 Barrett’s oesophagus (intestinal metaplasia of oesophageal mucosal cells) with increased risk of cancer; this is a Th2-type immunological response (Ch. 38).
Barrett’s oesophagus (intestinal metaplasia of oesophageal mucosal cells) with increased risk of cancer; this is a Th2-type immunological response (Ch. 38).Control of gastric acid secretion
Acid secretion into the canaliculi of gastric parietal cells is initiated by the activity of a membrane-bound proton pump which exchanges H+ and K+ across the cell membrane (H+/K+-ATPase). Hydrogen ions are obtained from carbonic acid (H2CO3) by carbonic anhydrase, and HCO3− enters the plasma in exchange for Cl−. Chloride ions are then secreted into the stomach lumen with H+ via a symport carrier. The activity of the proton pump is influenced by several mediators, including histamine, gastrin and acetylcholine (Fig. 33.1).
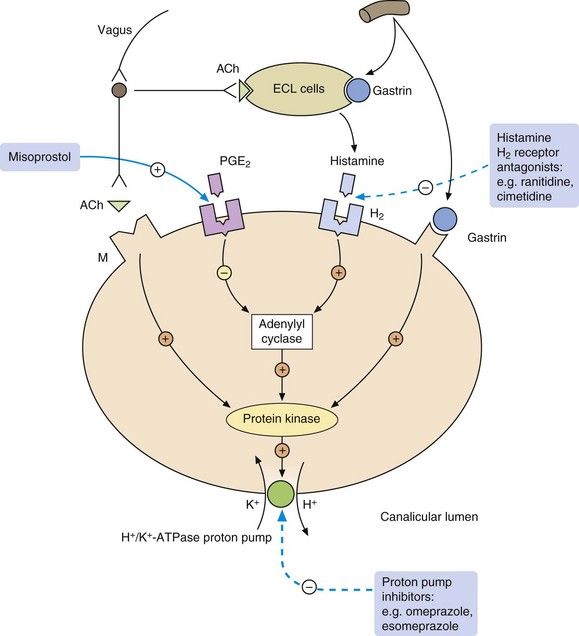
Fig. 33.1 Control of gastric acid secretion from the parietal cell.
Acid secretion from the parietal cell is stimulated by acetylcholine (ACh), histamine and gastrin. Gastrin and ACh also reinforce acid secretion by causing the release of histamine from the enterochromaffin-like (ECL) cells which lie close to the parietal cells in the gastric pits. Prostaglandin E2 (PGE2) reduces acid secretion. The sites of action of the main drugs used to inhibit acid secretion from the parietal cell are shown. There are no useful inhibitors of gastrin action, and the gastric-selective muscarinic receptor (M) antagonist pirenzepine is no longer available in the UK. H2, histamine type 2 receptor.
Drugs for treating dyspepsia, peptic ulcer and gastro-oesophageal reflux disease
It is only necessary to raise intragastric pH above 3 for a few hours each day to promote healing of most peptic ulcers. However, rapid healing requires acid suppression for a minimum of 18–20 h per day. The duration of acid suppression determines the rate of healing but not the eventual proportion of ulcers healed. Several classes of drug have antisecretory actions on the gastric mucosa.
Proton pump inhibitors
Mechanism of action: Since the proton pump (H+/K+-ATPase) is the final common pathway for acid secretion in gastric parietal cells, inhibition of the pump almost completely blocks acid secretion (Fig. 33.1). Proton pump inhibitors are irreversible inhibitors of H+/K+-ATPase and the return of acid secretion is dependent on the synthesis of new proton pumps. Proton pump inhibitors are weak bases that are selectively concentrated from the circulation into the acid environment of the secretory canaliculi of the gastric parietal cell. The drugs are then protonated and structurally transform into active derivatives that covalently bind to and irreversibly inhibit the proton pump. Because protonation to the active derivatives only takes place at acid pH, these drugs have a selective action on gastric cells, and proton pumps elsewhere in the body are not inhibited. Acid production is inhibited by about 90% for approximately 24 h following a single dose.
Pharmacokinetics: Proton pump inhibitors are prodrugs that are unstable in acid. They are given orally as enteric-coated formulations; esomeprazole, omeprazole and pantoprazole are also available as intravenous formulations. Elimination is by hepatic metabolism. They have short plasma half-lives (1–2 h) but, because of the irreversible mechanism of action, these bear no relationship to the long biological duration of action. Esomeprazole is the S-isomer of omeprazole that has lower clearance and therefore achieves slightly higher plasma concentrations.
 Omeprazole and esomeprazole are inhibitors of CYP2C9 and CYP2C19 in the liver. This can give rise to drug interactions with other substrates of these isoenzymes, for example decreasing the metabolism and increasing the clinical effects of warfarin, phenytoin and several antiviral drugs (see Table 2.7).
Omeprazole and esomeprazole are inhibitors of CYP2C9 and CYP2C19 in the liver. This can give rise to drug interactions with other substrates of these isoenzymes, for example decreasing the metabolism and increasing the clinical effects of warfarin, phenytoin and several antiviral drugs (see Table 2.7).Concerns that substantial reductions of gastric acid, and the associated rise in gastrin secretion, might increase the risk of gastric cancer (comparable to the increased risk in pernicious anaemia) appear to be unfounded. These drugs do not completely abolish acid secretion and intragastric pH can still fall below 4 during part of the day, the critical pH below which bacterial populations that predispose to cancer are thought not to become established. However, symptomatic improvement following treatment with a proton pump inhibitor can mask the symptoms of gastric cancer.
Histamine H2 receptor antagonists
Mechanism of action: Histamine H2 receptor antagonists act competitively at receptors on gastric parietal cells. They reduce basal acid secretion and pepsin production, and prevent the increase in secretion that occurs in response to several secretory stimuli. Overall, acid secretion is reduced by about 60% (Fig. 33.1).
Pharmacokinetics: Absorption of cimetidine and ranitidine from the gut is almost complete but both undergo limited first-pass metabolism. The drugs are mainly eliminated unchanged by the kidney, in part through active tubular transport. Their half-lives are between 1 and 4 h.
 Drug interactions: cimetidine is an inhibitor of hepatic P450 isoenzymes (see Table 2.7) and can increase the plasma concentrations and actions of drugs such as warfarin, phenytoin and theophylline.
Drug interactions: cimetidine is an inhibitor of hepatic P450 isoenzymes (see Table 2.7) and can increase the plasma concentrations and actions of drugs such as warfarin, phenytoin and theophylline.Antacids
Mechanism of action
Antacids neutralise gastric acid; magnesium salts do so much more rapidly than aluminium salts. They have a more prolonged effect if taken after food. If used without food, the effect lasts no more than an hour because of rapid gastric emptying. Antacids quickly produce symptom relief in peptic ulcer disease, but large doses are required to heal ulcers. Liquid preparations work more rapidly, but tablets are more convenient to use. Most antacids are relatively poorly absorbed from the gut. Simeticone is sometimes added to an antacid as an antifoaming agent. The combination may reduce flatulence, or relieve hiccups in palliative care.
Unwanted effects
 Constipation can occur with aluminium salts, and diarrhoea with magnesium salts; mixtures of aluminium and magnesium salts may have less effect on stool consistency.
Constipation can occur with aluminium salts, and diarrhoea with magnesium salts; mixtures of aluminium and magnesium salts may have less effect on stool consistency. In advanced renal failure, retention of absorbed aluminium may contribute to metabolic bone disease and encephalopathy. Magnesium salts can also cause toxicity, and the dose should be reduced in renal failure.
In advanced renal failure, retention of absorbed aluminium may contribute to metabolic bone disease and encephalopathy. Magnesium salts can also cause toxicity, and the dose should be reduced in renal failure.Antacids with alginic acid
Alginic acid is an inert substance. It is claimed that it forms a raft of high-pH foam which floats on the gastric contents and protects the oesophageal mucosa during reflux. All proprietary preparations combine alginic acid with an antacid, which is probably responsible for much of the clinical effect. Some formulations contain a high Na+ concentration and these should be used with caution in people with fluid retention or hypertension.
Cytoprotective drugs
Mechanism of action: Sucralfate is a complex of aluminium hydroxide and sucrose octasulphate. It dissociates in the acid environment of the stomach to its anionic form, which binds to the ulcer base. This creates a protective barrier to pepsin and bile and inhibits the diffusion of gastric acid. Sucralfate also stimulates the gastric secretion of bicarbonate and prostaglandins.
Bismuth salts
Mechanism of action: Bismuth salts precipitate in the acid environment of the stomach and then bind to glycoprotein on the base of an ulcer. The resulting complex adheres to the ulcer and has similar local effects to sucralfate. Bismuth salts, in combination with antibiotics, were the first effective anti-Helicobacter agents and this effect may have accounted for their ulcer-healing properties. They have now largely been superseded by proton pump inhibitor combinations for this purpose; however, when triple therapy with two antibacterials and a proton pump inhibitor fails, bismuth is included as part of the treatment regimen (see below).
Prostaglandin analogues
Mechanism of action: Misoprostol is an analogue of PGE1 and has several actions that protect the gastric and duodenal mucosae (see Ch. 29). Misoprostol limits the damage to superficial mucosal cells caused by agents such as acid and alcohol. It is most widely used to prevent NSAID-associated ulcers, and is available in combination products with diclofenac or naproxen (Ch. 29).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree













