Table 16-1. Classification of Lipids
Type | Classification |
| |
LDL cholesterol |
|
< 100 mg/dL | Optimal |
100–129 mg/dL | Near optimal or above optimal |
130–159 mg/dL | Borderline high |
160–189 mg/dL | High |
≥ 190 mg/dL | Very high |
| |
Total cholesterol |
|
< 200 mg/dL | Desirable |
200–239 mg/dL | Borderline high |
≥ 240 mg/dL | High |
| |
HDL cholesterol |
|
< 40 mg/dL | Low |
≥ 60 mg/dL | High |
| |
Triglycerides |
|
< 150 mg/dL | Normal |
150–199 mg/dL | Borderline high |
200–499 mg/dL | High |
≥ 500 mg/dL | Very high |
Diagnostic Criteria
Screening of adults > 20 years of age is recommended every 4–6 years in patients without ASCVD or diabetes and with LDL of 70–189 mg/dL. Children ages 2–8 should be screened if they have a family history of dyslipidemia or heart disease, or if the child has other risk factors for heart disease such as obesity, hypertension, diabetes, or exposure to cigarette smoke. Universal screening is recommended for all children ages 9–11. LDL levels in excess of 160 mg/dL may indicate a familial dyslipidemia.
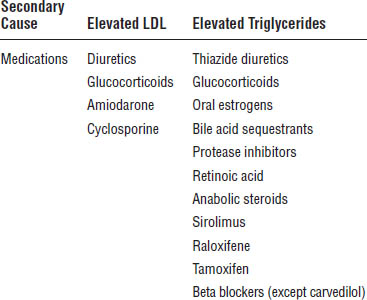
Secondary causes of dyslipidemia should be investigated. Common causes of elevated LDL are diet (excess saturated or trans fats, weight gain, anorexia), diseases (biliary obstruction, nephrotic syndrome), or disorders and altered metabolic states (hypothyroidism, obesity, pregnancy). Elevated TG may be caused by diet (weight gain, very low-fat diets, high intake of refined carbohydrates, excessive alcohol). See Table 16-2 for medication-related causes of dyslipidemia.
Familial hypercholesterolemia
Familial hypercholesterolemia (FH) is associated with a mutation in the LDL receptor gene, the apolipoprotein B (Apo B) gene, or the proprotein convertase subtilisin/kexin type 9 (PCSK9) gene. Patients who are homozygous for this mutation may have LDL cholesterol > 800 mg/dL in infancy, and those with heterozygous FH often have LDL cholesterol > 160 mg/dL. Cardiovascular mortality in patients age 20–39 is 100-fold that of the general population, if the condition is untreated. FH treatment in children should target LDL values < 130 mg/dL or a 50% LDL reduction with a high-intensity statin.
Table 16–2. Medications That Cause Dyslipidemia
Children and adolescents
Children age 8 and older with LDL levels > 190 mg/dL should be considered for medication therapy (> 160 mg/dL for children with family history of heart disease or more than two other risk factors and > 130 mg/dL for children with diabetes). First-line medication options include bile acid sequestrants, cholesterol absorption inhibitors, and statins. Niacin products are not recommended for children, and fibrates should be used with caution and under the supervision of a pediatric lipid specialist.
Children age 2 and older who are overweight or obese and who have a high TG level or low HDL level should receive a recommendation of weight management and increased physical activity as the primary treatment.
Clinical Presentation
Dyslipidemias are usually asymptomatic, except in some familial lipid disorders in which patients may develop cutaneous manifestations of lipid deposition (e.g., tendon xanthomas, planar xanthomas, xanthelasmas, and eye manifestations [corneal arcus]).
Treatment Principles
Prior to November 2013, the Adult Treatment Panel (ATP) III (published in 2001) and Update to ATP III (published in 2004) served as the standard of care for lipid management. Within these guidelines, assessment of risk factors and titration of medication therapy to target LDL levels were the mainstay of treatment. In 2013, the American College of Cardiology/American Heart Association (ACC/AHA) issued updated recommendations for the treatment of blood cholesterol that were markedly different from previous guidelines. Though ACC/AHA explicitly stated that these were not meant to be a comprehensive guide to lipid management, they are a recommendation for treatment of lipids using fixed-dose statins to prevent ASCVD.
ASCVD is defined as follows:
■ Acute coronary syndromes
■ Myocardial infarction
■ Stable or unstable angina
■ Coronary or other arterial revascularization
■ Stroke or transient ischemic attack (TIA)
■ Peripheral arterial disease
Consider potential ASCVD risk and benefit, taking into consideration adverse effects, drug–drug interactions, and patient preferences for statins.
Lifestyle modification
All patients with dyslipidemia should undertake lifestyle modifications. For the purposes of ASCVD prevention, the 2013 ACC/AHA guidelines recommended the Dietary Approaches to Stop Hypertension (DASH) diet because evidence shows that it can reduce the risk of ASCVD. The DASH diet consists of dietary intake patterns that emphasize vegetables, fruits, whole grains, low-fat dairy products, poultry, fish, legumes, nontropical vegetable oils, and nuts. Intake of sweets, sugar-sweetened beverages, and red meats should be limited. Daily intake from saturated fats should be 5–6% of total calories. Sodium in the diet should be limited to no more than 2,400 mg/day, with reduction to 1,500 mg sodium/day producing the maximum blood pressure reduction. Exercise should consist of moderate to vigorous aerobic activity 3–4 times per week, lasting an average of 40 minutes per session.
Other dietary interventions that can lower LDL cholesterol (but are not included in the new recommendations) include viscous fiber (10–25 g/day) and plant stanols or sterols (2 g/day). Plant sterols and stanols interfere with micellar absorption of cholesterol. Viscous fiber, found in oats, pectin, and psyllium, also interferes with cholesterol absorption. Soy protein (25–40 g/day), when replacing animal food products, can also lower cholesterol. Though there is less evidence to support such measures in ASCVD prevention in adults, these dietary interventions are still recommended for children and adolescents who do not achieve their LDL goals.
Risk evaluation
The Pooled Cohort Risk Score takes into account age, gender, race (non-Hispanic white or African American), total cholesterol, HDL cholesterol, systolic blood pressure, blood pressure medication use, diabetes, and smoking status to determine a percent risk for an atherosclerotic event at 10 years. The equation may be used for other ethnic groups; however, it may underestimate risk in subgroups such as Native Americans, South Asians, and Puerto Ricans and overestimate risk for East Asians and Mexican Americans. Cut-points of ≥ 7.5.% or < 7.5% have been established to guide therapy.
Treatment
Patients are stratified by presence or absence of existing ASCVD disease, baseline LDL level, presence of diabetes, and age. See Table 16-3 to delineate statin therapy for patients with associated risk. Four major benefit groups are outlined.
Though these statin benefit groups are identified, patients may not completely fit into one of the categories. The following risk factors should also be considered when evaluating individual patient risk:
■ Primary LDL > 160 mg/dL or other evidence of genetic dyslipidemia
■ Family history of premature ASCVD onset (< 55 years of age in a first-degree male relative, < 65 years of age in a first-degree female relative)
■ High-sensitivity C-reactive protein
■ Coronary artery calcium (CAC) score > 300 Agatston units or ≥ 75th percentile for age, gender, and ethnicity
■ Ankle-brachial index < 0.9
■ Elevated lifetime risk of ASCVD.
16-4. Drug Therapy
Prior to initiation of therapy, a baseline fasting lipid panel (FLP) should be obtained and then reevaluated at 4–12 weeks to assess adherence. Following this initial test, FLP should be assessed every 3–12 months to assess adherence and response to treatment. Other laboratory parameters specific to each medication will be included separately.
HMG-CoA Reductase Inhibitors (statins)
These agents competitively inhibit HMG-CoA (3-hydroxy-3-methyl-glutaryl-coenzyme A) reductase, which is the enzyme responsible for conversion of HMG-CoA to mevalonate.
Mevalonate is an early precursor to and a rate-limiting step in cholesterol synthesis. This reduction in liver cholesterol synthesis results in upregulation of liver LDL receptors and increased clearance of LDL and VLDL particles in the blood. These actions induce a decrease in total cholesterol and LDL cholesterol, promote a slight increase in HDL cholesterol, and effect a modest decrease in TG.
Monitoring
■ Conduct baseline liver function tests (LFTs), A1c, thyroid function tests (thyroid-stimulating hormone [TSH] tests), serum creatinine (SCr), and creatine phosphokinase (CPK) in patients with a personal or family history of muscle side effects from statins.
Table 16-3. Reduction of ASCVD Risk with Statins: Daily Doses and Associated Risk Categories
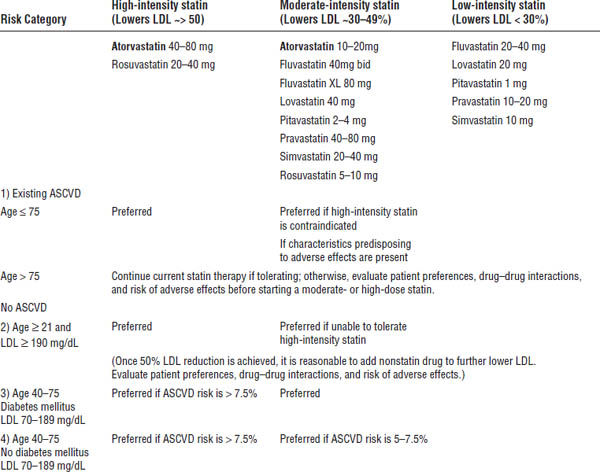
Boldface indicates one of top 100 drugs for 2012 by units sold at retail outlets, www.drugs.com/stats/top100/2012/units.
■ LFTs should be repeated only when clinically indicated.
■ CPK needs to be monitored only if the patient has suspected muscle damage.
■ Patients with LDL cholesterol < 40 mg/dL on two separate readings should have their statin dose decreased.
Dosage and administration
See Tables 16-4 and 16-5 for detailed information regarding dosing.
Short-acting statins (pravastatin, simvastatin, fluvastatin) are administered at bedtime because most hepatic cholesterol production occurs overnight. Atorvastatin, rosuvastatin, and pitavastatin may be given any time of the day because of their longer half-life. Lovastatin conventional tablets should be given with the evening meal because absorption is better with food; however, the extended-release lovastatin products should be taken at bedtime. The lovastatin plus Niaspan combination product should be taken at bedtime with a low-fat snack. Administration of simvastatin 80 mg is limited to patients who have been taking this dose for ≥ 12 consecutive months without evidence of myopathy. Initiation of simvastatin 80 mg is no longer recommended because of risk of myopathy. All statins are approved for use in children ages 10–18. Only pravastatin is approved for children ≥ 8 years of age. Doubling the dose of statin lowers LDL levels only by an additional 6%.
Table 16–4. Statin Dosing Considerations
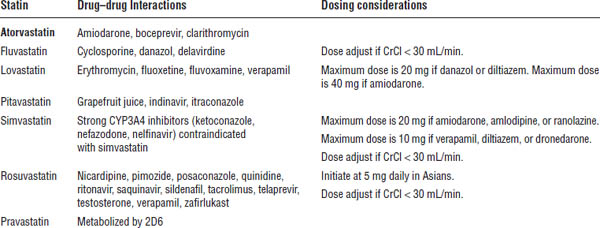
Boldface indicates one of top 100 drugs for 2012 by units sold at retail outlets, www.drugs.com/stats/top100/2012/units.
Table 16-5. Drug Products and Dosage
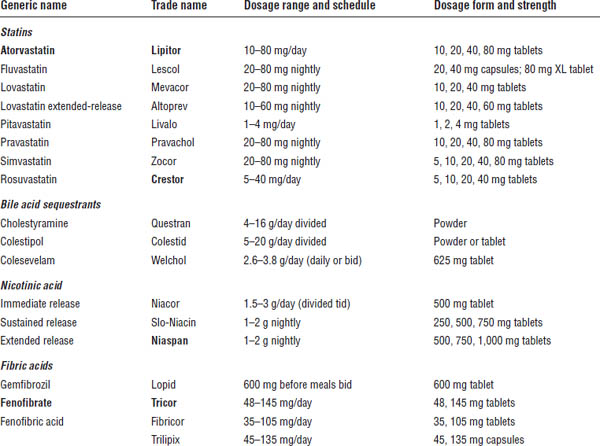
Boldface indicates one of top 100 drugs for 2012 by units sold at retail outlets, www.drugs.com/stats/top100/2012/units.
a. Aspirin tablets and pravastatin tablets are separate tablets within the Pravigard PAC.
Adverse effects
■ Myopathy (muscle damage) may occur.
■ Myalgia (muscle pain, soreness, or tenderness) may occur.
■ Myositis occurs in 0.2% of patients. Myositis is myalgia combined with CPK elevated 3–10 times the upper limit of normal (ULN).
■ Rhabdomyolysis occurs rarely, but it can cause acute renal failure. The statin or other offending drug should be discontinued immediately. Rhabdomyolysis is the combination of severe muscle symptoms plus CPK elevated 10 times the ULN with increased serum creatinine and urine myoglobin.
■ Elevated liver enzymes occur in 0.1–2.3% of patients.
■ Cognitive impairment, such as memory loss, forgetfulness, and confusion, has been reported by some statin users.
■ Statins may be associated with a slightly increased rate of incident type 2 diabetes.
■ Flu-like symptoms and headache may occur.
■ Patients may have mild gastrointestinal (GI) complaints.
■ Active liver disease is a contraindication to statin therapy; caution should be used in patients with chronic liver disease or unexplained elevations in transaminases (> 3 × ULN). Statins may be beneficial in fatty liver disease.
Drug interactions
See Table 16-4 for dosing considerations with statins. Patients taking pitavastatin who are also taking erythromycin should not take more than 1 mg/day of pitavastatin. Patients taking pitavastatin who are also taking rifampin should not take more than 2 mg/day of pitavastatin. Dosing of simvastatin 80 mg should be avoided except in patients who have been stable on this dose for the past 12 months.
Bile Acid Sequestrants (Resins)
Nonabsorbable anion exchange resins exchange chloride ions for bile acids and other anions in the intestine. This action inhibits enterohepatic recycling, which results in bile excretion and a decrease in the cholesterol pool in the liver. LDL receptors are upregulated, increased LDL is cleared, and LDL is lowered.
Monitoring
■ Evaluate baseline FLP for hypertriglyceridemia:
• If TG > 200 mg/dL, use resins with caution.
• If TG > 400 mg/dL, resins are contraindicated.
Dosing and administration
Cholestyramine and colestipol should be titrated slowly to avoid GI side effects. They may be started with one dose daily with the largest meal. They may be increased (after the patient adjusts to the resin) to two doses daily with the largest meals or divided between breakfast and dinner. Powdered doses can be mixed with food such as soup, oatmeal, nonfat yogurt, and applesauce. The mixture can also be chilled overnight to improve palatability. To prevent constipation, resins may be mixed with psyllium; however, this mixture should be ingested immediately after mixing to prevent a gel from forming. Counsel the patient to rinse the glass and drink the remains to ensure ingestion of all resin. Colesevelam is a tablet formulation, which may be easier for some patients to self-administer. However, the tablets are large, and some patients may not be able to swallow them. Separate other medications 1 hour before and 4 hours after administration to prevent binding of medications.
Adverse effects
■ GI distress may occur.
■ Patients may experience palatability problems with the resin slurry.
■ Constipation may occur that increases with the dose and in the elderly.
■ Decreased absorption of other drugs may occur. Dose other drugs 1 hour before or 4 hours after ingestion of resin.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



