Endocarditis
A. Brad Farris, III, MD
Key Facts
Terminology
GN following infection of heart valves
Etiology/Pathogenesis
Subacute bacterial endocarditis (SBE)
e.g., Streptococcus viridans infecting a rheumatic heart
Acute bacterial endocarditis (ABE)
e.g., Staphylococcus aureus infecting previously normal heart, as in an intravenous drug abuser
Clinical Issues
Hematuria and proteinuria
Renal dysfunction: ↑ BUN & creatinine (mostly with diffuse GN)
Hypocomplementemia
Microscopic Pathology
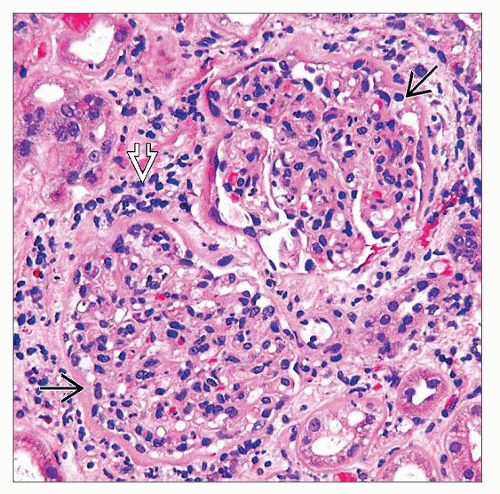
Diffuse or focal proliferative GN ˜ 50%
Neutrophils and nuclear fragments in glomeruli
Focal crescents
MPGN, type I pattern ˜ 50%
Lobular mesangial hypercellularity, duplicated GBM
IF: Usually IgG, IgM, and C3 (subendothelial & mesangial); sometimes IgA
EM: Mesangial & subendothelial amorphous deposits
Top Differential Diagnoses
Postinfectious GN, other site
MPGN, type I
Lupus nephritis
ANCA-related GN
TERMINOLOGY
Abbreviations
Subacute bacterial endocarditis (SBE)
Acute bacterial endocarditis (ABE)
Synonyms
Embolic nonsuppurative focal nephritis
Focal embolic nephritis
Focal and segmental proliferative, necrotizing, or sclerosing glomerulonephritis (GN)
Definitions
GN following infection of heart valves (i.e., endocarditis)
ETIOLOGY/PATHOGENESIS
Infectious Agents
SBE: Classic example is Streptococcus viridans group bacteria infecting a rheumatic heart
Coagulase-negative staphylococci, including S. epidermis, have also been observed
Others observed
Actinobacillus actinomycetemcomitans, Enterococcus, Streptococcus mitis, Haemophilus influenzae, Neisseria gonorrhea, Chlamydia psittaci, Bartonella henselae, Coxiella burnetii
Subacute endocarditis due to Streptococcus bovis and N. subflava bacteremia has been reported in a case with concurrent high antineutrophil cytoplasmic antibody (ANCA) (anti-proteinase-3) titer
Of note, positive ANCA has also been reported in another series of GN associated with endocarditis
ABE: Classic example is Staphylococcus aureus infecting previously normal heart (e.g., as in an intravenous drug abuser)
Proportion of bacterial endocarditis-associated GN caused by S. aureus appears to be increasing, causing > 50% of all cases and > 1/3 of fatal cases
40-70% of intravenous drug abusers with acute endocarditis from S. aureus have GN
Immunologic injury is thought to be primary mechanism of endocarditis-associated GN
Presence of glomerular immune complexes is evidence of this process
Serum complement is depressed, also indicative of process involving immune system
Circulating immune complexes have been demonstrated in patients with infectious endocarditis
Eluates from kidney with focal GN associated with endocarditis have been shown to react with bacterial antigens derived from bacteria cultured from patient’s blood
Earlier investigators thought that direct action of bacterial emboli lead to endocarditis-associated GN when they observed emboli in glomeruli
Called “focal embolic GN” or “embolic nonsuppurative focal nephritis” before pathogenesis was attributed to mechanisms other than embolization
Focal GN in patients involving only right side of heart suggest that embolization is not major mechanism
CLINICAL ISSUES
Epidemiology
Incidence
Antibiotic therapy has decreased incidence of GN due to endocarditis
Studies of endocarditis have indicated an incidence of GN in patients with infectious endocarditis of 2-60%
Indicates that it is difficult to provide accurate measure of this incidence
Of endocarditis cases, renal disease is presenting feature in 20% of patients
Presentation
Hematuria
Macroscopic hematuria
May be associated with the GN or renal infarction from “septic” emboli
May persist or resolve and may be intermittent
Proteinuria
Usually mild; nephrotic syndrome rare
Urinary casts
Hypocomplementemia
Frequently seen (but not always) and not specific to renal involvement
Seen in 70-90% of patients with diffuse GN and 60% of patients with focal GN before advent of antibiotic therapy
Associated with activation of classical complement pathway
Renal dysfunction
Variable to severe
BUN and creatinine elevations are typically associated with diffuse form of GN
Uremia seen in 5-10% of patients before epoch of antibiotics and in 3-4% after advent of antibiotics
Roth spots
Anemia
Hepatosplenomegaly
Purpura
Pulmonary hemorrhage has been reported as initial symptom (& initially confused with Goodpasture syndrome)
Laboratory Tests
Rheumatoid factor may be positive
Circulating immune complexes may be present
Cryoglobulins (mixed [type III]) have been reported
Treatment
Surgical approaches
Valve vegetation removal or valve replacement may be required
Drugs
Antibiotic therapy may achieve resolution of milder endocarditis-associated GN
Antibiotic prophylaxis in patients at risk for endocarditis may reduce incidence of endocarditis-associated GN
Corticosteroids may be used in brief course
May help in resolution of nephritis without exacerbating the endocarditis
Plasmapheresis has been uncommonly used in aggressive cases
Prognosis
Partial to total resolution of renal disease occurs after antibiotic therapy
Proteinuria, circulating immune complexes, cryoglobulinemia, and elevation of rheumatoid factor (if present) resolve with effective treatment
MACROSCOPIC FEATURES
General Features
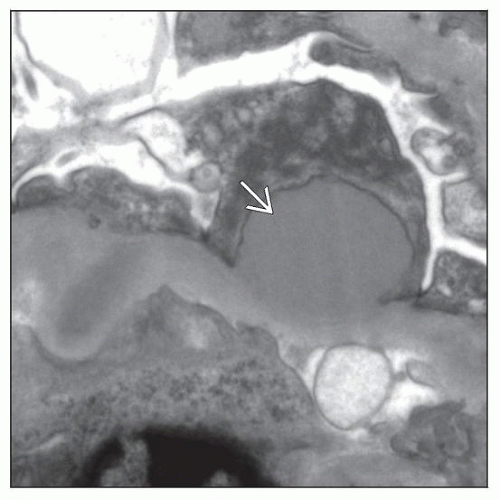
Abscesses may occur in severe cases
Renal infarction (in up to 50-57% of cases according to some early studies, including autopsy data) may occur in severe cases
Single or multiple and grossly appreciable, of size associated with arcuate or large interlobular arteries
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree