FIGURE 55-1 (A) Basal ECG of a 7-year-old child (type 2). (B) ECG positive for Brugada syndrome (type 1) during ajmaline infusion. The infusion was stopped after the positive result. (C) NSVT observed two minutes after stopping the infusion of ajmaline.
CONCEPT
Brugada syndrome is an autosomal-dominant, inherited channelopathy characterized by ST-segment elevation or J wave in the right precordial leads. First described in 1992,1 the syndrome is associated with a high incidence of SCD secondary to a rapid polymorphic VT or VF in patients with structurally normal hearts.
EPIDEMIOLOGY
The prevalence of the Brugada ECG pattern is variable, ranging from 3% in endemic areas of Southeast Asia to 0.61% in Europe. In the United States, the prevalence ranges from 0.012% to 0.43%. However, because the diagnostic ECG pattern can be intermittently present or concealed, it is difficult to estimate the true prevalence of the disease in the general population.2–4 In up to 60% of patients the disease can be sporadic. Although the disease is inherited as an autosomal-dominant, there is a male predominance in its phenotype. It suggests-that gender- and age-related factors (eg, sex hormones) may play a role in triggering the arrhythmia in Brugada syndrome. The age of onset of clinical manifestations (syncope or cardiac arrest) is the third to fourth decade of life.5
ETIOLOGY AND PATHOPHYSIOLOGY
The ST-T wave changes in Brugada syndrome likely reflect a profound change in the process of ventricular repolarization. Three different theories have attempted to explain the syndrome: the depolarization theory, the repolarization theory, and the neural crest theory.6–8
DIAGNOSIS
The diagnosis of Brugada syndrome (BS) requires the presence of a type 1 BS pattern in the right precordial leads (ie, V1-V3), either spontaneous or unmasked by class I antiarrhythmic drugs (Table 55-1), characterized by a prominent coved ST-segment elevation displaying J-point amplitude or ST-segment elevation ≥2 mm, followed by a negative T wave. The type 2 BS pattern (≥2 mm J-point elevation, ≥1 mm ST-segment elevation, and a saddleback appearance, followed by a positive or biphasic T wave), and type 3 BS pattern (either a saddleback or coved appearance, but with an ST segment elevation <1 mm) are considered to be suggestive but not confirmatory of the disease (Figure 55-2).
TABLE 55-1 Drugs Used to Unmask Brugada Syndrome
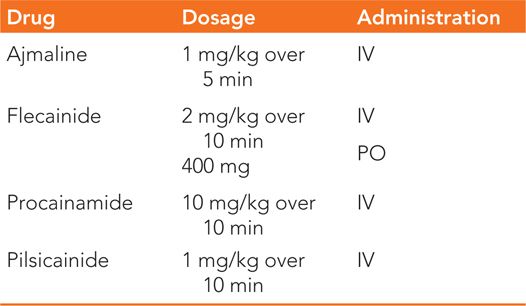
FIGURE 55-2 ECG patterns associated with Brugada syndrome. (A) Type 2 ECG (suspicious); (B) Type 1 ECG (diagnostic).
The diagnosis of BS is based on clinical diagnostic criteria (Table 55-2). Right bundle branch block may be associated with BS, but its presence is not required for the diagnosis (Figure 55-3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



