6 Endocrine and reproductive systems
The thyroid gland
Basic concepts
Production of thyroid hormones
The thyroid gland secretes three hormones, triiodothyronine (T3), thyroxine (T4) and calcitonin.
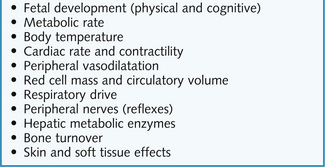
The principal effects of the thyroid hormones are: determination of basal metabolic rate and influence of growth through stimulation of growth hormone synthesis and action. Other effects are summarized in Figure 6.1.
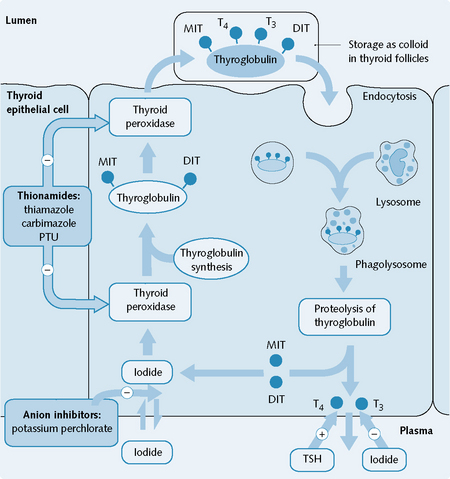
Thyroglobulin, now known as colloid, is endocytosed into the follicular cells, where it is broken down to release T3, T4, MIT and DIT T3 and T4 are secreted into the plasma; MIT and DIT are metabolized within the cells and their iodide is recycled (Fig. 6.2).
Control of thyroid hormone secretion
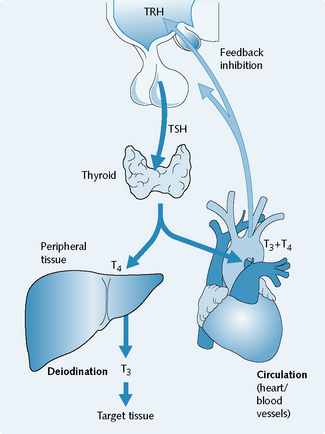
TSH reaches the thyroid gland through the systemic circulation where it stimulates thyroid hormone secretion (Fig. 6.3). Both T3 and T4 bind to proteins in the plasma (mostly thyroxine-binding globulin), and less than 1% of total thyroid hormones are free. It is the free thyroid hormones which exert the physiological effects. T3 is about five times more biologically active than T4, and T4 is converted to T3 in some peripheral tissues.
T3 and T4 exert negative feedback on the hypothalamus and pituitary.
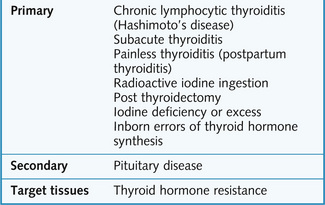
Thyroid dysfunction
Management of hypothyroidism
Levothyroxine
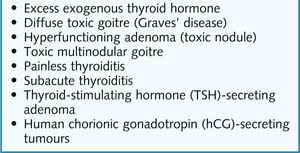
Management of hyperthyroidism
Thioureylenes
In the body, carbimazole is rapidly converted to active compound thiamazole.
Mechanism of action
The thioureylenes cause inhibition of thyroid peroxidase with a consequent reduction in thyroid hormone synthesis and storage (see Fig. 6.2). The effects of PTU may take several weeks to manifest as the body has stores of T3 and T4. PTU also inhibits the peripheral deiodination of T4 to T3.
Indications
Thioureylenes are used for hyperthyroidism. Patients sensitive to carbimazole are given PTU.
Anion inhibitors
Iodine, iodide and potassium perchlorate are examples of anion inhibitors.
Potassium perchlorate inhibits the uptake of iodine by the thyroid (see Fig. 6.2), but is no longer used owing to the risk of aplastic anaemia.
β-Adrenoceptor antagonists
The endocrine pancreas and diabetes mellitus
Insulin
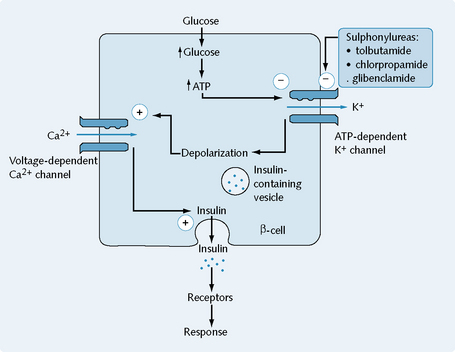
Insulin release is mediated by ATP-dependent potassium channels, located in the membrane of the β-cells. These close in response to elevated cytoplasmic ATP and decreased cytoplasmic ADP levels, resulting in depolarization of the membrane. This triggers calcium entry into the cell through voltage-dependent calcium channels, and subsequent insulin release (Fig. 6.6).
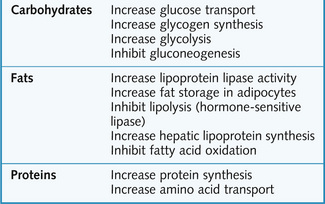
The effects of insulin are summarized in Figure 6.7.
Diabetes mellitus
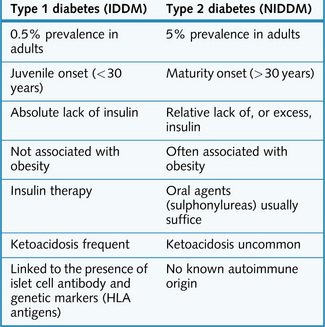
There are two types of diabetes mellitus:
The differences between the two types are summarized in Figure 6.8.
Management of diabetes mellitus
Insulin
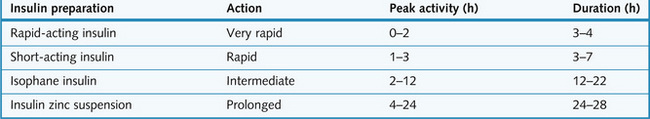
Nowadays the insulin preparation used is mostly the human (recombinant) insulin (however, insulin preparations of bovine origin are also available). Insulin is available as short-, intermediate-, and long-acting preparations (Figure 6.9).
Therapeutic regimen
Different regimens are used according to the patient’s needs and age:
Oral hypoglycaemics
Sulphonylureas
Gliclazide, tolbutamide, chlorpropamide and glibenclamide are examples of sulphonylureas.