is performed, and the mass has the following appearance (see Figure 11-6). What is the most likely diagnosis?
(A) Adrenal cortical adenoma
(B) Adrenal cortical carcinoma
(C) Angiomyolipoma
(D) Myelolipoma
(E) Pheochromocytoma
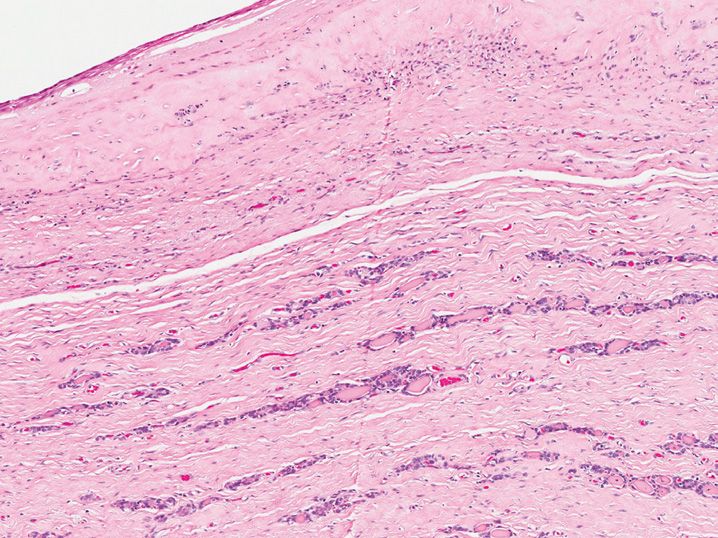
7. A 52-year-old man presents with progressive central obesity, skin striae, and a round face (“moon facies”). His adrenal gland has the following gross appearance (see Figure 11-7). What is the most likely cause of his symptoms?
(A) Adrenocorticotropic hormone (ACTH)-secreting pituitary adenoma
(B) Aldosterone-secreting adrenal cortical adenoma
(C) Cortisol-secreting adrenal cortical adenoma
(D) Pheochromocytoma
(E) Primary pigmented nodular adrenocortical disease
8. A 51-year-old man with medication-resistant hypertension and hypokalemia is found to have an adrenal mass. Excision of his adrenal gland demonstrates a well-circumscribed yellow-tan nodule arising from the adrenal cortex. Microscopic examination demonstrates round, eosinophilic inclusions with the cytoplasm of the neoplastic cells (see Figure 11-8). What medication was he most likely treated with prior to surgery?
(A) Angiotensin-converting enzyme inhibitor
(B) β-blockers
(C) Furosemide
(D) Prednisone
(E) Spironolactone
9. A 57-year-old woman presents with flank pain, and a 12 cm left adrenal mass is found. Adrenalectomy is performed (see Figure 11-9). Which of the following findings is not a predictor of malignancy in this tumor?
(A) Atypical mitotic figures
(B) Invasion of other anatomic structures (e.g., kidney)
(C) Mitotic rate >6 mitotic figures per 10 high-power fields
(D) Nuclear pleomorphism and hyperchromasia
(E) Vascular invasion
10. A 45-year-old man presents with hypertension and episodes of palpitations, headaches, and diaphoresis. An adrenal mass is discovered on imaging, and the resection has the following appearance (see Figure 11-10). All of the following statements are true regarding this lesion except
(A) 10% of patients will have bilateral tumors
(B) Associated with RET gene gain-of-function mutation
(C) Derived from the adrenal medulla
(D) Distant metastasis can occur late (>20 years after diagnosis)
(E) Vascular invasion is diagnostic of malignancy
11. A 14-year-old boy presents with double vision and headaches. CT scan demonstrates a suprasellar mass that is partially calcified. The lesion is removed, and has the following appearance (see Figure 11-11). What is the best diagnosis?
(A) Craniopharyngioma
(B) High-grade glioma
(C) Meningioma
(D) Metastatic squamous cell carcinoma
(E) Pituitary adenoma
12. A 32-year-old woman undergoes pituitary biopsy. A reticulin stain is performed on the biopsy specimen (see Figure 11-12). This reticulin staining pattern is most consistent with what diagnosis?
(A) Brain glial tissue
(B) Normal anterior pituitary
(C) Pituitary adenoma
(D) Pituitary infarction
(E) Posterior pituitary
13. A patient with elevated serum levels of parathyroid hormone is found to have four enlarged abnormal parathyroid glands at surgery, which have the following appearance (see Figure 11-13). All of the following processes are a possible cause of these changes except
(A) Chronic renal failure
(B) Lithium therapy
(C) Multiple endocrine neoplasia type 1
(D) Parathyroid carcinoma
(E) Vitamin D deficiency
14. A 60-year-old woman is diagnosed with primary hyperparathyroidism. At neck exploration, a 1.0 cm mass in the region of the right upper parathyroid is excised (see Figure 11-14). All of the following stains will be positive in this lesion except
(A) Chromogranin
(B) Cytokeratin
(C) Parathyroid hormone
(D) Periodic acid Schiff without diastase
(E) Renal cell carcinoma (RCC) antigen
15. A 53-year-old man presents with primary hyperparathyroidism. At surgery, a single abnormal appearing parathyroid gland is found, which weighs 2.5 g and measures 1.8 cm in greatest dimension. The other three parathyroid glands are normal in size and appearance. After excision, the intraoperative parathyroid hormone levels drop within the normal range. A portion of the abnormal parathyroid gland is submitted to pathology (see Figure 11-15). What is the best diagnosis for this lesion?
(A) Normal parathyroid gland
(B) Parathyroid adenoma
(C) Parathyroid hyperplasia
(D) Parathyroid lipoadenoma
(E) Water-clear cell hyperplasia
16. A 25-year-old woman presents with a midline cystic neck mass, which is excised (see Figure 11-16). All of the following statements are true regarding this lesion except
(A) Clinically moves upward with swallowing
(B) Contain C-cells that can undergo malignant transformation
(C) Papillary thyroid carcinoma is the most common malignancy to arise from this lesion
(D) Removal of the hyoid bone is necessary to prevent recurrence
(E) Thyroid tissue in the cyst wall is variable
17. An 18-year-old girl presents with heat intolerance, weight loss, sweating, and palpitations. Her thyroid gland is diffusely enlarged and undergoes excision, with the following appearance (see Figure 11-17). What is the underlying mechanism of her disease?
(A) Autonomously hyperfunctioning hyperplastic nodule
(B) Nonstimulating autoimmune antibodies against thyroid antigens
(C) Stimulating autoimmune antibodies against the thyroid-stimulating hormone (TSH) receptor
(D) T-cell mediated destruction of thyroid tissue
(E) Viral infection leading to excess thyroid hormone release
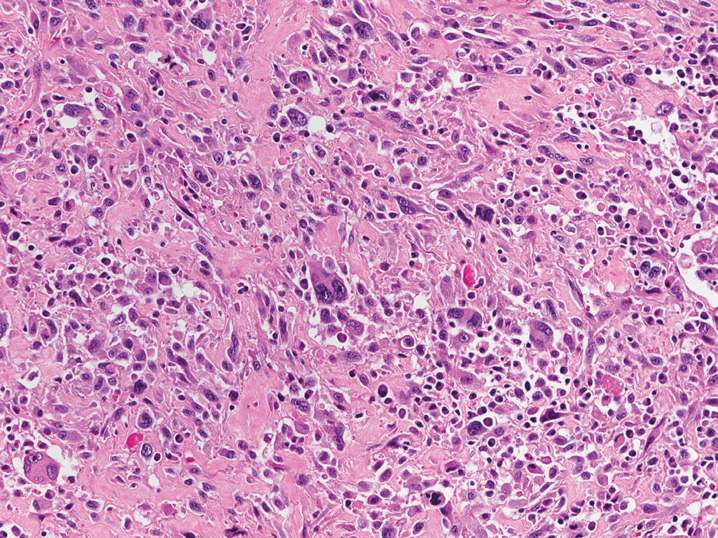
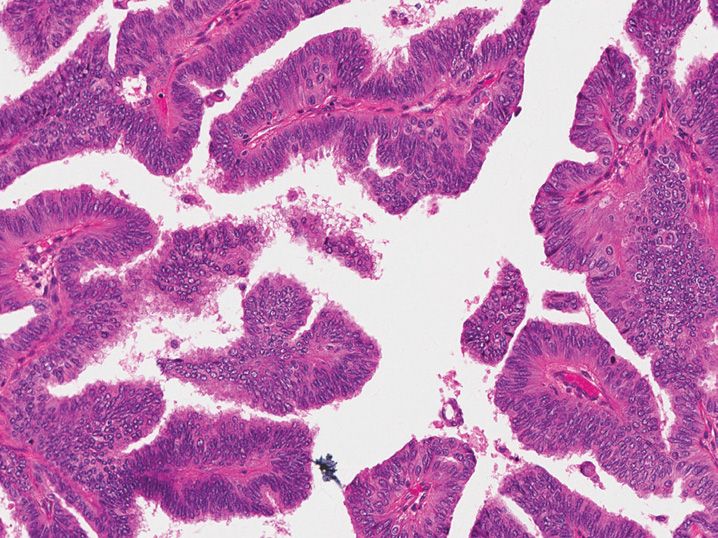
18. A 75-year-old man presents with hoarseness and a rapidly enlarging neck mass. Physical examination demonstrates an enlarged and firm thyroid gland. An incisional biopsy is performed (see Figure 11-18). Which of the following statements is true regarding this lesion?
(A) Immunohistochemical expression of thyroglobulin is present in over 90% of cases
(B) Locally aggressive tumor but rarely develops distant metastasis
(C) Median overall survival is 20 months
(D) Most commonly arises from a preexisting medullary thyroid carcinoma
(E) Tumors confined to the thyroid gland are staged as T4a disease
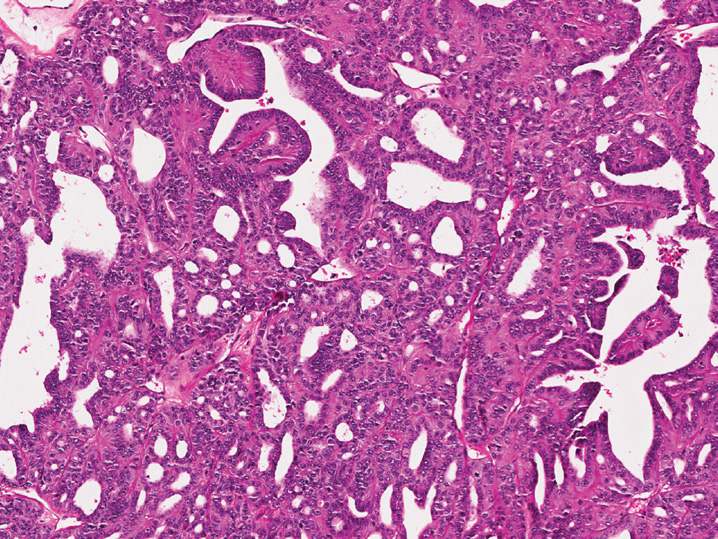
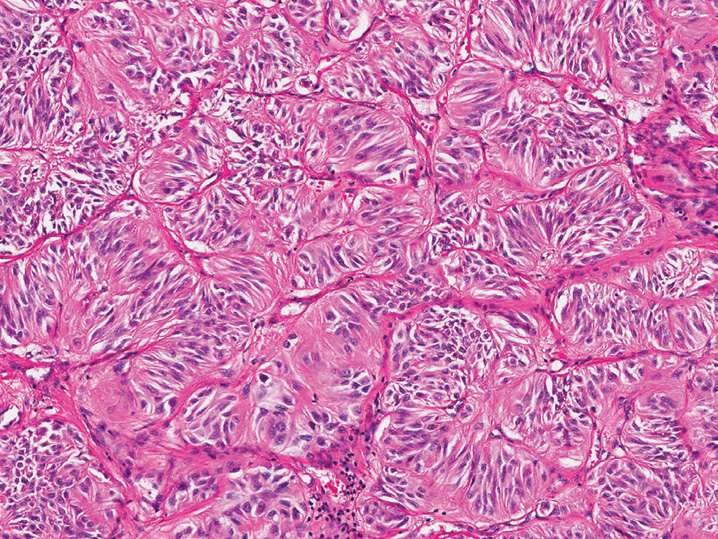
19. A 34-year-old woman undergoes thyroid resection for a thyroid nodule, which has the following appearance (see Figure 11-19). What genetic syndrome is this lesion associated with?
(A) Cowden syndrome (PTEN gene mutation)
(B) Familial adenomatosis polyposis (FAP)
(C) Hereditary nonpolyposis colorectal carcinoma (HNPCC) syndrome
(D) Multiple endocrine neoplasia type 1 (MEN 1)
(E) Multiple endocrine neoplasia type 2a (MEN 2a)
20. A 63-year-old woman has a 4.5 cm thyroid mass that is resected (see Figure 11-20). Examination of the capsule demonstrates lymphovascular space invasion. All of the following statements are true regarding this lesion except
(A) Abundant eosinophilic cytoplasm is composed of lysosomes
(B) Calcification of colloid can mimic psammoma bodies
(C) Criteria for malignancy are similar to conventional follicular carcinoma
(D) Immunohistochemical staining for thyroid transcription factor 1 (TTF-1) will be positive
(E) More commonly develops lymph node metastasis than conventional follicular carcinoma
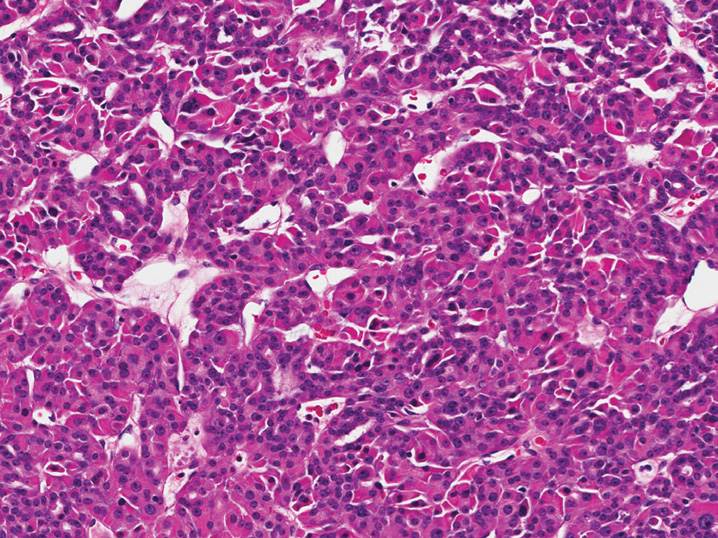
21. A 58-year-old man presents with a thyroid mass. At total thyroidectomy, a 3.5 cm poorly circumscribed mass involving the right thyroid lobe is identified (see Figure 11-21). What is the best diagnosis for this tumor?
(A) Follicular adenoma
(B) Follicular carcinoma
(C) Papillary thyroid carcinoma, solid variant
(D) Poorly differentiated thyroid carcinoma
(E) Undifferentiated (anaplastic) thyroid carcinoma
22. A 39-year-old woman with a thyroid nodule undergoes thyroid resection, and the operative note states the thyroid was easily removed without involvement of the thyroid cartilage or recurrent laryngeal nerve. A 1.2 cm papillary thyroid carcinoma is found at histopathologic examination, with the following finding (see Figure 11-22). What is the best tumor stage for this carcinoma?
(A) pT1a
(B) pT1b
(C) pT2
(E) pT4a
23. A thyroid mass has the following appearance (see Figure 11-23). Which of the following immunohistochemical stains will not be positive in the neoplastic cells?
(A) Calcitonin
(B) Carcinoembryonic antigen (CEA)
(C) Cytokeratin
(D) Thyroglobulin
(E) TTF-1
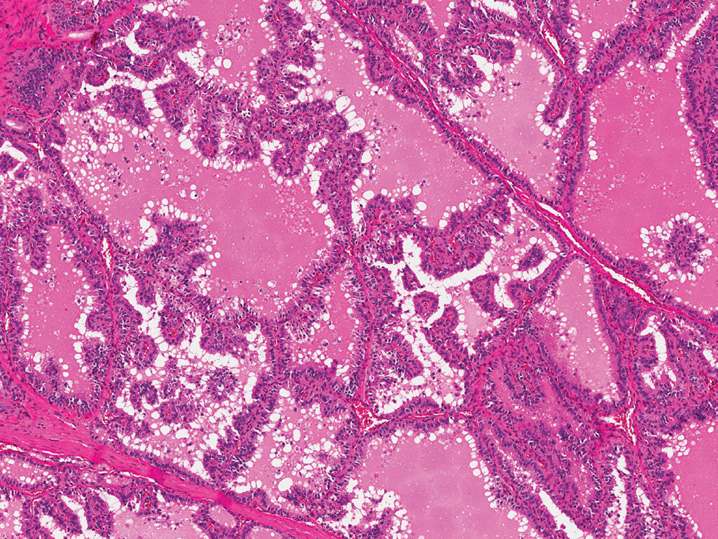
24. A 59-year-old man presents with a 5.0 cm thyroid mass. Total thyroidectomy is performed (see Figure 11-24). What is the best diagnosis?
(A) Medullary thyroid carcinoma
(B) Metastatic endometrioid adenocarcinoma
(C) Columnar cell variant of papillary thyroid carcinoma
(D) Cribriform-morular variant of papillary thyroid carcinoma
(E) Poorly differentiated thyroid carcinoma
25. A 45-year-old woman has a thyroid gland excised for a solitary well-circumscribed 1.5 cm nodule that has the following appearance (see Figure 11-25). No capsular or vascular invasion is identified. Immunohistochemical staining for thyroglobulin is positive. What is the best diagnosis for this lesion?
(A) Follicular adenoma
(B) Follicular carcinoma
(C) Hyalinizing trabecular tumor
(D) Medullary thyroid carcinoma
(E) Tall cell variant of papillary thyroid carcinoma
26. A 62-year-old woman presents with hypothyroidism. Physical exam demonstrates an enlarged, hard, fixed thyroid gland. At the time of surgery, the process involving the thyroid gland extends into the surrounding strap muscles and perithyroidal fat, so only an incisional biopsy is performed (see Figure 11-26). What is the best diagnosis for this process?
(A) Anaplastic thyroid carcinoma
(B) Graves disease
(C) Hashimoto thyroiditis
(D) Diffuse sclerosing variant of papillary thyroid carcinoma
(E) Riedel’s disease
27. A 51-year-old woman presents with a painful neck mass, palpitations, weight loss, and heat intolerance. Clinical exam demonstrates a diffusely enlarged and tender thyroid gland. A biopsy is performed (see Figure 11-27). What is the best diagnosis?
(A) Chronic lymphocytic thyroiditis
(B) Graves disease
(C) Palpation thyroiditis
(D) Sarcoidosis
(E) Subacute thyroiditis
28. A 41-year-old woman has hypothyroidism. A biopsy of her thyroid gland is shown in Figure 11-28. All of the following statements are true regarding this process except
(A) Associated with antithyroglobulin antibodies
(B) More common in men than women
(C) Oncocytic (Hürthle cell) metaplasia of follicular epithelium is characteristic
(D) Patients with this disorder have an increased risk of other autoimmune diseases
(E) This disease is a risk factor for the development of papillary thyroid carcinoma
29. A 55-year-old man undergoes radical neck dissection for squamous cell carcinoma of the tonsil. A lymph node from the right lateral level 4 shows the following finding (see Figure 11-29). What is most likely explanation for this finding?
(A) Embryonic remnant of thyroid tissue within lymph node capsule
(B) Iatrogenic disruption of normal thyroid tissue with lymph node embolization
(C) Normal lymph node with prominent vascular structures in the hilum
(D) Occult papillary thyroid carcinoma with lymph node metastasis
(E) Squamous cell carcinoma metastasis with variant morphology
30. A 47-year-old man undergoes thyroid lobectomy for a thyroid nodule. Upon gross evaluation, a single 3.5 cm nodule with a thick fibrous capsule is present in the thyroid lobe, and a frozen section has the following appearance (see Figure 11-30). How should sections be taken to exclude malignancy?
(A) No additional sections are needed; the frozen section is diagnostic
(B) Submit representative sections of the nodule in relationship to adjacent thyroid tissue
(C) Submit representative sections of the nodule in relationship to the margins of resection
(D) Submit the entire fibrous capsule of the nodule and random sections of uninvolved thyroid tissue
(E) Submit two random sections of nodule and the remaining uninvolved thyroid gland
31. A 19-year-old man presents with a thyroid mass. At resection, the tumor is composed of densely packed bland spindle cells that merge with gland-like structures, and are positive for cytokeratin and negative for thyroglobulin, TTF-1, and calcitonin. What is the most likely diagnosis?
(A) Carcinoma showing thymus-like differentiation (CASTLE)
(B) Papillary thyroid carcinoma, solid variant
(C) Poorly differentiated thyroid carcinoma
(D) Spindle epithelial tumor with thymus-like differentiation (SETTLE)
(E) Undifferentiated (anaplastic) thyroid carcinoma
32. A 37-year-old woman with acne undergoes thyroid resection. The thyroid cut surface is diffusely black in color. What medication was she taking?
(A) Clindamycin
(B) Isotretinoin
(C) Minocycline
(D) Oral contraceptives
(E) Salicylic acid
33. A 62-year-old man presents with diarrhea and severe peptic ulcer disease. His symptoms do not improve despite maximal medical therapy. A pancreatic tumor is found on imaging. What is the most likely hormone to be produced by this tumor?
(A) Gastrin
(B) Glucagon
(C) Insulin
(D) Somatostatin
(E) Vasoactive intestinal peptide
34. At autopsy, examination of the pancreas demonstrates diffuse islet cell hyperplasia. Which of the following clinical scenarios is a likely cause of this finding?
(A) A 1-week-old baby girl exposed to uncontrolled maternal diabetes
(B) A 14-year-old girl with new diagnosis of type 1 diabetes
(C) A 48-year-old woman with an insulin-secreting pancreatic endocrine neoplasm
(D) A 53-year-old obese woman with a new diagnosis of type 2 diabetes
(E) A 72-year-old woman on a short steroid taper for rheumatoid arthritis
35. A 13-year-old girl is diagnosed with type 1 diabetes. Histologic examination of her pancreas would show what pathologic change?
(A) Acinar atrophy and fibrosis
(B) Amyloid deposition within the islets
(C) Dystrophic calcification and fat necrosis
(D) Increased number of islets
(E) Infiltration of islet cells by T-lymphocytes
36. In an experimental mouse model, a researcher is able to selectively destroy all of the α-cells within the pancreatic islet cells, but leaves all other cell types intact. What hormone will this mouse be unable to produce?
(A) Glucagon
(B) Insulin
(C) Pancreatic polypeptide
(D) Somatostatin
(E) Vasoactive intestinal polypeptide
37. A 75-year-old man undergoes a distal pancreatectomy for a pancreatic neuroendocrine tumor. All of the following pathologic features would favor an excellent prognosis except
(A) Confined to the pancreas
(B) Ki-67 proliferative index of 3%
(C) Mitotic rate of 1 mitotic figure per high-power field
(D) No angiolymphatic invasion
(E) Size 1.8 cm
38. A newborn baby has ambiguous genitalia, and within 2 weeks develops dehydration, hyponatremia, hyperkalemia, and vomiting. Ultrasound shows enlarged adrenal glands bilaterally. What is the most common cause of this syndrome?
(A) 17-alpha-hydroxylase deficiency
(B) Autoimmune adrenalitis
(C) Cushing disease
(D) 21-hydroxylase deficiency
(E) X-linked congenital adrenal hypoplasia
39. A 74-year-old man with clear cell renal cell carcinoma has a nodule is present in the ipsilateral adrenal gland composed of cells with abundant clear cytoplasm. Which of the following immunohisto-chemical stains, if positive, would favor a diagnosis of adrenal cortical adenoma?
(A) Calretinin
(B) Chromogranin
(C) Cytokeratin 7
(D) HMB-45
(E) Renal cell carcinoma (RCC) antigen
40. A 47-year-old man presents with slowly progressive fatigue, weakness, and skin hyperpigmentation. Serologic studies show low levels of cortisol and aldosterone, which do not increase when exogenous adrenocorticotropic hormone (ACTH) is administered. All of the following are possible causes of this disease except
(A) Acquired immunodeficiency syndrome (AIDS)
(B) Autoimmune adrenalitis
(C) Disseminated tuberculosis infection
(D) Metastasis to the adrenal glands
(E) Pituitary infarction
41. Pheochromocytomas are highly associated with all of the following syndromes except
(A) Hereditary paraganglioma-pheochromocytoma syndrome
(B) Multiple endocrine neoplasia 1 (MEN 1)
(C) Multiple endocrine neoplasia 2a (MEN 2a)
(D) Multiple endocrine neoplasia 2b (MEN 2b)
(E) von Hippel–Lindau disease (VHL)
42. A 42-year-old woman is diagnosed with an adrenal cortical adenoma. All of the following statements are true regarding adrenal cortical adenomas except
(A) Are grossly well circumscribed with a smooth border
(B) If hyperfunctional, most commonly produce aldosterone
(C) Incidentally discovered adenomas are usually not hyperfunctional
(D) Typically weigh <100 g
(E) Virilization or feminization is a good prognostic sign
43. A cross section of a large adrenal mass is soaked in a potassium dichromate solution, and turns a dark blue-black color. This color change favors what diagnosis?
(A) Adrenal cortical adenoma
(B) Adrenal cortical carcinoma
(C) Metastatic melanoma
(D) Pheochromocytoma
(E) Tuberculosis infection
44. Which of the following hormones is released from the posterior pituitary?
(A) Adrenocorticotropic hormone (ACTH)
(B) Antidiuretic hormone (ADH)
(C) Corticotropin-releasing hormone (CRH)
(D) Growth hormone (GH)
(E) Thyroid stimulating hormone (TSH)
45. A 32-year-old woman presents with amenorrhea and bilateral white breast discharge. No breast lesions are palpated, and a pregnancy test is negative. What is the most likely finding on an MRI scan of the brain?
(A) An empty sella turcica
(B) Glioblastoma
(C) Pituitary macroadenoma
(D) Pituitary microadenoma
(E) Subarachnoid hemorrhage
46. A patient on glucocorticoids for multiple medical problems dies in the intensive care unit. An autopsy is performed, and examination of the otherwise normal pituitary shows scattered cells containing a ring of cytoplasmic pale-pink amorphous material around the nucleus, which is positive for low molecular weight cytokeratin immunohistochemical stain. What hormone would these cells normally secrete?
(A) Adrenocorticotropic hormone (ACTH)
(B) Growth hormone (GH)
(C) Luteinizing hormone (LH)
(D) Prolactin (PRL)
(E) Thyroid stimulating hormone (TSH)
47. A 37-year-old pregnant woman goes through a difficult home labor and delivery, which results in significant postpartum hemorrhage. Two weeks later, she calls her midwife about problems breastfeeding, and reports that her breast milk still has not “come in.” What is the most likely cause of her inability to breastfeed?
(A) Cushing syndrome
(B) Poor hydration
(C) Prior breast surgery
(D) Prolactin-secreting pituitary adenoma
(E) Sheehan syndrome
48. A 55-year old man is found to have a pituitary adenoma. Serologic studies show elevated levels of insulin-like growth factor 1 (IGF-1). What clinical symptoms did he most likely present with?
(A) Bilateral galactorrhea
(B) Changing facial features and large hands with sausage-like fingers
(C) Erectile dysfunction and fatigue
(D) Obesity and abdominal striae
(E) Very tall with disproportionately long arms and legs
49. A diagnosis of pituitary carcinoma requires which of the following findings?
(A) Direct invasion of bone or brain
(B) Discontinuous subarachnoid space deposits
(C) >10 mitotic figures per 10 high-power fields
(D) Marked nuclear pleomorphism
(E) Tumor necrosis
50. All of the following are features of an atypical pituitary adenoma except
(A) Diffuse nuclear staining for p53
(B) Increased mitotic activity
(C) Ki-67 index of >3%
(D) Microscopic bone invasion
(E) Microscopic dura invasion
51. A 52-year-old woman presents with a lytic lesion of the jaw, which on biopsy shows bone resorption and replacement by fibrous tissue and osteoclast-like giant cells. She also has recently been diagnosed with kidney stones and osteopenia. A serum calcium level is 12.4 mg/dL. What is the most likely cause of her symptoms?
(A) Four gland parathyroid hyperplasia
(B) Hypoparathyroidism
(C) Osteomalacia (vitamin D deficiency)
(D) Parathyroid adenoma
(E) Renal failure
52. A newborn baby girl with congenital heart disease develops convulsions and tetany shortly after birth. A serum calcium level is low. Chest x-ray shows an absent thymus gland. What is the most likely cause of her clinical findings?
(A) DiGeorge syndrome
(B) Down syndrome
(C) Iatrogenic hypoparathyroidism
(D) Multiple endocrine neoplasia type 1
(E) X-linked familial hypoparathyroidism
53. A patient with hypercalcemia undergoes a neck exploration, and a parathyroid gland is excised. Which of the following features would favor a solitary adenoma over multiple gland hyperplasia?
(A) All four glands appear abnormal
(B) Circumscribed hypercellular nodule with a rim of atrophic parathyroid tissue
(C) Gland weight over 0.5 g
(D) Oil red O staining shows reduced intracellular fat
(E) Recurrent hyperparathyroidism within 2 years
54. A 52-year-old woman presents with severe hyperparathyroidism, and a calcium of 14.8 mg/dL. In the operating room, the surgeon identifies a single, enlarged parathyroid gland that is difficult to excise. Which of the following histopathologic findings would support a diagnosis of parathyroid carcinoma?
(A) Diffuse or solid growth pattern
(B) Fibrosis
(C) Increased mitotic activity
(D) Immunohistochemical staining with parafibromin
(E) Vascular space invasion
55. A 45-year-old woman is undergoing parathyroid exploration for primary hyperparathyroidism. A biopsy is submitted for frozen section evaluation, and the surgeon is uncertain whether the tissue represents abnormal parathyroid gland tissue or a portion of thyroid parenchyma. Which of the following findings would only be seen in thyroid tissue?
(A) Interspersed fibroadipose tissue
(B) Microfollicular architecture
(C) Oxalate crystals
(D) Rim of normal parathyroid gland
(E) Two cell types (oxyphil and chief cell)
56. A 32-year-old woman with severe hypothyroidism is pregnant. What disorder is her fetus at risk for developing if she is not treated?
(A) Congenital heart disease
(B) Limb defects
(C) Neural tube defects
(D) Renal agenesis
(E) Severe mental retardation
57. A 42-year-old woman presents with fatigue, weight gain, cold intolerance, and loss of appetite. Serum laboratory testing demonstrates low T3 and T4 levels, and an elevation in thyroid stimulating hormone (TSH). All of the following are potential causes of these findings except
(A) Chronic lymphocytic thyroiditis
(B) History of radiation therapy to the neck
(C) Iodine deficiency
(D) Pituitary infarction
(E) Total thyroidectomy
58. All of the following statements regarding diffuse sclerosing variant of papillary thyroid carcinoma are true except
(A) Approximately 20% of patients will have lymph node metastasis at diagnosis
(B) Associated with severe chronic lymphocytic thyroiditis
(C) Excellent long-term prognosis despite aggressive behavior
(D) Most common in young adults
(E) Requires diffuse involvement of at least one thyroid lobe by carcinoma
59. All of the following histologic changes can be seen in a thyroid nodule after a previous fine-needle aspiration biopsy except
(A) Artifactual displacement or implantation of tumor with vascular lumens
(B) Complete infarction of the thyroid nodule
(C) Irregular capsular contour suggestive of capsular invasion (capsular pseudoinvasion)
(D) Nuclear enlargement, chromatin clearing, and nuclear pseudoinclusions
(E) Proliferation of bland spindle cells with abundant mitotic figures (postoperative spindle cell nodule)
60. What is the most common primary malignant neoplasm of the thyroid gland in countries with adequate dietary iodine?
(A) Follicular adenoma
(B) Follicular carcinoma
(C) Medullary thyroid carcinoma
(D) Papillary thyroid carcinoma
(E) Primary thyroid lymphoma
61. What is the most common molecular alteration found in tall cell variant of papillary thyroid carcinoma?
(A) BRAF point mutation
(B) PAX8/PPAR-γ translocation
(C) RAS point mutation
(D) RET point mutation
(E) RET/PTC translocation
62. A minimally invasive follicular carcinoma is defined as having which of the following features?
(A) Invasion into adjacent normal thyroid parenchyma
(B) Invasion into large caliber vessels
(C) Invasion into less than one-third of the tumor capsule
(D) Invasion into perithyroidal structures
(E) Invasion into small caliber vessels within the tumor capsule
63. All of the following are features of poorly differentiated thyroid carcinomas except
(A) Classic nuclear features of papillary thyroid carcinoma
(B) Convoluted nuclei
(C) Increased mitotic activity (3 or more mitotic figures per 10 high-power fields)
(D) Solid or insular growth pattern
(E) Tumor necrosis
64. A 54-year-old woman presents with a diffusely enlarged and firm thyroid gland. She has a history of chronic lymphocytic thyroiditis, and the surgeon is concerned for a primary thyroid lymphoma. Which of the following pathologic features, if present, would favor a diagnosis of malignant lymphoma over chronic lymphocytic thyroiditis?
(A) Lymphoepithelial lesions involving thyroid epithelium
(B) Polytypic B-cells lacking kappa or lambda light chain restriction
(C) Preserved architecture of the thyroid gland
(D) Prominent germinal centers containing tingible body macrophages.
(E) Sharp borders between lymphoid infiltrates and perithyroidal soft tissue
65. All of the following nuclear changes are typically seen in papillary thyroid carcinoma except
(A) Fine chromatin
(B) Grooves
(C) Macronucleoli
(D) Nuclear enlargement
(E) Pseudoinclusions
66. Examination of a thyroid gland demonstrates an increase in C-cells. All of the following statements are true regarding nodular (neoplastic) C-cell hyperplasia except
(A) Associated with multiple endocrine neoplasia 2 (MEN 2)
(B) C-cells must remain confined within the basement membrane of thyroid follicles
(C) Defined as nodular foci of C-cells filling or partially destroying thyroid follicles, usually over 50 cells
(D) Requires immunohistochemistry with calcitonin for identification in most cases
(E) RET gene mutations can be demonstrated in these cells
67. A 31-year-old woman is diagnosed with adrenocortical insufficiency, and if biopsied, her adrenal gland would likely show changes of autoimmune adrenalitis (see Figure 11-31). She notices patchy increased skin pigmentation around her knuckles and elbows. What is the cause of her skin hyperpigmentation?
(A) Excess aldosterone production
(B) Excess melanocyte-simulating hormone
(C) Hemochromatosis
(D) Malignant melanoma
(E) Melasma
68. A 61-year-old woman presents with a cold thyroid nodule. A resection is performed (see Figure 11-32). All of the following statements are true regarding this lesion except
(A) Histologically indistinguishable from similar tumor of salivary glands
(B) Immunohistochemical staining for thyroglobulin is focally positive in the nonsclerosing type
(C) Likely derived from salivary gland inclusions within the thyroid gland
(D) Mucicarmine stain is positive in the goblet cell component
(E) The sclerosing variant with eosinophilia is associated with chronic lymphocytic thyroiditis
69. A 71-year-old man undergoes PET scan during follow-up for a diagnosis of renal cell carcinoma 12 years ago, and a thyroid mass is identified. He undergoes thyroid lobectomy, which contains a well-circumscribed nodule with the following appearance (see Figure 11-33). What is the most helpful feature in differentiating a primary thyroid neoplasm from metastatic renal cell carcinoma?
(A) Absence of colloid
(B) Absence of thyroglobulin staining
(C) Clear cytoplasm
(D) Papillary structures
(E) Solitary well-circumscribed nodule
70. A 23-year-old man presents with a thyroid mass. At total thyroidectomy, a 3.5 cm mass is found with the following appearance (see Figure 11-34). What genetic mutation is most likely present in the tumor cells?
(A) BRAF point mutation
(B) RAS point mutation
(C) RET activating point mutation
(D) RET inactivating point mutation
(E) RET/PTC translocation
71. A 42-year-old woman presents with episodes of confusion and loss of consciousness, which are precipitated by exercise. Drinking orange juice results in immediate improvement. A blood glucose level during one of these episodes is 38 mg/dL, along with elevated C-peptide levels. What is the most likely cause of her fainting spells?
(A) Diabetes mellitus type 1
(B) Diffuse hyperplasia of the islets of the pancreas
(C) Factitious hypoglycemia
(D) Glucagon-secreting pancreatic endocrine neoplasm
(E) Insulin-secreting pancreatic endocrine neoplasm
72. All of the following are features of a pancreatic neuroendocrine microadenoma except
(A) Associated with multiple endocrine neoplasia type 1 when multiple microadenomas are present
(B) Clinically functional, most commonly causing hyperinsulinemia
(C) Immunohistochemical staining restricted to one or two pancreatic hormones
(D) Low mitotic rate (<10 mitotic figures per 10 high-power fields)
(E) Size <0.5 cm
73. The most common neoplasm responsible for an adrenal mass is
(A) Adrenal cortical adenoma
(B) Adrenal cortical carcinoma
(C) Metastatic carcinoma
(D) Myelolipoma
(E) Pheochromocytoma
74. The anterior pituitary is derived from what embryologic structure?
(A) First branchial arch
(B) Neural tube
(C) Notochord
(D) Rathke’s pouch
(E) Second branchial cleft
75. What two anterior pituitary hormones would a mammosomatotroph cell pituitary adenoma express?
(A) Adrenocorticotropic hormone and growth hormone
(B) Adrenocorticotropic hormone and prolactin
(C) Follicle stimulating hormone and thyroid stimulating hormone
(D) Growth hormone and prolactin
(E) Prolactin and thyroid stimulating hormone
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree