15 Endocrine disease
Pituitary disorders
Pituitary tumours
Treatment
Treatment (Table 15.1) options include surgery, radiotherapy and medical therapy, depending on the aetiology of the pituitary mass. Post-operative radiotherapy is used if significant tumour bulk remains after surgery or the underlying disease is still active. Radiotherapy results in a gradual decline of residual pituitary function over many years and must be monitored.
Table 15.1 Comparison of primary treatment for pituitary tumours
| Treatment method | Advantages | Disadvantages |
|---|---|---|
| Surgical | ||
| Trans-sphenoidal adenomectomy or hypophysectomy | Relatively minor procedure Potentially curative for micro- and smaller macro-adenomas | Some extrasellar extensions may not be accessible Risk of CSF leakage and meningitis |
| Trans-frontal | Good access to suprasellar region | Major procedure; danger of frontal lobe damage High chance of subsequent hypopituitarism |
| Radiotherapy | ||
| External (40–50 Gy) | Non-invasive Reduces recurrence rate after surgery | Slow action, often over many years Not always effective Possible late risk of tumour induction |
| Stereotactic | Precise administration of dose to lesion | Long-term follow-up data limited |
| Yttrium implantation | High local dose | Only used in few centres |
| Medical | ||
| Dopamine agonist (e.g. bromocriptine) | Non-invasive; reversible | Usually not curative; significant side-effects in minority |
| Somatostatin analogue (octreotide) | Non-invasive; reversible | Usually not curative; expensive |
| Growth hormone receptor antagonist (pegvisomant) | Highly selective | Usually not curative; very expensive |
Hypopituitarism
Clinical features
Secondary hypothyroidism (p. 571) and adrenal failure (p. 582) both lead to tiredness and general malaise:
Examination
Investigation of pituitary function
• Basal serum investigations
• Dynamic tests
Management
Options for hormone replacement regimes are given in Table 15.2.
Table 15.2 Replacement therapy for hypopituitarism
| Axis | Usual replacement therapies |
|---|---|
| Adrenal | Hydrocortisone 15–40 mg daily (starting dose 10 mg on rising/5 mg lunchtime/5 mg evening) (Normally no need for mineralocorticoid replacement) |
| Thyroid | Levothyroxine 100–150 mcg daily |
| Gonadal | |
| Male | Testosterone IM, orally, transdermally or implant |
| Female | Cyclical oestrogen/progestogen orally or as patch |
| Fertility | HCG plus FSH (purified or recombinant) or pulsatile GnRH to produce testicular development, spermatogenesis or ovulation |
| Growth | Recombinant human growth hormone used routinely to achieve normal growth in children Also advocated for replacement therapy in adults where growth hormone has effects on muscle mass and well-being |
| Thirst | Desmopressin 10–20 mcg 1–3 times daily by nasal spray or orally 100–200 mcg 3 times daily Carbamazepine, thiazides and chlorpropamide are very occasionally used in mild diabetes insipidus |
| Breast (prolactin inhibition) | Dopamine agonist (e.g. cabergoline 500 mcg weekly) |
FSH, follicle-stimulating hormone; GnRH, gonadotrophin-releasing hormone; HCG, human chorionic gonadotrophin.
Thyroid disorders
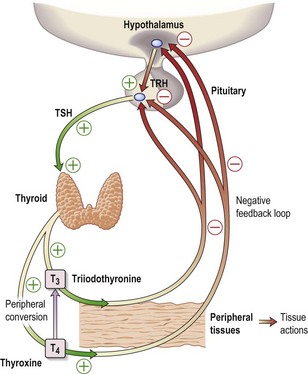
The thyroid hormones, T4 and T3, are produced within the thyroid gland. Synthesis and release are stimulated by TSH, which is released from the pituitary gland in response to the hypothalamic factor, TRH (thyrotrophin-releasing hormone) (Fig. 15.1). Predominantly, T4 is produced, but this is converted in the peripheral tissues (liver, kidney, muscle) to the more active T3. More than 99% of T4 and T3 circulate bound to plasma proteins, mainly thyroid-binding globulin (TBG).
Thyroid function tests
Problems in interpreting thyroid function tests
Hypothyroidism
Investigations
Treatment
Myxoedema coma
Hyperthyroidism
Clinical features
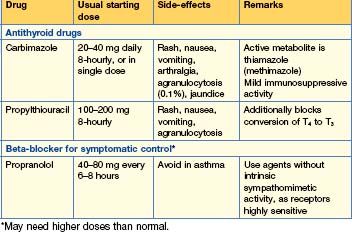
Treatment (Table 15.3)
There are three main options and preference varies widely.