57 Eczema and psoriasis
Eczema
Pathology and clinical features
Acute eczema is an inflammatory process leading to oedema in the epidermis. The oedema is seen histologically in the epidermis as ‘spongiosis’. Oedema manifests as fluid that collects into tiny blisters which may then coalesce. This is seen histologically as intraepidermal vesicles and clinically as pompholyx blisters on thicker palmar and plantar skin, and as excoriated, ruptured crusted vesicles elsewhere. Tightly packed keratinocyte cells in the epidermis usually prevent transepidermal fluid loss and the entry of pathogens. This barrier function of the skin is lost in eczema. A schematic diagram demonstrating the normal skin epidermis and the effects on the barrier function during an acute eczema flare is shown in Fig. 57.1.
In the chronic form of eczema, prolonged rubbing and scratching results in a thickened epidermis and an increase in the upper horny cell layer of keratin, termed hyperkeratosis. Clinically, the skin appears thick, leathery, scaly and ‘lichenified’ with exaggerated skin markings, like tree bark (Fig. 57.2). Both acute and chronic stages are accompanied by a heavy chronic inflammatory cell infiltration of the dermis and epidermis. The main consequent symptom of these pathological processes is itch. The dictum of ‘if it’s not itchy, it’s not eczema’ holds true.
Clinical types
Atopic eczema
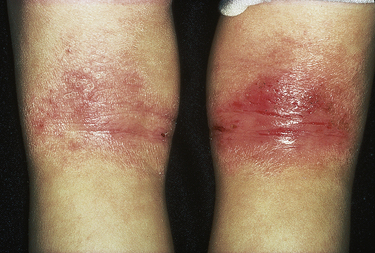
Atopic eczema is diagnosed clinically and the criteria for definition include chronic itchy skin with three or more of the following: a history of flexural involvement of the skin creases, visible flexural involvement, dry skin, other atopic disease or onset within the first 2 years of life. The clinical course and distribution change through puberty and adulthood. In infants, common areas affected are face, neck and nappy area. Through childhood, flexural sites such as folds of the elbows and backs of the knees are classically involved (see Fig. 57.3). Symptoms usually improve with age and approximately 60% have resolution of symptoms by the age of 16.
Exacerbating factors
A number of factors can aggravate atopic eczema:
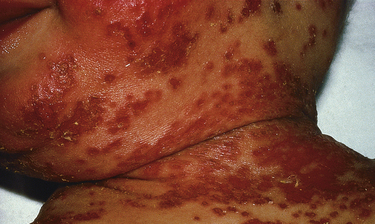
The commonest trigger in the paediatric population is secondary infection, either bacterial or viral. Bacterial colonisation is common on the skin of those with atopic dermatitis and may result in the invasive infection triggering an acute flare. Staphylococcus aureus and Streptococcus spp. are most often responsible (Fig. 57.4).
Contact dermatitis
Allergic contact dermatitis
Many common compounds can lead to ACD. The most common compounds implicated are:
The standard confirmatory investigation is patch testing and is used to differentiate allergic from ICD. This involves application of a standard, with or without a specialised range of compounds, to the patient’s back over 72 h. This is followed by examination for a cutaneous reaction at day 2 and day 4. Identification of relevant compounds allows the patient to avoid the substance in the future, and this will hopefully reduce symptoms. Common areas of the body affected by ACD, with corresponding probable sensitisers, are listed in Table 57.1.
Table 57.1 Common locations for allergic contact dermatitis and possible sensitisers
| Location | Possible sensitising agents |
|---|---|
| Periorbital | Airborne allergens, nail polish, contact lens solution |
| Umbilicus | Nickel hypersensitivity to belt/jean button |
| Neck | Antiseptic in soap, cosmetics |
| Hairline | PPD in hair dye, hair perming solution |
| Hands | Latex or rubber accelerators in gloves, nickel, fragrances, protein contact dermatitis in food preparation, irritant contact dermatitis due to water |
PPD, p-phenylediamine.
Irritant contact dermatitis
This is the most common form of occupational dermatitis and the commonest cause of hand eczema (Fig. 57.5). Unlike ACD, ICD is not immunologically mediated. The mechanism involves disruption of the epidermal permeability barrier and a direct cytotoxic effect depending on the irritant. Patients with pre-existing epidermal barrier dysfunction such as atopic eczema are at higher risk. The occupation of the individual may also be a risk factor, especially those working as builders, hairdressers, gardeners, healthcare workers and chefs. Irritants include detergents, oils, water, inorganic acids, alcohols and plastics. Preventative skin care is key and this includes the use of barriers such as emollients or cotton gloves in addition to avoiding suspected irritants.
Treatment
Emollients
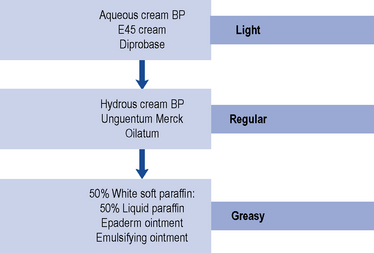
Emollients, topical hydrating agents consisting of fat or oil to soften the skin, are the mainstay of eczema management. Emollients are effective first-line treatments for all types of eczema, and regular, liberal use will reduce topical steroid requirements. The greasier products have more emollient effect (see Fig. 57.6). They are often underused and the need to educate the patient regarding use of sufficient quantities is vital. Dry skin is aggravated by soap and bath products, and therefore an emollient soap substitute for washing is advisable.
Topical corticosteroids
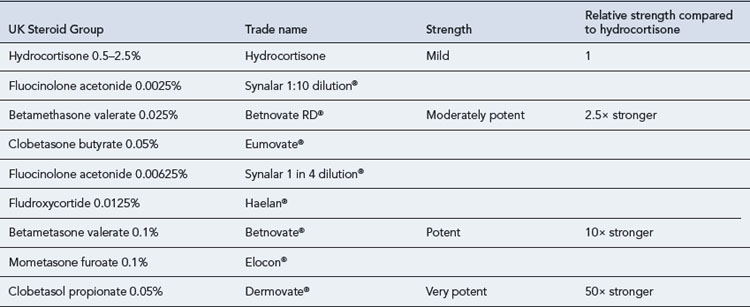
Topical steroids are classified into four main groups according to potency: mild, moderately potent, potent and very potent (Table 57.2). The choice of topical steroid is dependent on the site and severity of skin disease. Potent and very potent steroids should be avoided on delicate sites such as the face, genitals and flexures. The periorbital region should be treated with caution due to the thin skin increasing the likelihood of absorption and risk of cataracts or glaucoma. Treatment should be reviewed regularly and tailored accordingly. It is also important to remember that any form of occlusion will increase the absorption of steroid applied.
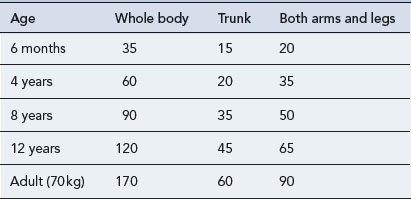
Local and systemic side effects are extremely rare with appropriate use and duration of topical steroid treatment. Patients should be advised to spread preparations thinly either once or twice daily. The recommended amount used can be quantified using a fingertip unit (Fig. 57.7). The quantity in this unit is sufficient to cover an area the size of two adult palms. Table 57.3 details the quantities for application to different sites required for twice-daily treatment for 1 week.
Calcineurin inhibitors
Pimecrolimus 1% cream (Elidel®) is indicated for short-term or intermittent long-term use in mild to moderate atopic dermatitis. Studies have shown that it is effective, well tolerated and has minimal adverse effects in the long-term control of eczema in children aged over 2 years (Langley et al., 2008). Furthermore, this has resulted in the reduced use of topical steroids leading to a lower risk of steroid-induced side effects (Kapp et al., 2002).
Systemic therapies
Methotrexate
Methotrexate is occasionally used in unresponsive adult atopic eczema, but randomised controlled trials are lacking. A small prospective trial has shown that methotrexate can be effective and well tolerated as a second-line therapy for the treatment of moderate to severe atopic eczema in adults (Weatherhead et al., 2007).
Phototherapy
Phototherapy can be effective in select cases of atopic dermatitis. Narrow-band UVB is the therapy of choice (Gambichler et al., 2005; Meduri et al., 2007). The potential side effects of all types of phototherapy include burning, premature ageing and a small increased risk of skin cancer. A small proportion of patients have photosensitive eczema, and this should be determined by taking a detailed patient history before prescribing phototherapy treatment. A treatment course requires a patient to attend two or three times a week for at least 6 weeks.
Dietary supplements
Interactions with drugs used in the treatment of eczema and psoriasis are shown in Table 57.4.
Table 57.4 Interactions with drugs used in the treatment of eczema and psoriasis
| Interacting drug | Outcome | |
|---|---|---|
| Methotrexate | Aspirin | Increased plasma concentration and toxicity of methotrexate |
| NSAIDs | Increased plasma concentration and toxicity of methotrexate | |
| Probenecid |