Drugs Used in Disorders of the Respiratory System
Overview
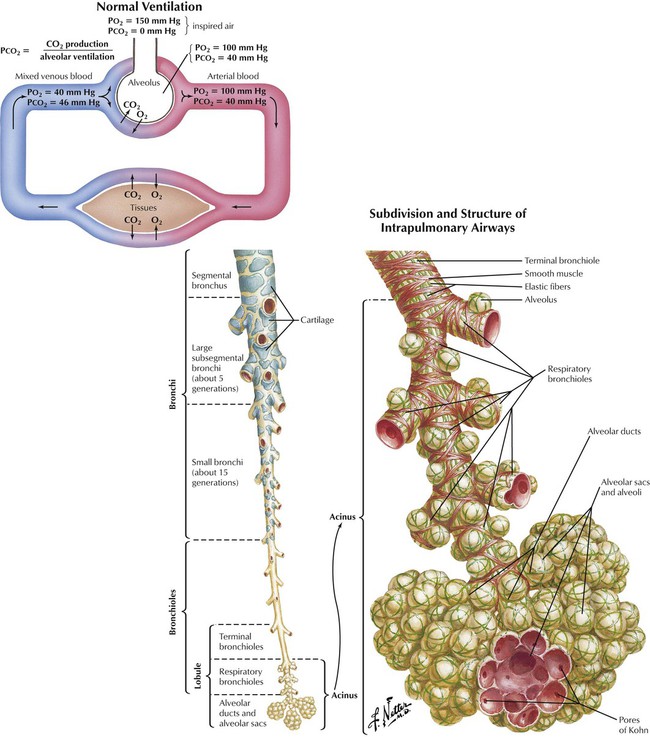
Respiration means ventilation, or breathing. The 2 phases of breathing are inspiration (inhalation) and expiration (exhalation). Primary functions of the respiratory system are to provide oxygen to tissues and to expel carbon dioxide from the body. Respiration is classified into 3 functional categories: external respiration, exchange of gas between the atmosphere and blood; internal respiration, exchange of gas between the blood and cells; and cellular respiration, the process whereby cells use oxygen and convert energy into useful forms. The major waste product of cellular respiration, carbon dioxide, diffuses from cells into blood, in which it is transported to the lungs and expelled during expiration. Secondary functions of the respiratory system are sound production, coughing, sneezing, and abdominal compression during urination, defecation, and parturition. Pharmacologic intervention becomes necessary when the respiratory system functions improperly.
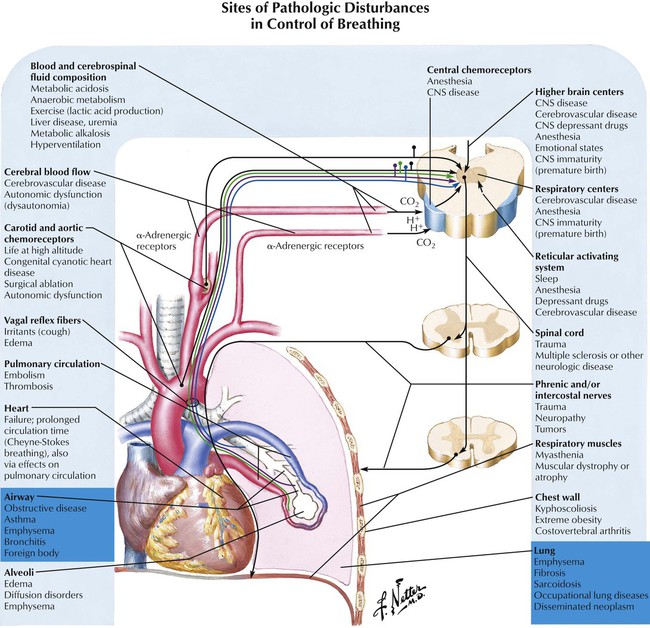
The most common respiratory disorders are asthma, cough, COPD (emphysema; chronic bronchitis), and pneumonia. Less common disorders are hyperventilation (excessive inspiration and expiration); apnea (temporary breathing cessation that may follow hyperventilation); and rhinitis (nasal mucosa inflammation). Drugs used for these conditions are normally given by inhalation (metered-dose or nebulized inhaler) or by oral means. Inhalation is preferred because of direct drug delivery to lungs, avoidance of first-pass metabolism by the liver and intestine, and minimization of adverse effects. Certain drugs used to treat asthma (eg, theophylline, albuterol, terbutaline) can be given orally. Parenteral dosing (intravascular, subcutaneous, or intramuscular) may be needed, especially when rapid onset of action is critical or drug absorption from the GI tract is poor; it controls the dose delivered, but adverse effects can result.
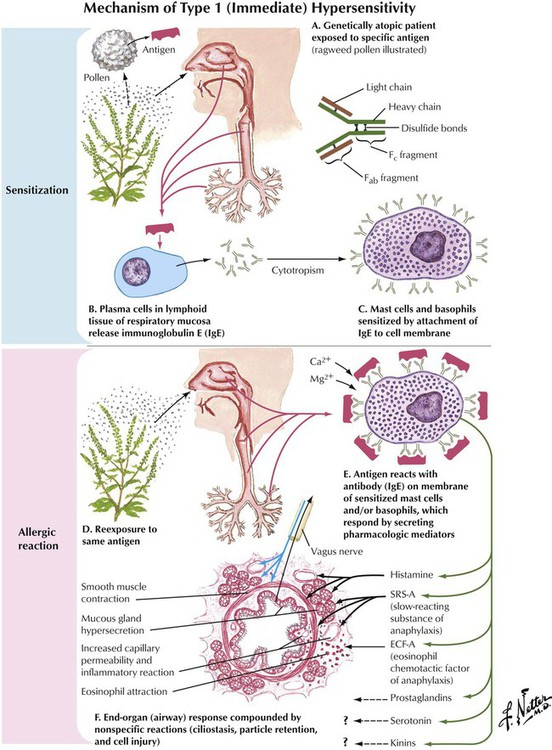
The term allergy, from the Greek allos (altered state) and ergon (reactivity), was first used to describe patients who had reactions caused by the effect of external factors, or allergens, on the body’s immune system. It is often defined as hypersensitive reactions of the immune system to substances (allergens) that are usually innocuous in most people, such as food, animal dander, pollen, bee stings, mold, ragweed, and drugs. The allergic person’s immune system recognizes something as foreign and mounts a specific reaction to identify the allergen and destroy it via inflammation. Thus, a sensitivity to a material that causes a symptom is allergic only if it has an identifiable mechanism. This distinction between allergic and nonallergic disorders is important because it determines evaluation and treatment. Treatment of an allergy as if it were nonallergic will fail and vice versa. In asthma, allergens increase sensitivity of bronchial smooth muscle, thereby creating an allergic state.
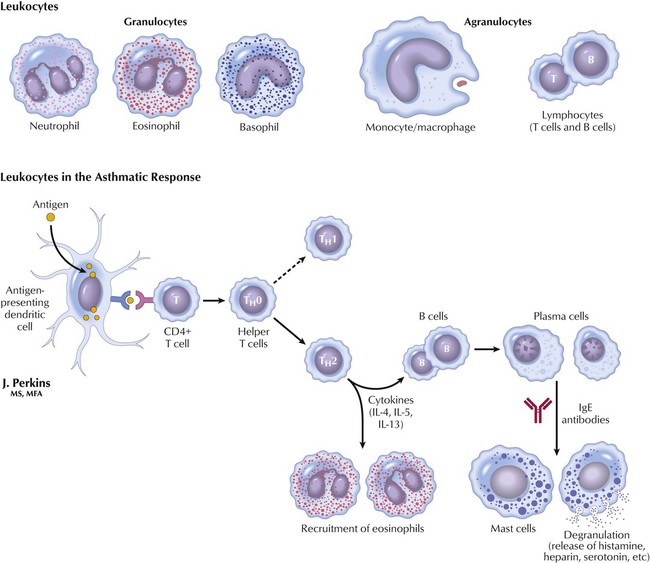
Humans have a special immune system to combat infectious and toxic agents (eg, bacteria and viruses). Major cells involved in defense against foreign substances are leukocytes, or white blood cells. Like all blood cells, they are synthesized in bone marrow. Leukocytes can be classified into 2 basic classes: granular, which store mediators in granules, and mononuclear or agranular, which have no granules. Three types of granular leukocytes exist: neutrophils, eosinophils, and basophils. Eosinophils, which phagocytize antigen-antibody complexes (antigen-IgE complexes that initiate an asthmatic reaction), and basophils, which release heparin (clotting), serotonin (clotting), and histamine (immune reaction), play primary roles in asthma. Agranular cells are monocytes, which phagocytize foreign particles, and lymphocytes, which play a critical role in the delayed asthmatic response. T cells (a subtype of lymphocytes) synthesize cytokines; B cells (another subtype) synthesize IgE antibodies.
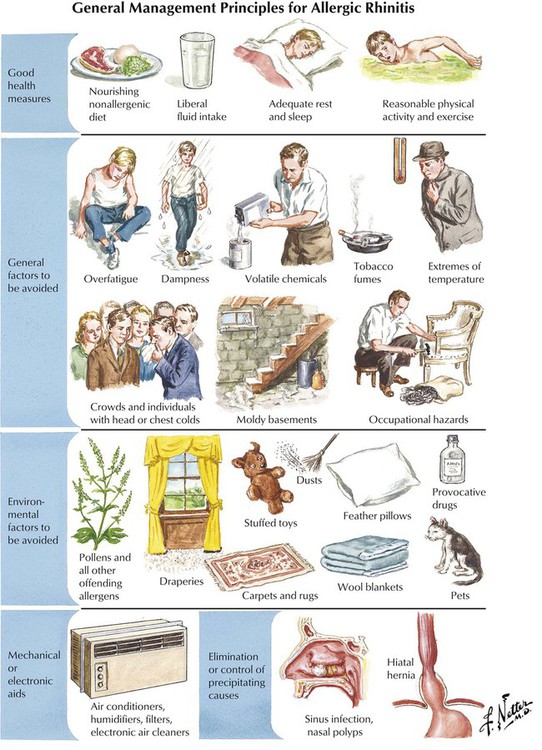
Allergic rhinitis (hay fever), an inflammation or irritation of the mucous membranes lining the nose, is initiated when allergens cause the body to defend itself by producing antibodies. The allergen-antibody combination prompts histamine release and the allergic response. Symptoms are sneezing, stuffy or runny nose, itchy eyes, noisy breathing, chronic fatigue, poor appetite, and nausea. The seasonal disorder is caused by pollen and normally wanes during winter; the perennial disorder occurs year-round and is caused by indoor allergens (eg, animal dander, mold spores, dust mites). Treatments are antihistamines (treatment of choice; blocks histamine action but can cause drowsiness), decongestants (relieve nasal stuffiness but can increase histamine release and worsen congestion), corticosteroids (desensitize cellular response to histamine and minimize the allergic reaction), and cromolyn sodium (inhibits histamine release, which reduces or stops the allergic response).
Bronchial asthma, known simply as asthma, is a chronic lung disease characterized by inflammation and obstruction of lower airways. Asthma affects approximately 5% of the US population, or 10 million people. The most common symptoms are acute constriction of bronchial smooth muscle, cough, chest tightness, wheezing, and rapid breathing. Asthma typically occurs in 2 stages: an initial phase followed by a second, delayed phase that occurs 6 to 12 hours later. Unlike diseases such as cystic fibrosis or chronic bronchitis, asthma is not a progressive disorder leading to COPD. Rather, it is a recurrent illness with periods of remission and exacerbation. However, a small percentage of patients with asthma present symptoms continuously. Precipitating factors include infections, allergens, irritant inhalants, stress, and other triggers. Deaths caused by asthma are infrequent.
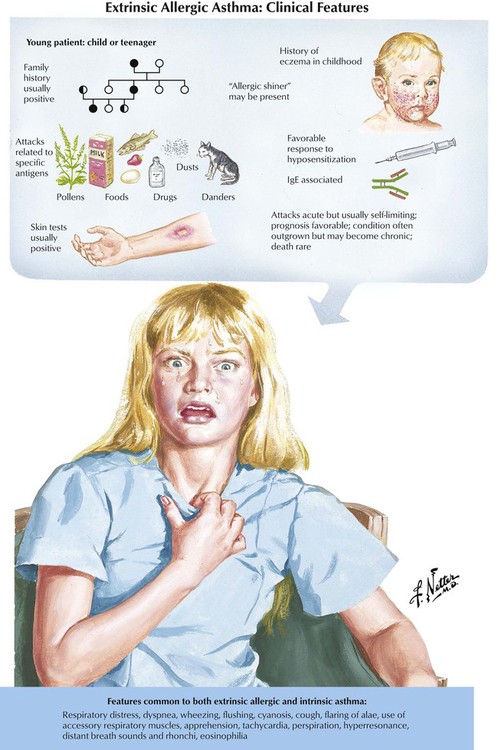
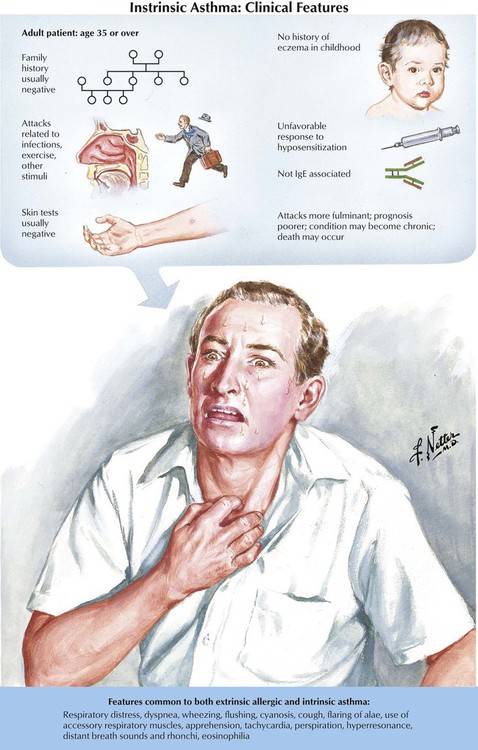
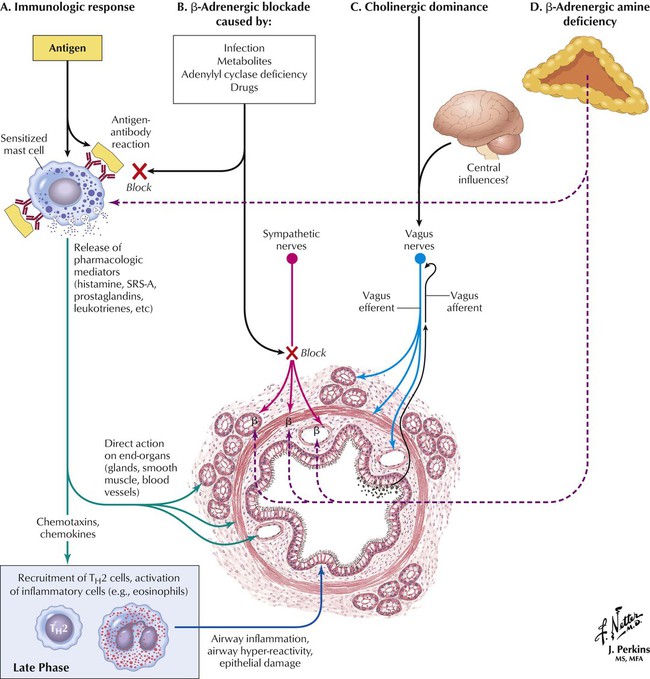
Pharmacotherapy of asthma depends on understanding the disease pathogenesis. In the immunologic, or antigen challenge, model, IgE antibodies produced by airway mucosa mast cells mediate asthma. B lymphocytes synthesize IgE antibodies after exposure to an antigen. IgE antibodies attach to mast cells and, with reexposure to antigen, form antigen-antibody complexes. The complexes trigger synthesis and release of mediators, such as histamine, leukotrienes (LTC4 and LTD4), and prostaglandins, from mast cells. Bronchoconstriction and vascular leakage result. Other substances (eg, cytokines) mediate the late response (IgE release). Corticosteroids reduce bronchial responses by inhibiting cytokine production. In some asthmatic patients who are not hypersensitive to antigens, infections and nonantigenic stimuli can evoke symptoms. Intrinsic asthma develops later in life, has unclear causes, is associated with a worse prognosis, and is less responsive to treatment than extrinsic asthma.
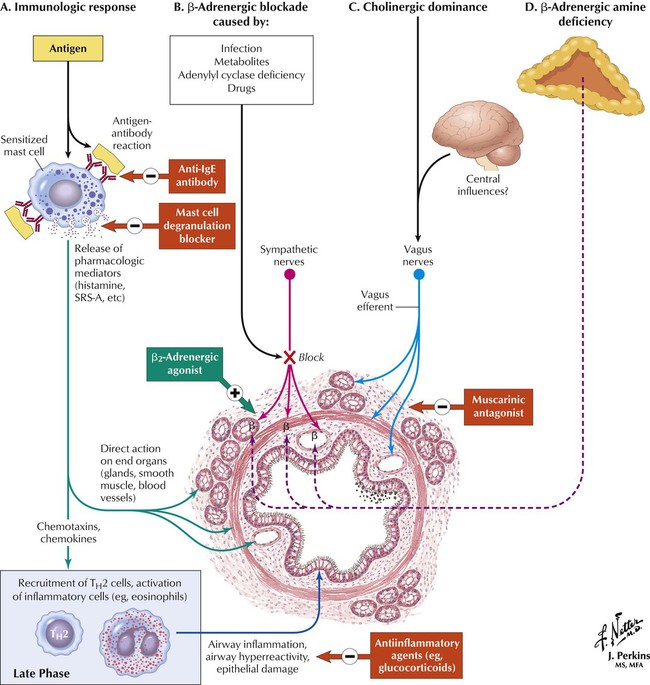
When exposure to allergens cannot be avoided, drug therapy is needed, the major goals being to reverse asthmatic symptoms and prevent recurrent episodes by disrupting actions of endogenous agents that worsen bronchospasm and inflammation. Major classes of drugs for asthma are anti-IgE antibodies, blockers of mast cell degranulation, smooth muscle relaxants, and antiinflammatory agents. Bronchodilators were the first and most effective treatment, but a better approach is prophylactic use of antiinflammatory agents to control bronchial inflammation. With these agents, patients with asthma are rarely hospitalized, seriously ill, or in need of emergency treatment. Patients can control their disease, and this therapy is much less expensive than previous emergency management. Now, antiinflammatory agents are the first-line therapy for patients who have more than occasional symptoms. Bronchodilators are still used but only when antiinflammatory therapy is inadequate, and then in smaller amounts.
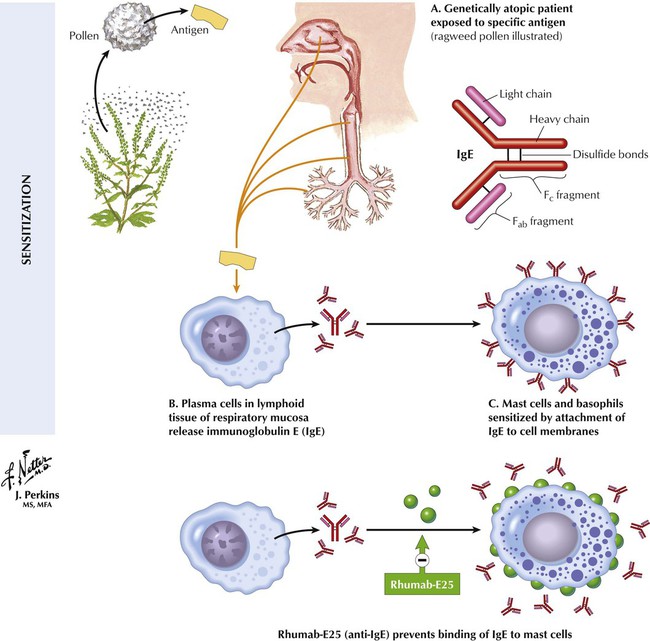
One of the more novel therapies is use of anti-IgE antibodies. In theory, drugs acting as anti-IgE antibodies would prevent IgE binding to mast cell surfaces. This action would reduce formation of activated antigen-IgE complexes and suppress release of mediators that induce immediate bronchoconstriction in the early phase. That is, mediators such as histamine, prostaglandins, and leukotrienes would be unable to cause sneezing, wheezing, itching, and coughing. The most notable anti-IgE antibody, Rhumab-E25, is a recombinant humanized monoclonal antibody to IgE. By binding to circulating IgE in the blood, Rhumab-E25 blocks release of inflammatory mediators by keeping IgE from binding to mast cells. This antibody, administered by parenteral injection, is currently in phase III clinical trials for seasonal allergic rhinitis and allergic asthma.
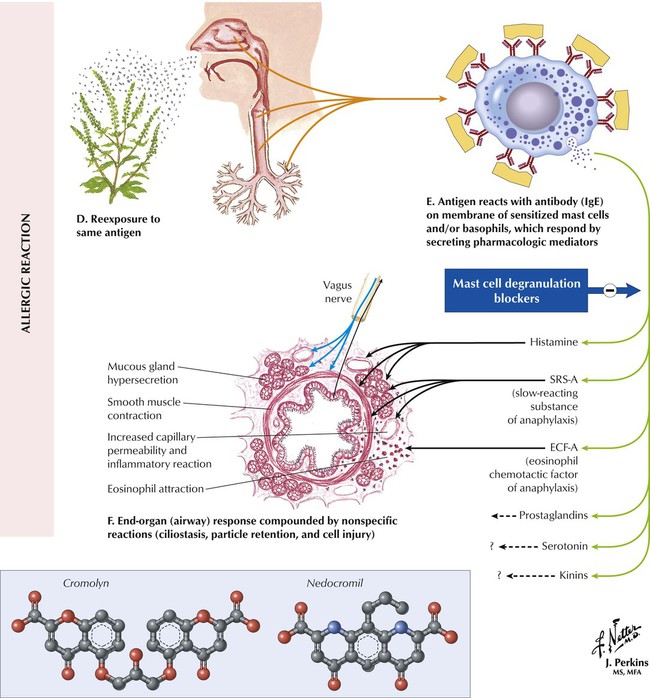
Cromolyn and nedocromil block mast cell degranulation by suppressing release of mediators of immediate bronchoconstriction (early response) and reducing eosinophil recruitment causing airway inflammation. Neither drug directly alters smooth muscle tone or reverses bronchospasm. Both drugs, usually inhaled as aerosols, can be used for intrinsic (antigen-induced) or extrinsic (non–antigen-induced) asthma. Nedocromil enhances corticosteroid effects and is more potent than cromolyn in patients with extrinsic asthma (especially exercise induced); even when given after reexposure to antigen, it blocks delayed inflammation. Both drugs are poorly absorbed, so adverse effects (eg, chest tightness, cough) are restricted to deposition site. Cromolyn is preferred for young patients. Both drugs alter Cl− channel function, which (1) on airway neurons underlies cough inhibition, (2) on mast cells delays antigen-evoked bronchoconstriction, and (3) on eosinophils prevents inflammatory responses to antigens.![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


