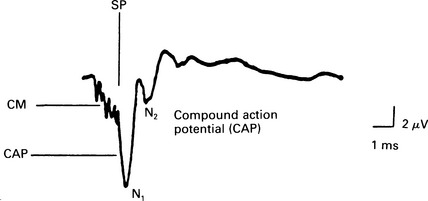
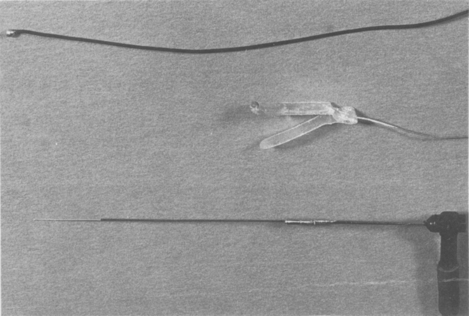
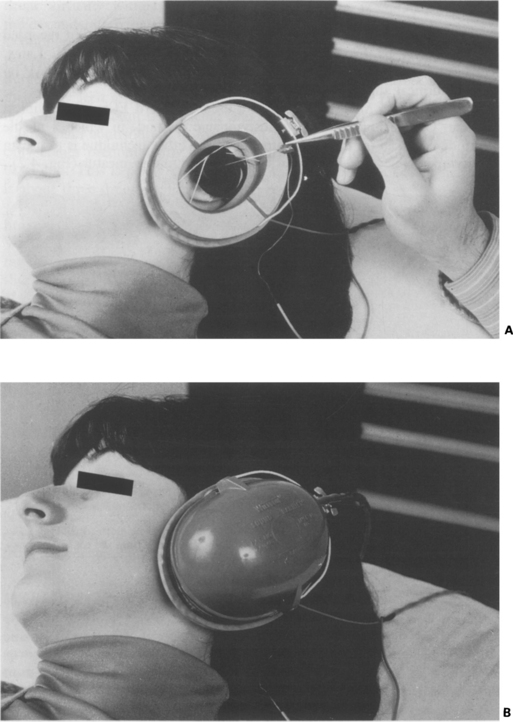
4 Auditory-evoked potentials from the receptor organ (CM and SP) and the action potential (AP) of the VIIIth nerve can be recorded using the near-field recording method of electrocochleography (Fig. 4.1). The CM and SP occur virtually without delay, and the AP occurs within the first few milliseconds after the stimulus onset for high-level click stimuli. Fig. 4.1 Cochlear and VIIIth nerve potentials in response to a monophasic click. The CM appears on the leading edge of the SP response. The AP is best elicited in response to abrupt, transient sounds such as a broad-band click, which activates the neural fibres in synchrony (Fig. 4.1). Within a few milliseconds, the activity in the fibres returns to their normal, random, very low rate of discharge, and the AP is not observed. It can be shown (Kiang, Moxon & Kahn 1976) that the AP is the convolution integral of the single-fibre impulses. Thus, the surface-recorded or compound AP reflects both the number of fibres activated and the degree of synchrony among them. The highest speed of the travelling wave propagation is in the basal turn, and, therefore, the synchronization of the AP is greatest at the high-frequency region of the cochlea. Travelling wave propagation towards the apical part of the cochlea and progressive time delay creates out-of-phase responses of individual fibres with less synchrony. Therefore, the contributions from more apical regions are more difficult to record. In man, the compound AP shows two or three negative peaks (N1, N2, and sometimes N3) which are thought to be recorded from the nerve up to the level of the medial part of the internal auditory meatus. However, in small laboratory mammals, in which the VIIIth nerve is much shorter, the N1 potential recorded from the promontory represents a synchronized response from the auditory nerve, and the N2 peak represents response from the neurones of the cochlear nucleus (Ruben et al 1982, Moller 1983). Cochlear microphonics from the round window of man were first recorded during surgery by Fromm et al (1935) and Gersuni et al (1937). Later, Ruben et al (1959, 1961, 1967) and Ronis (1966) recorded CM and AP by using a surgical approach to the round window. At present, two main techniques are used to record ECochG in clinical practice. One technique is the transtympanic method, in which a needle electrode is placed on the promontory, and the other technique is to use an extratympanic electrode placed in the external auditory meatus (Fig. 4.2). Fig. 4.2 Transtympanic needle electrode (botom), an extratympanic electrode (middle), and silver ball electrode (top) which may be used to record either from the round window or the annulus. The transtympanic method was attempted by Lempert (1950) and successfully developed and popularized by Portmann (1968). The sterile needle electrode is insulated, apart from its tip, and is placed, through the tympanic membrane, aseptically onto the promontory of the cochlea. It is kept in place by elastic hooked over the electrode holder. This stabilizes the electrode and maintains contact with the promontory (Fig. 4.3). Fig. 4.3 (A) The placement of a needle electrode used in transtympanic electrocochleography. The earphone is held in position by the circumaural magnetic base so that it can be placed on the ear (B) after the electrode has been inserted. The electrode is positioned midway between the tip of the malleus and the annulus of the tympanic membrane at the position of about 8 o’clock for the right ear, or 4 o’clock for the left ear. In this position, the electrode rests in front of and close to the round window niche. An operating microscope facilitates the accurate placement of the electrode. It should be noted that the closer the electrode is placed to the round window, the greater are the recorded potentials (Yoshie 1985). Extratympanic ECochG has been recorded by implanting a needle electrode into the posterior meatal wall (Yoshie et al 1967, Elberling & Salomon 1971). In order to make the technique less invasive, various designs of non-traumatic surface electrodes in the form of a ball or wick attached to the wire have been placed on the eardrum (Cullen et al 1972, Khechinashvili & Kevanishvili 1974), or close to the annulus (Yoshie 1973, Coats 1974). Coats (1974) designed an atraumatic, external, auditory meatus electrode from a narrow strip of acetate, which he bent into ‘V’-shape to provide the tension needed to maintain good contact. This electrode was inserted in a closed position with ear forceps. An insulated silver wire was connected to a 0.4 mm-diameter silver ball positioned at the tip of the electrode (Fig. 4.2). The contact point was located within 5 mm of the tympanic annulus in the area between 3 and 9 o’clock for the right ear. Singh et al (1980) obtained good-quality recordings by using an endomeatal silver/silver chloride electrode measuring 2 × 1 × 0.5 mm and soldered to a very flexible wire. The electrode was attached with conductive electrode paste to the meatal wall close to the annulus at the level of about seven o’clock for the right ear or the equivalent 5 o’clock for the left ear. Ear-canal preparation to remove wax is usually necessary before introducing the electrode. A sterile needle electrode should be used, and an aseptic technique should be employed in placing the electrode. The transtympanic electrode usually can be stabilized in position better than extratympanic electrodes. Intramuscular injection of ketamine has been recommended for anaesthesia in children under 3 years of age (Hutton 1981). Anaesthesia starts within a few minutes and lasts for about half an hour. If necessary, a second injection can be given. ECochG under general anaesthesia in adults is very rarely indicated, and placement of both extratympanic and transtympanic electrodes can be tolerated without local anaesthesia on most occasions. Yoshie (1973) used a Japanese acupuncture needle as an electrode for his patients. The discomfort from the transtympanic method is comparable to that of a transcutaneous injection. For nervous patients, an anxiolytic dose of oral diazepam may be helpful. Also, it will improve the recording by reducing muscular activity and hence improving the signal-to-noise ratio. The commonest click stimulus is a square electrical impulse of 100 μs duration presented to an earphone or insert receiver. Tone bursts of several milliseconds, usually 4–20 ms in duration, can be used with short rise–fall times of 0.1–2 ms, depending on the frequency of the stimulus. Tone bursts of 2000 Hz and 1000 Hz should have rise–fall times of 1 ms and 2 ms, respectively. This can improve the frequency specificity of the AP when recorded close to the threshold. However, the main advantage of the tone bursts is in obtaining CM and SP. Simultaneous ipsilateral masking to obtain derived-responses can be used to get better, frequency-specific responses from the cochlea. The number of sweeps per average ranges from 128 to 512, depending on conditions of recording and signal-to-noise ratio. Up to 1000 responses need to be averaged when an extratympanic electrode is used. Near-threshold replications of the response should be obtained to avoid false-positive errors, and at least two averages should be recorded and compared (Bell & Thornton 1988). The recommended recording bandwidth of the filters is 30–3000 Hz. The analysis window is 10–20 ms.
Electrocochleography (ECochG)
GENERATORS OF COCHLEAR AND VIIITH NERVE POTENTIALS
METHODS
Electrode placement
Anaesthesia for electrode placement
Technical aspects of stimulation and recording
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Basicmedical Key
Fastest Basicmedical Insight Engine
