Duodenum-Preserving Partial, Subtotal, and Total Resection of the Pancreatic Head in Chronic Pancreatitis and Neoplastic Cystic Lesions
Hans G. Beger
Bettina M. Rau
Bertram Poch
In Western countries, alcohol is the most frequent etiologic factor causing chronic pancreatitis. Approximately 90% of the patients with alcoholic chronic pancreatitis suffer a severe abdominal pain syndrome. In alcoholic chronic pancreatitis, and in tropical, nutritional chronic pancreatitis in Asian countries as well, an inflammatory mass in the head of the pancreas is frequently found in combination with local complications. As a consequence of the chronic inflammatory process, a loss of the endocrine and exocrine parenchyma takes place, replaced locally by extracellular matrix tissue resulting in fibrosis. The molecular and pathobiochemical mechanisms causing inflammation and fibrosis are largely unknown. Pathomorphologically, common features are pancreatic main duct and side branch stenoses and dilations, focal necrosis, and extensive infiltration of leukocytes and immunocytes. Overexpressions of epidermal growth factor, transforming growth factor-β, and acidic and basic fibroblast growth factor, as well, are considered to be crucial for production of extracellular matrix substances.
Pain in chronic pancreatitis is related to increased duct and tissue pressure in the pancreas. Pathomorphologic changes in sensory intrapancreatic nerves, which have been observed being increased in diameter, perineural infiltration of inflammatory cells, and increased levels of neurotransmitter substances are causally related to the pain syndrome. In long-term follow-up studies, the natural course of chronic pancreatitis after diagnosis reveals persistence of pain in 85% of the patients after 5 years and in 55% after 10 years.
The progression of exocrine and endocrine insufficiency, which is frequently observed in chronic pancreatitis, has a limited influence on the pain syndrome and results in only a subgroup of patients in the final burned-out syndrome. Local complications, for example, pseudocystic lesions, inflammatory mass in the head, common bile duct stenosis, compression or occlusion of the portal, superior mesenteric respectively splenic vein, and narrowing of the periampullary duodenum, are frequently observed. A coexistence of chronic pancreatitis and pancreatic cancer developing years after the diagnosis of chronic pancreatitis is observed, on the basis of epidemiologic studies, in 1.8% to 5.0% of the patients, and for extrapancreatic cancers, in 3.9% to 13.0% patients. The death rate related to chronic pancreatitis is between 12% and 20%. Ten years after diagnosis and treatment of chronic alcoholic pancreatitis, the death rate caused by complications of chronic pancreatitis and continuing alcohol abuse is ∼,30%.
Diagnosis of chronic pancreatitis is based on contrast-enhanced computed tomography (MD-CT) as the “gold standard.” Endoscopic retrograde cholangiopancreatography or magnetic resonance cholangiopancreatography provides additional information about the duct changes, including the main pancreatic duct and side branches and the intrapancreatic segment of the common bile duct. In ∼30% to 50% of the patients suffering from advanced chronic pancreatitis, the intrapancreatic segment of the common bile duct shows a prepapillary stenose. To evaluate the endocrine and exocrine function, an oral glucose tolerance test, a pancreolauryl test, a secretin stimulation test, or a fecal chymotrypsin estimation has to be performed.
Until now, there has been no preventive therapy for chronic pancreatitis. Except for avoidance of alcohol consumption, medical management has a supportive role in terms of analgesic treatment, supplementation with exogenous enzyme substitutes, and treatment of diabetes mellitus. Medically intractable pain and the development of severe local complications are reasons to change from medical management to surgical treatment (Table 1).
The surgical technique of subtotal/total pancreatic head resection includes three principal technical steps (Table 2).
Table 1 Indications for Duodenum-Preserving Subtotal/Total Pancreatic Head Resection | ||
|---|---|---|
|
Exposure of the Pancreatic Head
The head of the pancreas is exposed, dividing the gastrocolic and duodenocolic ligaments, preserving the gastroepiploic vessels. Subsequently, the duodenum is mobilized by a Kocher maneuver. After identification of the superior mesenteric vein at the lower margin of the pancreatic head, preparation of a tunnel between the portal vein and the pancreatic neck has to be performed.
Table 2 Surgical Steps of Subtotal/Total, Duodenum-Preserving Resection of the Head of the Pancreas in Chronic Pancreatitis | |||
|---|---|---|---|
|
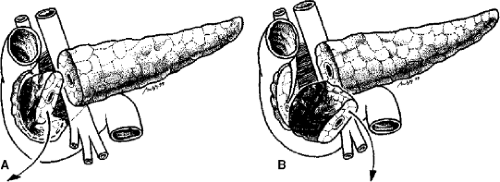
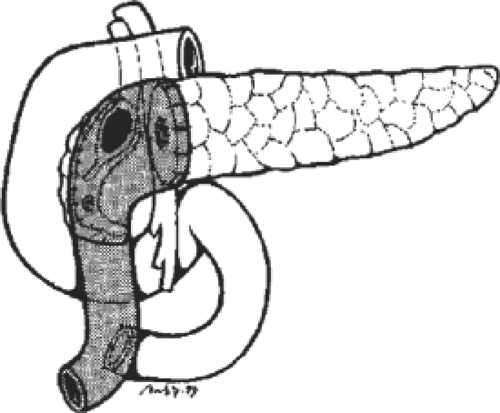
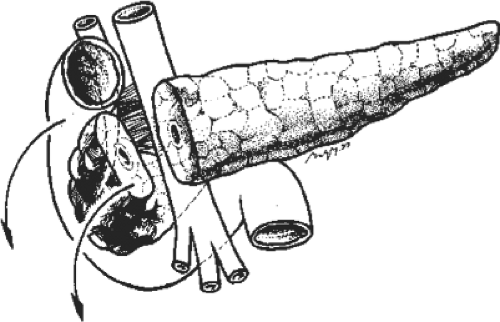 Fig. 2. After completion of the transection of the pancreatic neck, the pancreatic head is rotated into the ventrodorsal axis (upward) for subtotal resection. |
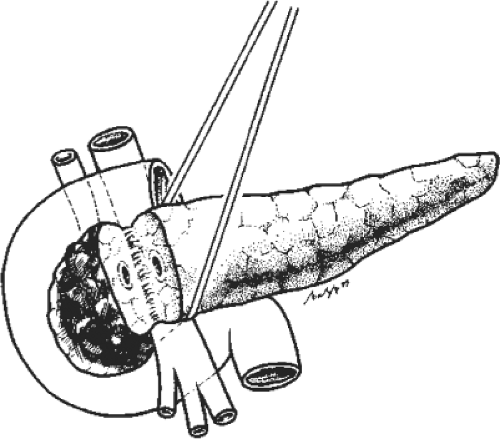
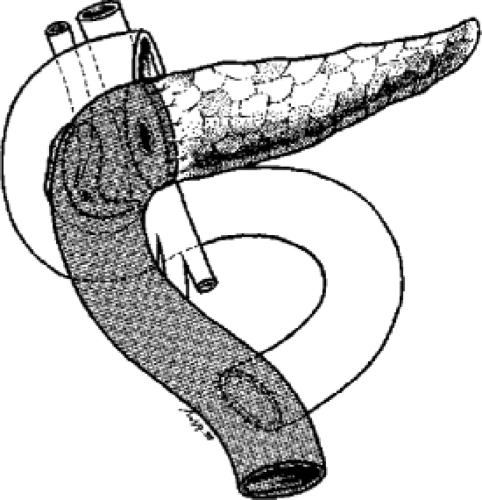
Even in cases of extensive inflammation, the tunneling can be performed without major difficulties. The identification and looping of the common hepatic artery is carried out on the upper margin of the neck and head of the pancreas. The common bile duct is identified and banded with a rubber loop in the hepatoduodenal ligament (Fig. 1).
Subtotal Head Resection
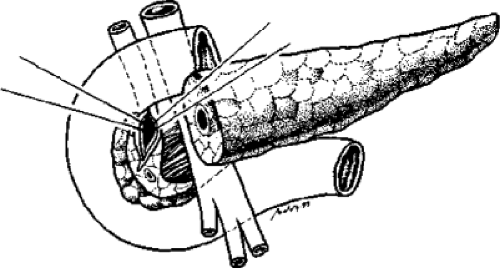
Resection of the inflammatory mass in the pancreatic head is initiated with a transverse division of the pancreatic neck at the duodenal edge of the portal vein (Fig. 1). At the cut surface of the left pancreas, meticulous hemostasis using monofilament 5-0 to 6-0 nonabsorbable sutures is carried out. The head of the pancreas is rotated forward and to the right (Fig. 2). This can be achieved easily by bluntly freeing the head of pancreas from the portal vein; small branches entering the portal vein and superior mesenteric vein are ligated. The head of the pancreas is removed, using a knife, from the retroperitoneal surface of the pancreas toward the uncinate process without major technical difficulties (Fig. 3A). The subtotal resection of the pancreatic head is completed by including the tissue of the uncinate process and excising the pancreatic head tissue at a distance of 5 mm from the duodenal wall. The wet weight of the operative specimen after subtotal pancreatic head resection lies between 25 and 50 g. It has not proved necessary to preserve the gastroduodenal artery for ensuring an optimal blood supply to the duodenal wall because the supraduodenal vessels, the dorsal pancreaticoduodenal arcades, and the mesoduodenal vessels maintain the blood supply. The dissection of the intrapancreatic segment of the common bile duct is started at the upper margin of the pancreatic head (Fig. 3B). In most cases, decompression of the common bile duct can be achieved by dissecting the pancreatic tissue along the common bile duct wall. The dorsal capsula of the pancreatic head is preserved.
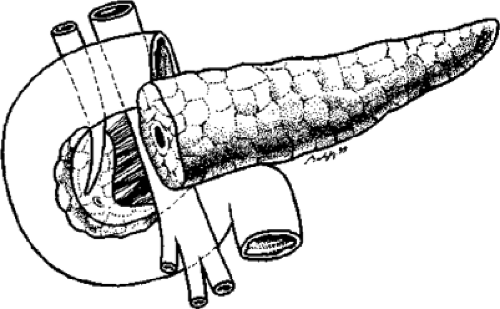
In cases with an inflammatory process in the wall of the common bile duct causing duct narrowing, the duct is opened by excising a 15 × 5 mm wall segment (Fig. 4). After completion of the subtotal resection of the pancreatic head, a shell-like, 5 to 8 mm wide remnant of the tissue of the pancreatic head is left connected to the duodenal wall (Fig. 5). Meticulous suturing of any bleeding vessels using 5-0 to 6-0 nonabsorbable suture material is recommended.
Reconstruction
Reconstruction is executed by dissecting the most proximal jejunal loop 20 cm distally to the ligament of Treitz. The aboral jejunal loop is transposed via a retrocolic mesenteric opening to the pancreatic head, and an end-to-end anastomosis using a two-layered technique is fashioned between the pancreatic neck and the jejunal loop (Fig. 6). In patients with a dilated main pancreatic duct and multiple fibrotic duct stenoses, the main pancreatic duct is incised longitudinally at its anterior surface up to the tail of the pancreas. In these patients, the anastomosis is performed as a side-to-side anastomosis, as a Partington–Rochelle modification of drainage of the main pancreatic duct (Fig. 7). A single- or double-layer suture between the jejunum and the residual head of the pancreas along the excision line has to be carried out at a distance of 5 to 8 cm from the anastomosis with the left pancreas.
An additional anastomosis between the common bile duct and the jejunal loop is not mandatory. The opening of the common bile duct is included in the pancreatic anastomosis, which is carried out with the remnant of the pancreatic head (Figs. 7 and 8).
For restoration of the food transit, a typical Roux-en-Y anastomosis is sutured 20 cm distal to the pancreaticojejunal anastomosis (Fig. 8).
In patients with severe stenosis of the duodenum, dissection of the tissue at the ventral surface of the duodenum, causing
encasement of the duodenum, has to be carried out. The stenosis is caused by fibrous tissue bands at the ventral wall of the suprapapillary duodenum. Removal of the fibrous layers up to the level of the serosa results in restoration of a normal diameter of the duodenum. The subtotal resection of the pancreatic head brings about in decompression of the portal vein and an immediate release of the signs of portal hypertension.
encasement of the duodenum, has to be carried out. The stenosis is caused by fibrous tissue bands at the ventral wall of the suprapapillary duodenum. Removal of the fibrous layers up to the level of the serosa results in restoration of a normal diameter of the duodenum. The subtotal resection of the pancreatic head brings about in decompression of the portal vein and an immediate release of the signs of portal hypertension.
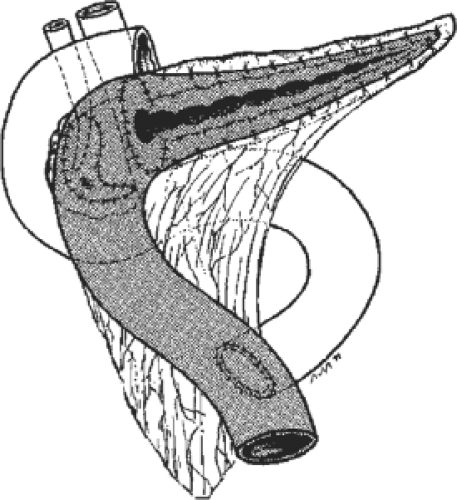 Fig. 7. In cases of multiple pancreatic main duct stenoses, a Partington–Rochelle modification of a drainage procedure between the jejunal loop and the left pancreas is carried out. |
Results After Subtotal Duodenum-Preserving Pancreatic Head Resection
Clinical observations and immunologic and molecular biologic data underline the hypothesis that the pancreatic head is the pacemaker of chronic pancreatitis. The subtotal duodenum-preserving resection of the pancreatic head results in relief of local complications. The coring-out technique of Frey is a modification of the Partington–Rochelle duct drainage procedure resulting in duct decompression, but it conserves the inflammatory tissue mass of the pancreatic head if only 6 g of pancreatic head tissue is excised. In comparison to Whipple resection and pylorus-preserving pancreaticoduodenectomy, the subtotal duodenum-preserving pancreatic head resection offers the major advantage of preserving the extrahepatic biliary tree, stomach, and duodenum. In five randomized controlled clinical trials, the superiority of the duodenum-preserving technique compared to Whipple resection or pylorus-preserving resection has been demonstrated for the patients suffering from advanced chronic pancreatitis. In terms of hospital death rates, frequency of relaparotomy, and complications as well, the subtotal pancreatic head resection offers the major advantage of low postoperative morbidity (Table 3).
Table 3 Subtotal, Duodenum-Preserving Pancreatic Head Resection in Chronic Pancreatitis: Early Postoperative Results
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|
|---|