Dyshormonogenetic Goiter
Vania Nosé, MD, PhD
Key Facts
Terminology
Familial goiter that develops from defect in the metabolism of thyroid hormone secondary to an inherited disorder
Etiology/Pathogenesis
Multiple inherited biochemical defects lead to decreased thyroid hormone synthesis
Resultant alterations in thyroid gland homeostasis, disturbance of feedback system, and chronic TSH stimulation lead to enlarged thyroid glands or goiters
Clinical Issues
2nd most frequent cause of permanent congenital hypothyroidism after thyroid dysgenesis, including aplastic and hypoplastic thyroid disorders
May be associated with nerve deafness (Pendred syndrome)
Macroscopic Features
Thyroid gland is enlarged asymmetrically
Cut surface is firm and tan with nodules of varying size, which may be up to a few centimeters in diameter
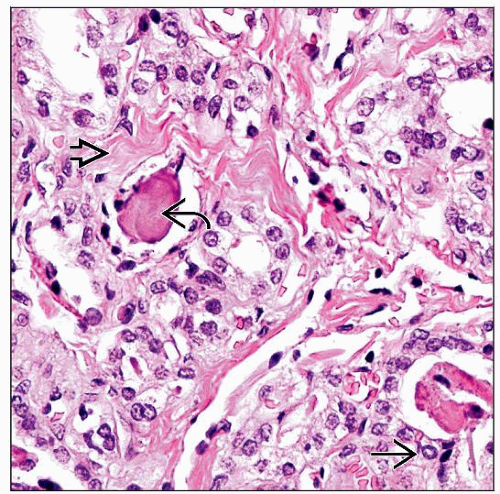
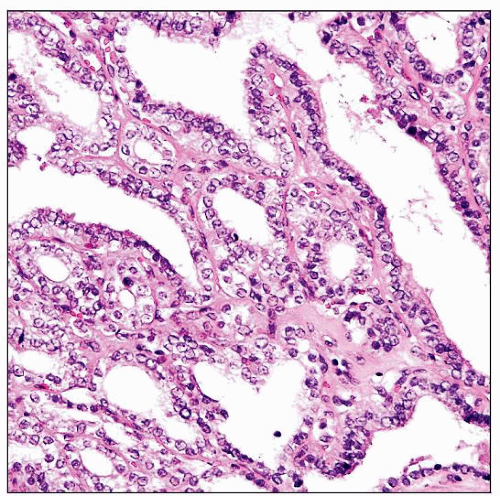
Microscopic Pathology
When present, colloid frequently has pale, washed-out appearance
Extensive fibrosis in internodular tissue may simulate true capsular invasion
Nuclear abnormalities consist of enlarged, irregularly shaped, hyperchromatic and vesicular nuclei
Colloid is usually absent
TERMINOLOGY
Abbreviations
Dyshormonogenetic goiter (DHG)
Synonyms
Inherited goiter
Definitions
Familial goiter that develops from defect in metabolism of thyroid hormone secondary to an inherited disorder
ETIOLOGY/PATHOGENESIS
Developmental Anomaly
Multiple inherited biochemical defects, which lead to decreased thyroid hormone synthesis
Resulting alterations in thyroid gland homeostasis, disturbance of feedback system, and chronic TSH stimulation lead to enlarged thyroid gland or goiters
Known Genetic Etiologies
Deficiencies may be present in multiple steps of thyroid hormone synthesis
Thyroglobulin synthesis
Iodine transport (into and out of follicular cell)
Iodine oxidation
Organification of thyroglobulin
Coupling and dehalogenation of iodotyrosine compounds
Breakdown of thyroglobulin
Pendred Syndrome
Familial syndrome in which patient has DHG and familial deaf-mutism from sensorineural deafness
Mutations in the PDS/SLC26A4 gene (pendrin)
This gene encompasses 21 exons and contains an open reading frame of 2,343 base pairs
CLINICAL ISSUES
Epidemiology
Incidence
2nd most frequent cause of permanent congenital hypothyroidism after thyroid dysgenesis, including aplastic and hypoplastic thyroid disorders
Prevalence of 1 in 30,000-50,000 live births in Europe and North America
Site
Thyroid is diffusely involved as this is a constitutional genetic condition
Presentation
Goiter is not usually present at birth but appears later in life
75% of goiters develop before 24 years of age (average age: 15 years)
Ranges from neonates to adults (only the most severe inherited mutations result in infant presentation)
Patients usually present with clinical evidence of goiter although sometimes diagnosis is made at autopsy
May be associated with nerve deafness (Pendred syndrome)
Slight predilection for female gender
Family history of hypothyroidism or goiter is reported in ˜ 20% of patients
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree