Drugs Used in Disorders of the Reproductive System
Overview
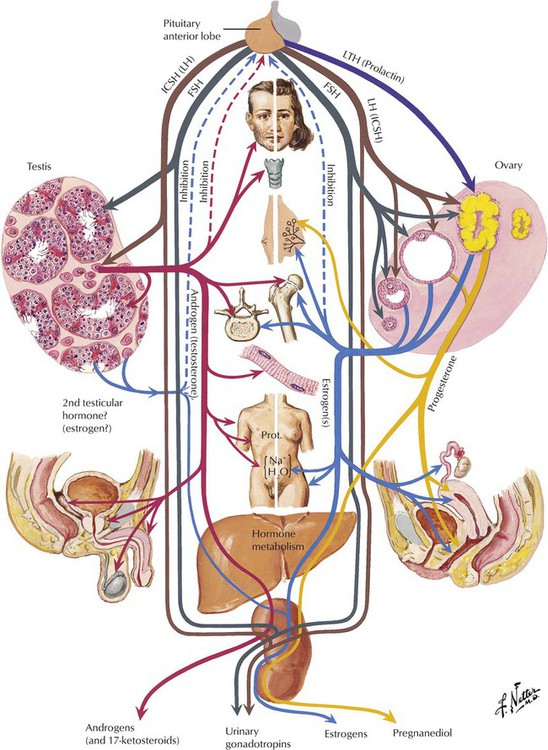
Sex hormones include progestins, estrogens, and androgens. They are produced by the gonads and adrenal glands and are necessary for conception, embryonic maturation, and development of primary and secondary sexual characteristics. As one example of these functional gonadal relations, the menstrual cycle is controlled by a neuroendocrine cascade involving the hypothalamus, pituitary, and ovaries. For control of this cycle, the hypothalamus releases gonadotropin-releasing hormone (GnRH), which triggers the anterior pituitary to release the gonadotropins luteinizing hormone (LH) and follicle-stimulating hormone (FSH), with effects on the ovaries. Androgens are steroids with anabolic and masculinizing effects in both males and females. Testosterone, the main androgen in humans, is synthesized and secreted primarily by testicular Leydig cells, as well as by ovaries in women and by adrenal glands. Testosterone secretion is also controlled by the hypothalamus-pituitary cascade.
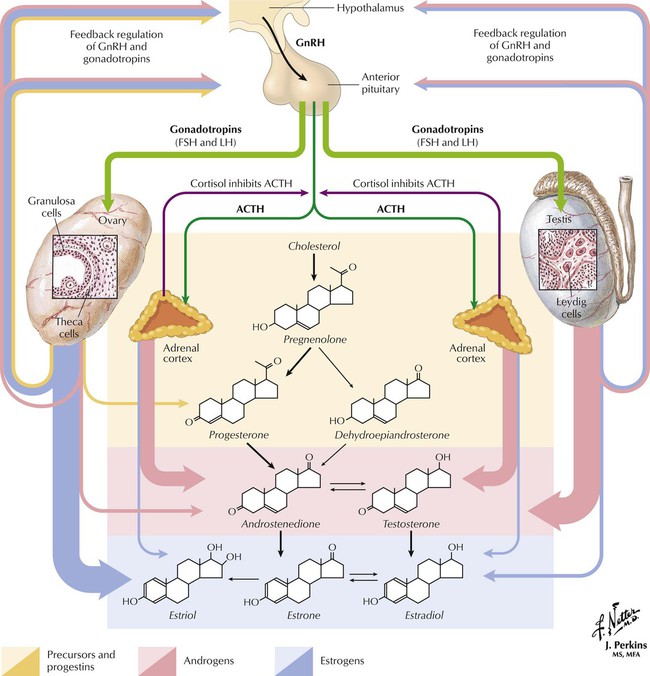
Estrogen is synthesized in several forms, estradiol being the most potent and estrone and estriol having one tenth its potency. Many organs and processes in women are under the influence of estrogen, but the menstrual cycle shows its greatest effects. For control of this cycle, the hypothalamus periodically releases GnRH, which triggers the anterior pituitary to release the gonadotropins LH and FSH. LH and FSH, which are responsible for growth and maturation of ovarian follicles, also control ovarian production of estrogen and progesterone, which exert feedback regulation on the pituitary and hypothalamus and signal them when to start and stop releasing GnRH, FSH, and LH. In males, the hypothalamus and anterior pituitary also effect release of FSH (starts spermatogenesis) and LH (triggers steroidogenesis in Leydig cells). The testosterone resulting from steroidogenesis inhibits hormone production via negative feedback on the pituitary and hypothalamus, and release of GnRH, FSH, and LH ends.
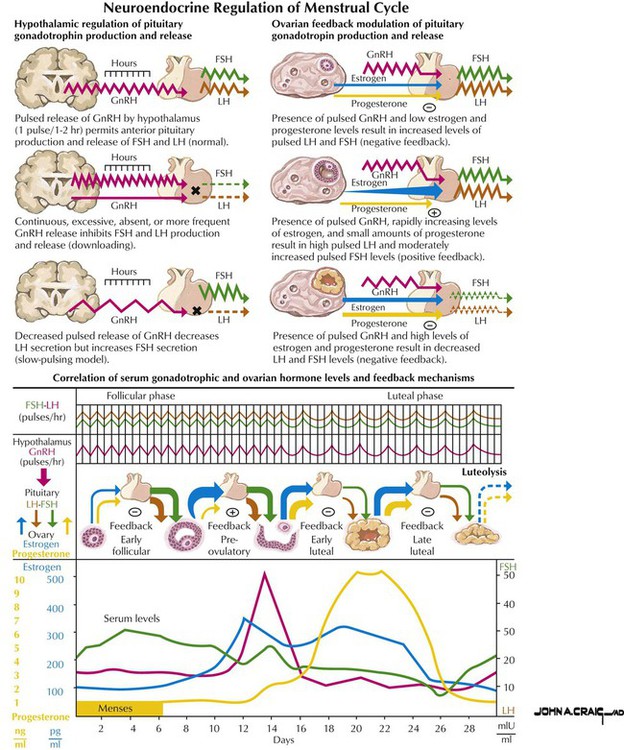
In the early (follicular) phase, the hypothalamus releases GnRH, which triggers the anterior pituitary to release LH and FSH. These gonadotropins cause the graafian follicle to mature and secrete estrogen. Estrogen inhibits the pituitary; it reduces the gland’s release of LH and FSH (negative feedback loop). In midcycle, however, estrogen triggers a surge in gonadotropin release from the pituitary (a brief positive feedback effect), which stimulates follicular rupture and ovulation. The ruptured follicle becomes the corpus luteum, which produces progesterone and estrogen under the influence of LH during the second half of the cycle (luteal phase). Progesterone promotes development of a secretory endometrium that can accommodate embryo implantation. Conception causes progesterone secretion to continue, with the endometrium maintained as suitable for pregnancy. Without conception, the corpus luteum stops progesterone release and ceases to function, hormone levels decrease, and menstruation begins.
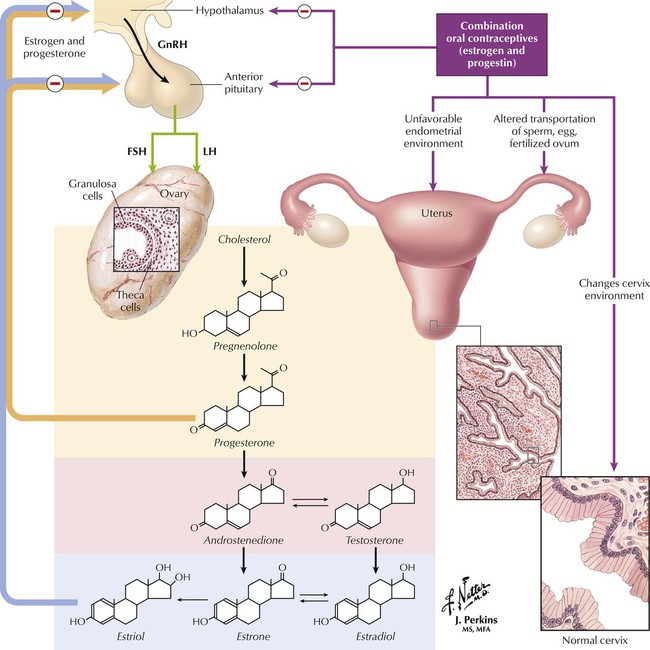
Combination oral contraceptives contain both estrogen and progestin and prevent pregnancy through several mechanisms. They inhibit ovulation via a negative feedback mechanism on the hypothalamus, which alters the normal pattern of FSH and LH secretion by the anterior pituitary. Estrogen suppresses FSH release from the pituitary during the follicular phase of the menstrual cycle and inhibits the midcycle surge of gonadotropins. Progestin inhibits the estrogen-induced LH surge. COCs also produce alterations in the genital tract. Progestin is likely responsible for changing the cervical mucus and rendering it unfavorable for sperm penetration even if ovulation occurs. COCs induce an environment in the endometrium that is unfavorable for implantation. COCs may also alter the tubal transport of the sperm, egg, and fertilized ovum through the fallopian tubes.
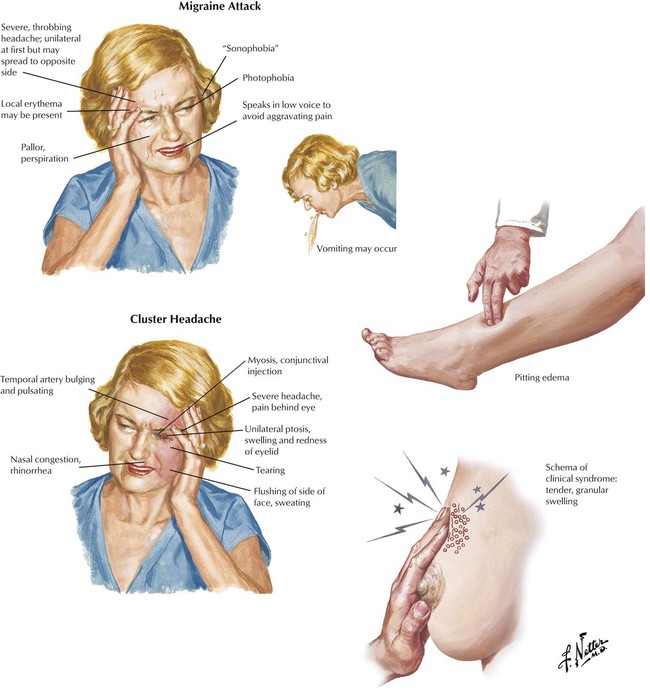
Major effects, related to excess or lack of estrogen or progestin, include breast fullness, depression, dizziness, edema, migraine, and vomiting. Serum lipoprotein profiles can change: estrogen increases HDL levels and decreases LDL levels; progestins (especially norgestrel) cause the unwanted opposite effect. COCs are associated with gallbladder disease, cholestasis, and abnormal glucose tolerance and are not used if cerebrovascular and thromboembolic disease, estrogen-dependent neoplasms, abnormal genital bleeding, chronic diabetes, or liver disease exists. Benefits include reduced risk of ovarian cysts, benign breast disease, and ectopic pregnancy and improved premenstrual symptoms, dysmenorrhea, endometriosis, acne, and hirsutism. COCs reduce endometrial and ovarian tumor incidence; their cause of other neoplasms is controversial. Other drugs—antibiotics (eg, tetracycline), rifampin, rifabutin, anticonvulsants—may decrease the efficacy of COCs.
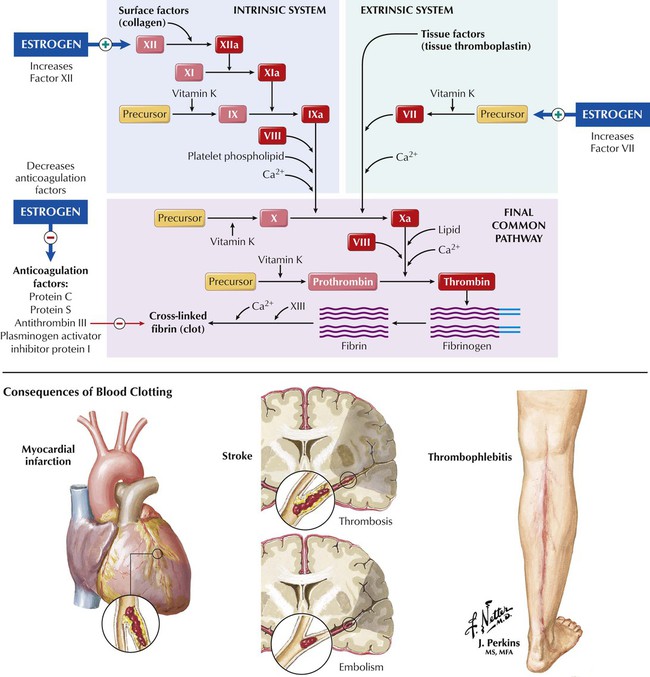
Estrogens may affect fibrinolytic pathways and cause a small increase in coagulation factors VII and XII and a decrease in anticoagulation factors protein C, protein S, plasminogen-activator inhibitor protein I, and antithrombin III. By causing this imbalance between coagulation and anticoagulation, estrogens may produce serious associated complications, including thromboembolism, thrombophlebitis, myocardial infarction, and cerebral and coronary thrombosis. These complications are more likely to occur in women who smoke and are older than 35 years.
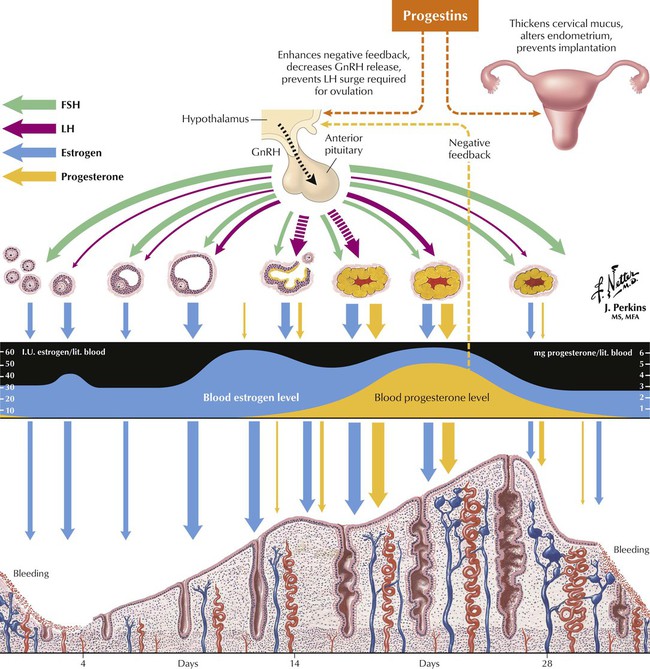
Progestin thickens cervical mucus, which decreases sperm penetration and alters the endometrium, thus preventing implantation. Progestin-only formulations are available as pills (“minipills”), depot injections, and implants. Pills contain norethindrone or norgestrel, taken daily on a continuous schedule; they are less effective than COCs because they block ovulation in only 60% to 80% of cycles. Depot injections of medroxyprogesterone acetate (MPA) impair implantation and produce plasma drug levels that are high enough to prevent ovulation in virtually all patients by slowing GnRH release, which thus prevents the LH surge required for ovulation. Progestin implants (subdermal capsules containing levonorgestrel) offer contraception for approximately 5 years. They are nearly as effective as sterilization, with completely reversible effects if the implants are surgically removed. Drug-related effects are weight gain, breast tenderness, headaches, and frequent occurrence of irregular menstrual bleeding.![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


