Embolectomy
Peter Henke
Overview, Epidemiology, and Brief Pathophysiology
Acute limb ischemia (ALI), for which embolectomy remains a standard therapy, is one of the most common vascular emergencies that surgeons encounter. The incidence will only increase as the population ages and cardiac care improves. Prompt recognition and diagnosis, followed by rapid restoration of blood flow to the ischemic extremity will decrease limb loss and subsequent reperfusion-related local and remote organ injury. This disease most often occurs in aged patients, who often have significant comorbidities, and which can lead to their demise even after successful revascularization of a limb.
A useful limb ischemia categorization system is the Society for Vascular Surgery/International Society for Cardiovascular Surgery (SVS/ISCVS) joint consensus document (Table 1). Class I is a viable limb that is not immediately threatened, no sensory or muscle weakness is present, and arterial Doppler and venous Doppler signals are audible. Category II is a threatened limb, with IIa being marginally threatened if promptly treated, with minimal to no sensory loss, inaudible arterial Doppler signals, but audible venous Doppler signals present. Category IIb is an immediately threatened limb, which requires rapid revascularization, and is associated with sensory loss and associated mild muscle weakness with inaudible arterial and venous signals. Category III is irreversible limb ischemia, with major tissue loss or permanent nerve damage, a profoundly anesthetic and paralyzed limb, with rigor and inaudible signals. The patient whose disease falls into this category almost always requires amputation.
Table 1 SVS Grade Acute Limb Ischemia | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||
The pathophysiology of ALI is due to an abrupt and complete blockage of the main arterial supply to the extremity. Unlike chronic limb ischemia, limb saving collaterals are not well developed. The distal tissue bed in the limb becomes ischemic with energy metabolism shifting from an aerobic to an anaerobic process. Progressive ischemia leads to cell dysfunction and death. Nerve cells, followed by muscle cells, are most susceptible. A patient without underlying vascular disease and an acute arterial blockage has approximately 6 hours for revascularization before irreversible functional tissue damage occurs. Upon reperfusion, release of cellular products may cause systemic organ injury such as renal and pulmonary failure. Both these factors need to be kept in mind when treating these patients.
 Anatomy, Diagnosis, and Indications
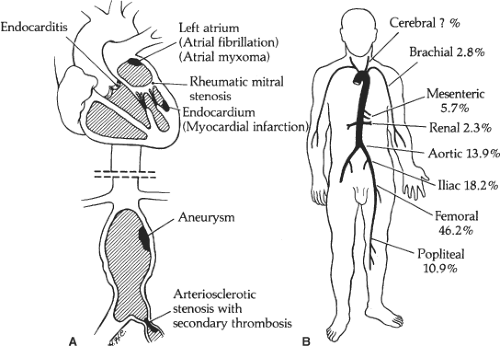
Anatomy, Diagnosis, and IndicationsThe etiology of ALI is often an embolic process, usually a thromboembolism, and commonly from a cardiac source. This is typically observed after a patient develops atrial fibrillation with a left atrial thrombus or after a myocardial infarction with a left ventricular thrombus. Common locations of embolic lodgment are at arterial bifurcations where the artery size changes, such as the aortic bifurcation, femoral bifurcation, or popliteal artery, and less frequently at other locations (Fig. 1).
The diagnosis is made with a combination of history and PE findings. The classical findings are the 6 P’s; pain, pulselessness, poikliothermia, pallor, parathesis, and paralysis. The clues important for determining the etiology of ALI are readily obtainable by the history and physical features (Table 2). Often, the location of the embolism can be determined by physical examination. For example, in a patient with new onset atrial fibrillation and right leg ALI, a nonpalpable right femoral pulse and normal left lower extremity pulse examination suggests thromboembolism, for which embolectomy would be appropriate. Conversely, an aged patient with longstanding peripheral arterial disease and claudication, who presents with a cool right lower extremity and a weakly palpable femoral pulse and only dopplerable signals in the contralateral nonaffected side, probably does not have an embolic etiology causing their limb ischemia. This patient would be best
addressed with an arteriogram or CT angiogram and possible endoluminal intervention.
addressed with an arteriogram or CT angiogram and possible endoluminal intervention.
Other etiologies of ALI include in situ arterial thrombosis, peripheral bypass thrombosis, peripheral arterial aneurysms, trauma (popliteal artery disruption or penetrating injury), or acute aortic dissection with occlusion of the aorta or iliac arteries. These need to be considered in the differential, but will not be discussed in this chapter as they are not primarily treated with embolectomy.
Men and women are equally affected by ALI. Modern series amputation rate is 13%, mortality is approximately 10%, and the average hospital length of stay estimated for these patients is approximately 10 days. Generally, ALI does not occur in young people outside of trauma, but it may occur in young patients due to unusual circumstances such as paradoxical emboli, hypercoagulable disorders, popliteal artery entrapment syndrome, or in those with severe early onset cardiac disease.
Emphasizing the need for excellent judgment is assessment of late SVS grade III limb ischemia. While perhaps obvious, it is important not to attempt embolectomy in those with nonrecoverable ischemia, as the tissue is not viable. Sometimes, the limb examination is marginal, and revascularization with reassessment of tissue viability is reasonable with close observation and a low threshold to amputate if warranted by clinical status. Frank discussion with the patient and their family is important, as there is high potential for limb loss.
Two primary factors underlie the morbidity and mortality that results from ALI: the patients’ underlying comorbid illness and delay in recognition and revascularization of the limb(s). It is uncommon that embolectomy itself will directly cause death. In a mixed etiology of ALI, factors associated with amputation free survival (AFS) have been evaluated. Decreased AFS is associated with non-Caucasian race, older age, a history of neurological disease, malignancy, congestive heart failure, and low body weight. Not surprisingly, skin mottling and rest pain are associated with increased risk of amputation. Another study suggested that ALI-related mortality was increased with delay in treatment of ischemia, significant underlying atherosclerosis, and poor arterial back bleeding at operation.
Selection of appropriate therapy is also an important factor to decrease amputation occurrence and mortality. While strong evidence suggests equivalence of endovascular or surgical therapies, as measured by mortality and amputation, the etiology of the ALI needs to be factored into this equation. Two landmark articles were published in the 1990s, which suggested that thrombolytic therapy had equivalent outcomes to surgical therapy in patients with ALI. These were the Surgery or Thrombolysis in Lower Extremity Ischemia (STILE) and Thrombolysis or Peripheral Artery Surgery (TOPAS) trials, which randomized patients to arteriography and thrombolytic therapy with urokinase, versus arteriography and embolectomy or urgent bypass. While these data are robust, it is important to note that a majority of patients in both of these trials had class I and IIa ischemia, with <25% having class IIb or III limb ischemia, for which embolectomy is most commonly performed. A large national database study suggested that in those patients with an embolic etiology (generally stage IIb ischemia), amputation is significantly less likely with embolectomy, but not thrombolytic therapy. Importantly, patients who failed thrombolytic therapy had a significantly greater risk of amputation and death. The bottom line is that providers must choose the appropriate therapy very carefully for patients with ALI.
Table 2 History and Physical Features of Acute Limb Ischemia | ||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||
Patient management includes intravenous fluid resuscitation, immediate anticoagulation
(if no contraindications), and then a decision is made to proceed with an endovascular approach or surgical thromboembo-lectomy (Fig. 2). Regardless of the etiology, the patient should be maximally resuscitated with intravenous fluids such as normal saline (no potassium until renal function determined), supplemental oxygen, and all patients should receive per oral or per rectum aspirin. Standard chemistry and hematology laboratory screening should be done, including a type and screen. Consideration of intravenous (IV) mannitol to induce a diuresis, as well as yielding some oxygen radical protection, should be given. It is also reasonable to alkalinize the urine if myoglobinuria is present. Similarly, while no level I evidence exists, use of extracorporeal renal support with CVVHD in patients who have significant tissue ischemia and acute renal insufficiency makes sense to decrease potentially fatal reperfusion hyperkalemia that may result. This therapy can be ongoing with the patient in the operating room.
(if no contraindications), and then a decision is made to proceed with an endovascular approach or surgical thromboembo-lectomy (Fig. 2). Regardless of the etiology, the patient should be maximally resuscitated with intravenous fluids such as normal saline (no potassium until renal function determined), supplemental oxygen, and all patients should receive per oral or per rectum aspirin. Standard chemistry and hematology laboratory screening should be done, including a type and screen. Consideration of intravenous (IV) mannitol to induce a diuresis, as well as yielding some oxygen radical protection, should be given. It is also reasonable to alkalinize the urine if myoglobinuria is present. Similarly, while no level I evidence exists, use of extracorporeal renal support with CVVHD in patients who have significant tissue ischemia and acute renal insufficiency makes sense to decrease potentially fatal reperfusion hyperkalemia that may result. This therapy can be ongoing with the patient in the operating room.
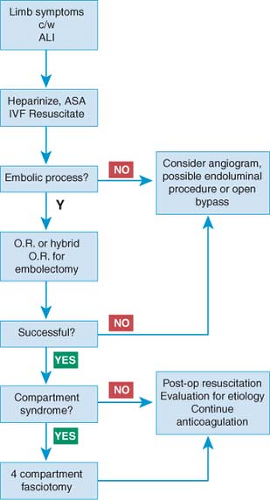 Fig. 2. Algorithm of treatment for acute limb ischemia (ALI) and catheter embolectomy. ASA, aspirin; OR, operating room. |
It cannot be emphasized strongly enough that all patients with ALI receive rapid, full anticoagulation (except if actively bleeding). This is typically heparin, bolused with 100 to 150 U/kg, and then titrated to maintain an activated partial thromboplastin time (aPTT) of two to two-and-a-half times baseline. If the patient has a known history of heparin-induced thrombocytopenia or an anti-thrombin deficiency, alternative agents, such as direct thrombin inhibitors (lepirudin or argatroban), can be used and aPTT can be used to guide dosage.
Laboratory markers may help predict major amputation risk in those with ALI. A recent study suggested several serum markers are associated with major amputation. Initial laboratory measures may predict amputation risk. For example, creatinine phosphokinase (CPK) elevation and neutrophilia upon presentation confer a tenfold increased risk of amputation, as compared to those without CPK elevation. It is not clear if CPK elevation after revascularization carries the same prognosis, but is unlikely, as washout of the ischemic tissue bed normally occurs.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree