Echinococcal Cysts: Laparoscopic Approach
Eduardo De Santibañes
Rodrigo Sanchez Clariá
Introduction
Hydatid disease is a zoonotic infection caused by adult or larval stages of the cestode Echinococcus granulosus.
Hydatid disease is endemic mainly in the Mediterranean countries, the Middle East, the Baltic areas, northern China, India, South America, New Zealand, Australia, and other sheep-raising areas.
The adult E. granulomatosus is a worm that resides in the jejunum of dogs and other canines that produce eggs that pass in the stools; these eggs can be ingested by intermediate hosts such as sheep, cows, and humans and liberate an embryo in the duodenum, then penetrate the intestinal wall and enter the portal system to reach the liver, lung, and other distant sites where they are transformed into cysts.
Most of these embryos are trapped in the liver, the rest pass through the liver and are scattered to other organs; however, the liver is infected in 60% of cases, the lung in about 20%, and the remaining organs in about 20% (kidney, brain, bone, spleen, and others).
Humans are accidental intermediate host due to ingestion of the parasitic eggs in contaminated vegetables, meat, or through direct contact with dogs (especially in children).
There are four documented species, being E granulomatosus and Echinococcus multilocularis the most common associated with hydatid disease in humans.
Hydatidosis may be asymptomatic for many years.
It may become evident when a cystic lesion is noted while the liver is imaged for other reason.
They tend to grow slowly, displacing normal hepatic parenchyma and other adjacent organs.
When hydatid cysts become symptomatic, their clinical presentation varies, from simple discomfort to acute abdomen.
Typical signs and symptoms are produced by two mechanisms: a generalized toxic reaction due to the presence of the
parasite itself characterized by anaphylaxis and shock and mechanical symptoms depending on the location, size, and complications of the cysts.
parasite itself characterized by anaphylaxis and shock and mechanical symptoms depending on the location, size, and complications of the cysts.
Pain in the right upper quadrant, nausea, and vomiting are the most common symptoms and a palpable mass is the most common sign in the physical examination.
Complications precede the diagnosis of the disease in 50% of the patients.
Infected cysts, rupture with intraperitoneal disease, and penetration of daughter cysts into the biliary tree causing obstructive jaundice and cholangitis are the most common complications.
Patients with exceptionally large cysts may also present signs of vena cava compression or portal hypertension.
The typical lesion is a cystic cavity filled with clear hydatid fluid containing live protoscoleces (Fig. 1).
The hydatid cyst of the liver has two layers: the outer acellular layer called the pericyst or ectocyst, a dense fibrous host reaction to the parasite that is 2 to 5 mm thick and it consists of compressed liver cells and fibrotic tissue, and an inner cellular germinal layer that is called the endocyst or the germinative membrane from which brood capsules containing protoscoleces proliferate toward the cystic cavity.
The pericyst is calcificated in approximately half of the patients.
Partial calcification of the cyst does not always indicate death of the parasite, whereas total and densely calcified cysts are considered inactive.
Because of the paucity of pathognomonic signs and symptoms of uncomplicated cyst, the diagnosis of hydatid disease of the liver is based on history, clinical suspicion, and images.
A history of living in or visiting an endemic area must be established.
Imaging is the main method that is relied on for diagnosis while serology tests are used to verify the imaging results.
Ultrasound has been chosen as the first-line diagnostic tool.
It is inexpensive, noninvasive, gives instant results, and is also used to classify the different cysts.
Gharbi’s classification as determined by ultrasound describes the stage of the cysts and is still being used (Table 1).
It is clinically relevant because therapy is often stage based.
Ultrasound specificity and sensitivity are 90% and 98%, respectively.
Computed tomography (CT) and magnetic resonance imaging (MRI) complement the information obtained by ultrasound.
These can provide better information regarding the size and location of the cysts, its relationship between adjacent structures, and the presence of the cysts in other organs.
CT sensitivity rate is 100%; it is more useful for following up the lesions during medical treatment with albendazole, demonstrating the calcifications and determining postoperative recurrence.
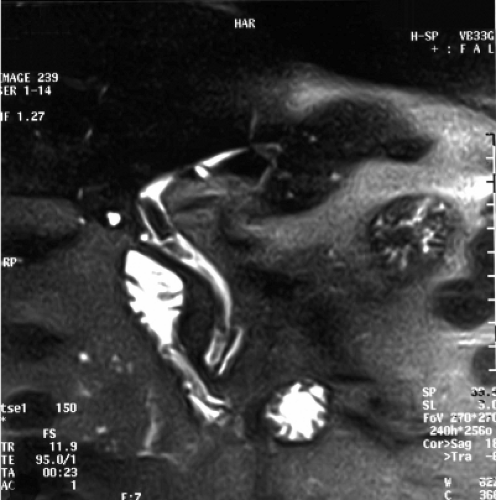
The presence of daughter cysts in the common bile duct and exogenous cysts can also be more clearly seen on MRI (Fig. 2).
So, ultrasound should be used in combination with CT and MRI in the diagnostic workup of patients with hydatid disease.
Endoscopic retrograde cholangiopancreatography (ERCP) is used preoperatively for patients with jaundice, history of cholangitis, dilatation of the biliary tree, existence of debris in the bile ducts, or elevation of serum liver tests.
Table 1 Gharbi’s Classification of Cystic Hydatid Disease | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||
With this method, the common bile duct is cleaned of the germinal vesicles and an efficient drainage is provided.
Some centers also use routine ERCP to define the bile duct anatomy and to visualize subclinical connection between the cyst and the biliary system before surgery.
We use MRI to clarify the anatomy and visualize the connection between the cyst and the biliary tree.
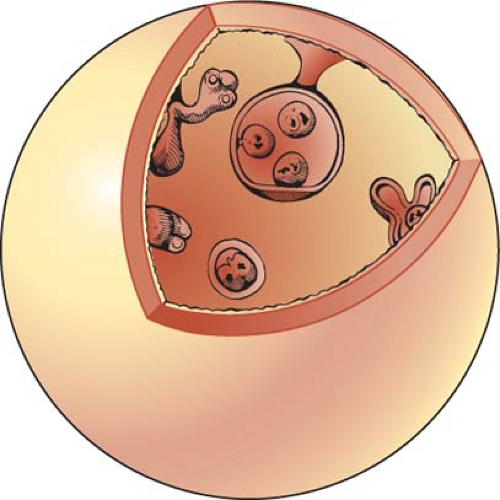 Fig. 1. The single-celled germinal membrane gives rise to brood capsules, which contain the scoleces, and daughter cysts which float in the clear cyst fluid. |
The disease is confirmed by enzyme-linked immunosorbent assay (ELISA) and the indirect hemagglutination test.
The basic principle of the immunological tests is based on determining the antibodies produced as a consequence of leaking antigens from the cyst fluids.
The tests may be negative if there is no leakage, the cyst is calcificated, or the parasite is dead.
So serological assays should be used to confirm the infection suspected on clinical findings and imaging studies.
Other laboratory tests, such as hematological tests and biochemical liver tests, are considered less sensitive, although some authors suggest that eosinophil count determination is important to determine the diagnosis and for control of the postoperative recurrence.
Fine needle aspiration biopsy of the cyst performed under ultrasound guidance is controversial; however, under antihelmintic coverage, it is generally safe and diagnostically useful in cases with no detectable serum antibodies and inconclusive appearance.
Although treatment choices for hydatid disease of the liver have increased in the last two decades, including medical treatment and percutaneous treatment, surgery remains the mainstay of therapy.
Several surgical procedures have been described for treatment of hepatic cyst, ranging from simple puncture to liver resection and liver transplantation.
Chemotherapy with albendazole is the medical treatment of choice, but it should be used in conjunction with surgery.
With the introduction of albendazole in the preoperative period, the risk of recurrence due to spillage has been considerably reduced, so it is mandatory to use it in the treatment of this disease.
It is also used for disseminated disease and in inoperable cases.
We use albendazole 4 weeks before and after surgery; if we suspect that during surgery we have any kind of spillage, we use it for 6 months, and if not, we use it for 3 months postoperative.
Percutaneous treatment or puncture/aspiration/injection/reaspiration (PAIR) has been proposed as an alternative to surgery, especially in patients who cannot or do not want to undergo surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree