Ductal Adenocarcinoma, including Variants
Mari Mino-Kenudson, MD
Key Facts
Terminology
Adenocarcinoma arising in pancreatic ductal system
Comprises 85-90% of all pancreatic neoplasms
Clinical Issues
Most cases unresectable at presentation
Nonspecific symptoms often mean delay in diagnosis
Macroscopic Features
Majority in head of pancreas
Poorly defined, firm mass with intense fibrotic reaction
Carcinoma may be difficult to distinguish from background pancreatitis
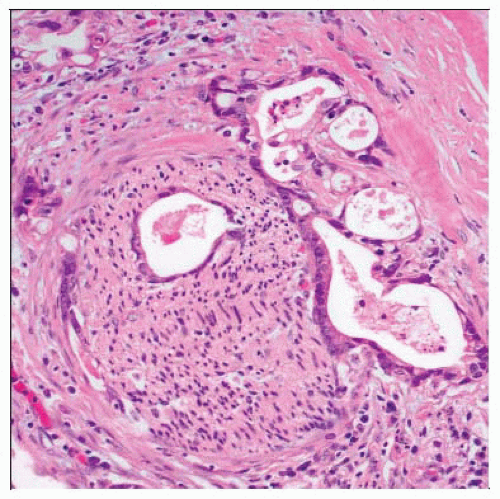
Microscopic Pathology
Small, haphazardly infiltrating glands embedded in dense desmoplastic stroma
Perineural and angiolymphatic invasion and associated chronic pancreatitis are very common
Many histologic patterns and variants
Foamy gland pattern
Clear cell pattern
Colloid carcinoma
Adenosquamous
Immunopositive for many antigens
Cytokeratins 7, 8, 18, 19
CEA, CA19-9, CA125, B72.3
MUC1, MUC4, MUC5AC, and MUC6 (25%)
TERMINOLOGY
Abbreviations
Pancreatic ductal adenocarcinoma (PDAC)
Synonyms
Pancreatic adenocarcinoma
Duct cell adenocarcinoma
Definitions
Malignant epithelial neoplasm arising in pancreatic ductal system
85-90% of all pancreatic neoplasms
Predominantly glandular differentiation
ETIOLOGY/PATHOGENESIS
Hereditary Risk Factors
Family history of pancreatic cancer
Hereditary pancreatitis
Peutz-Jeghers syndrome
Familial atypical multiple mole melanoma syndrome
BRCA2 and BRCA1 mutations
Medical Risk Factors
Chronic pancreatitis
Diabetes mellitus
Previous cholecystectomy or partial gastrectomy
Environmental and Occupational Risk Factors
Cigarette smoking approximately doubles risk
Diet high in meat, fat, nitrates, and pork products increases risk
Obesity
Chemicals (solvents, DDT, gasoline)
Occupational (coal gas workers, metal working, hide tanning, dry cleaning)
Precursor Lesions
Pancreatic intraepithelial neoplasia
CLINICAL ISSUES
Epidemiology
Age
Peak incidence in 7th and 8th decades of life
Rare before age 40
Majority of cases occur between age 60-80
Gender
More common in men than in women (1.3:1)
Ethnicity
More common in Maoris, native Hawaiians, and African-Americans in USA
Presentation
Very nonspecific symptoms may result in delay in diagnosis
Epigastric pain radiating to the back
Weight loss
Painless jaundice
Signs of biliary obstruction
Disease associations
Trousseau syndrome (migratory thrombophlebitis)
Diabetes mellitus
Sister Mary Joseph sign (palpable periumbilical nodules)
Courvoisier sign (distended, palpable gallbladder)
Treatment
Resection
Only 10-20% of cases resectable at diagnosis
Chemotherapy before resection, after resection, or both
Gemcitabine seems most promising
Prognosis
Dismal
Overall 5-year survival less than 5%
IMAGE FINDINGS
General Features
CT scan is most commonly used radiological method for diagnosis and staging
Magnetic resonance angiography can be used to examine vascular anatomy and determine resectability
Endoscopic ultrasound also very reliable for diagnosis and staging
ERCP/MRCP help visualize ductal system
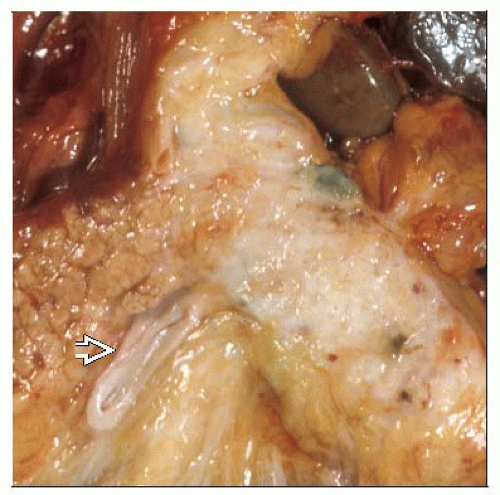
MACROSCOPIC FEATURES
General Features
Majority in head of pancreas
Minority in body or tail
Minority diffusely involves whole gland
Solitary (majority) or multifocal
Firm, solid, poorly defined, white-yellow mass
May have cystic degeneration
Usually intense fibrotic reaction
May make carcinoma difficult to distinguish from background pancreatitis
Pancreatic duct may be dilated
May cause stenosis of common bile duct
Tumors often grossly extend beyond pancreas
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree