Dyshormonogenetic Goiter
Lester D. R. Thompson, MD
Key Facts
Terminology
Thyroid enlargement due to hereditary defect in thyroid hormone synthesis
Clinical Issues
Usually autosomal recessive, enzyme defect in one of the biochemical steps of thyroid hormone synthesis
Congenital hypothyroidism: 1 in 3,000-4,000 births
About 15% due to dyshormonogenetic goiter
Average age at presentation: 16 years
Absent or severely decreased thyroid hormone synthesis
Low to absent T4 and T3, with high TSH
Treatment of hypothyroidism is primary goal, using surgery for symptomatic goiter
Macroscopic Features
Thyroid is enlarged, asymmetric, and nodular, resembling adenomatoid nodules
Microscopic Pathology
All thyroid tissue is abnormal
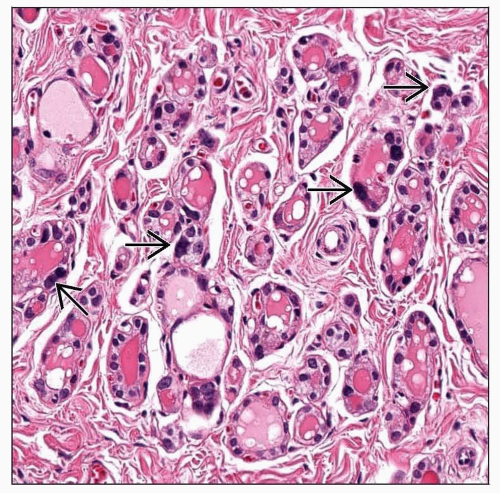
Nodules vary considerably but hypercellular with scant/absent colloid
Pleomorphism highlighted or accentuated in cells between nodules
In fibrous septae or internodular parenchyma
Top Differential Diagnoses
Adenomatoid nodules, diffuse hyperplasia (Graves disease), radiation thyroiditis, follicular carcinoma, iatrogenic goiter
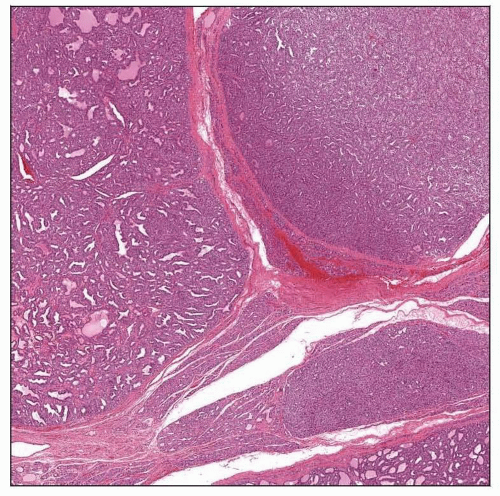 The thyroid gland is asymmetric and nodular, with the nodules resembling adenomatoid nodules. There is colloid present, although it is not prominent. The nodules are cellular. |
TERMINOLOGY
Synonyms
Inherited goiter
Definitions
Thyroid enlargement due to hereditary defect in thyroid hormone synthesis
ETIOLOGY/PATHOGENESIS
Developmental Anomaly
Genetic defect in one of the biochemical steps of thyroid hormone synthesis
Usually autosomal recessive
Several major enzyme defects are known
Loss of any of genes involved in thyroglobulin synthesis, iodine transport, iodide oxidation and organification, coupling of MIT and DIT, proteolytic breakdown of thyroglobulin, and iodide recycling
Deficiency in thyroperoxidase (TPO) activity is most frequent cause of dyshormonogenetic goiter
CLINICAL ISSUES
Epidemiology
Incidence
Very rare cause of permanent congenital hypothyroidism
2nd most frequent cause of permanent congenital hypothyroidism
Congenital hypothyroidism (thyroid dysgenesis): 1 in 3,000-4,000 births
About 15% due to dyshormonogenetic goiter
Prevalence of dyshormonogenetic goiter: 1 in 30,000-50,000 population
Age
Average age at presentation: 16 years
Majority manifest before age 25 years
Ranges from neonates to adults
Gender
Female slightly > Male
Site
Entire thyroid gland affected
Whenever “whole thyroid” is affected, must consider genetic or autoimmune etiologies
Presentation
Absent or severely decreased thyroid hormone synthesis
Results in increased secretion of TSH due to functional hypothyroidism
Insufficient hormone production for feedback loop
Insufficient hormone production results in continuous TSH stimulation
Yields thyroid hyperplasia without thyroid function improvement
Only patients with most severe impairment in thyroid hormone production present in infancy with cretinism
Most patients (2/3) have known hypothyroidism prior to recognition of goiter
Thyroid enlargement (goiter) tends to develop later in life
Family history of hypothyroidism &/or goiter is elicited in 20% of patients
Pendred syndrome very rare (SLC26A4 at 7q31)
Association of dyshormonogenetic goiter (impaired iodide organification) with familial deaf-mutism due to sensorineural deafness
Biallelic mutations in SLC26A4 gene
SLC26A4 gene encompasses 21 exons and contains open-reading frame of 2343 bp
Natural History
If severe or complete, cretinism at birth
Death without replacement therapy