Drugs Used in Disorders of the Gastrointestinal System
Overview
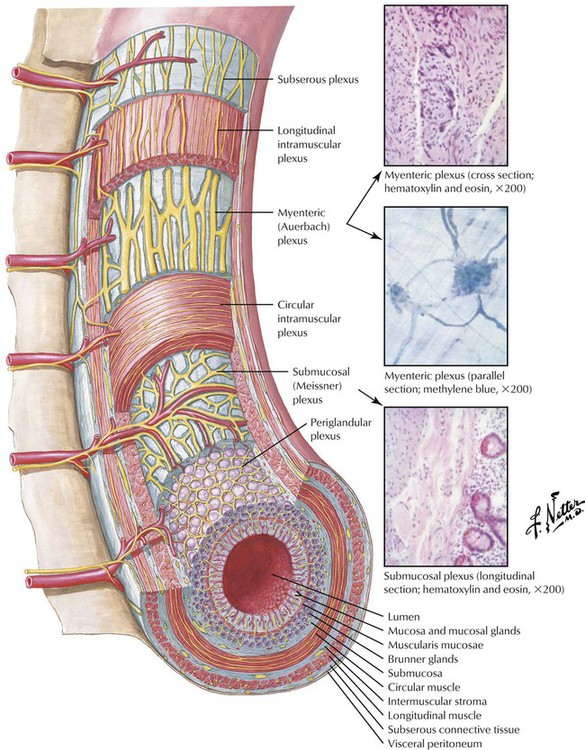
The nervous system exerts a profound influence on all digestive processes (motility, ion transport associated with secretion and absorption, and blood flow). Some of this control emanates from connections between the digestive system and the CNS, but just as important, the digestive system is endowed with its own, local nervous system, referred to as the enteric or intrinsic nervous system. Principal components of the enteric nervous system are 2 networks or plexuses of neurons, both of which are embedded in the wall of the digestive tract and extend from the esophagus to the anus. The myenteric (Auerbach) plexus is located between the longitudinal and circular layers of muscle in the tunica muscularis and controls primarily digestive tract motility. The submucosal (Meissner) plexus regulates GI blood flow and epithelial cell function by monitoring luminal contents.
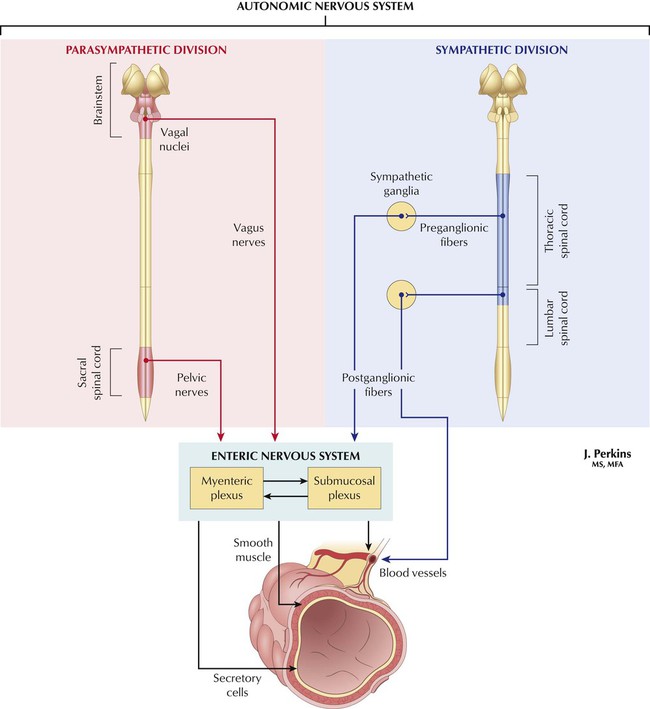
The enteric plexuses contain 3 types of neurons, most of which are multipolar. Motor neurons control GI motility, secretion, and absorption. They act directly on smooth muscle, secretory cells (parietal, chief, mucous, pancreatic exocrine cells), and GI endocrine cells. Sensory neurons receive information from sensory receptors in the mucosa and muscle. They respond to mechanical, thermal, osmotic, and chemical stimuli. Chemoreceptors are sensitive to pH, glucose, and amino acids. Sensory receptors in muscle respond to stretch and tension. Interneurons integrate information from sensory neurons and transmit it to enteric motor neurons. Enteric neurons secrete ACh and norepinephrine. Neurons that secrete ACh are excitatory and stimulate smooth muscle contraction, increase intestinal secretions, release enteric hormones, and relax (dilate) blood vessels. Norepinephrine, released from extrinsic sympathetic neurons, is inhibitory and opposes biologic actions of ACh.
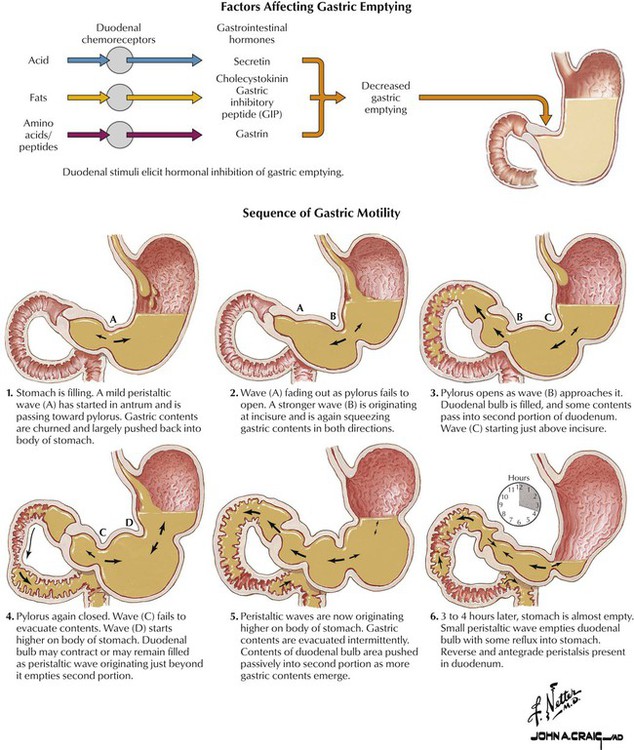
The digestive tube shows 2 basic motility patterns: propulsion, the movement of food along the tube so that food can be catabolized and absorbed, and peristalsis, the major type of propulsive motility, seen especially in the esophagus and small intestine. A ring of muscle contraction appears on the oral side of a food bolus and moves toward the anus, so the luminal contents are forced in that direction. As the ring moves, the muscle on the other side of the distended area relaxes for smooth passage of the bolus. Mixing ensures that ingested materials are exposed to digestive enzymes and properly absorbed. In the absence of mixing, food is not in contact with epithelial cells that absorb nutrients. Segmentation contractions are a common type of mixing motility seen especially in the small intestine; segmental rings of contraction break down and mix food. Alternating contraction and relaxation of longitudinal muscle in the gut wall also provides effective mixing of its contents.
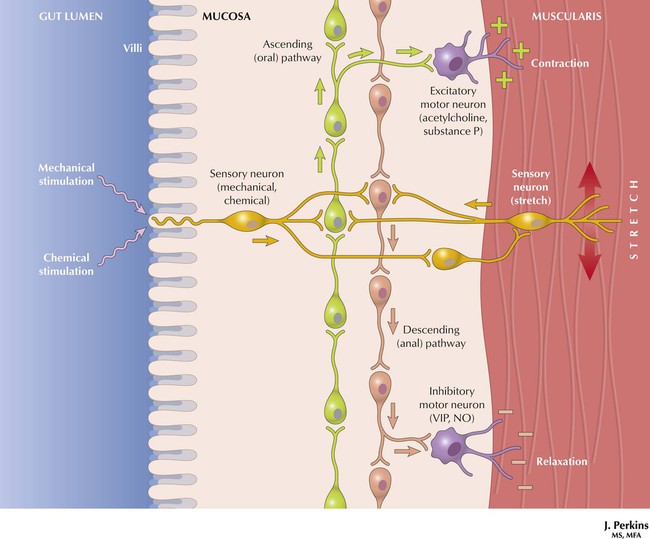
Food in the intestinal lumen causes smooth muscle contraction above the bolus and relaxation below, so that a peristaltic wave moves food down the intestine from the mouth to the anus. The enteric nervous system controls peristalsis and can work separately from the CNS, but digestion needs enteric nervous system and CNS coordination. Parasympathetic and sympathetic neurons connect the CNS and digestive tract, which allows sensory information to be sent to the CNS, as well as CNS regulation of GI function and relay of non-GI system signals. Sympathetic stimulation inhibits GI secretion and motor activity and causes GI sphincter and blood vessel contraction. Parasympathetic stimulation increases GI secretion and motor activity and causes GI sphincter and blood vessel dilation. Important peristaltic reflexes are the gastrocolic, in which stomach distension causes colonic exodus, and the enterogastric, in which small intestine distension or irritation reduces stomach secretion and motor activity.
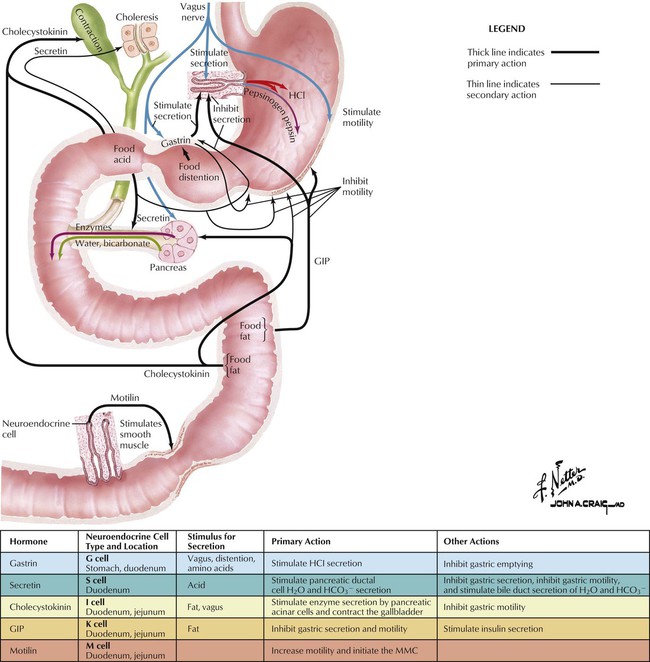
The endocrine system regulates GI function by secreting hormones. Hormones are chemical messengers secreted into blood that modify the physiology of target cells. Digestive function is affected by hormones produced in many endocrine glands, but the greatest control is exerted by hormones produced within the GI tract. The GI tract is the largest endocrine organ in the body, and the endocrine cells within it are referred to collectively as the enteric endocrine system. Three of the best-studied enteric hormones are gastrin, cholecystokinin (CCK), and secretin. Gastrin is secreted from the stomach and plays an important role in control of gastric acid secretion. CCK is a small intestinal hormone that stimulates secretion of pancreatic enzymes and bile. Secretin is a hormone secreted from small intestinal epithelial cells that stimulates secretion of bicarbonate-rich fluids from the pancreas and liver.
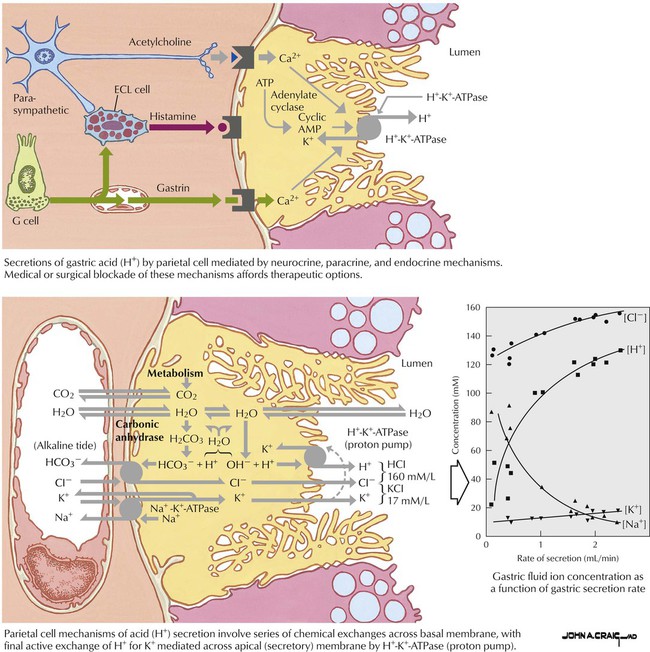
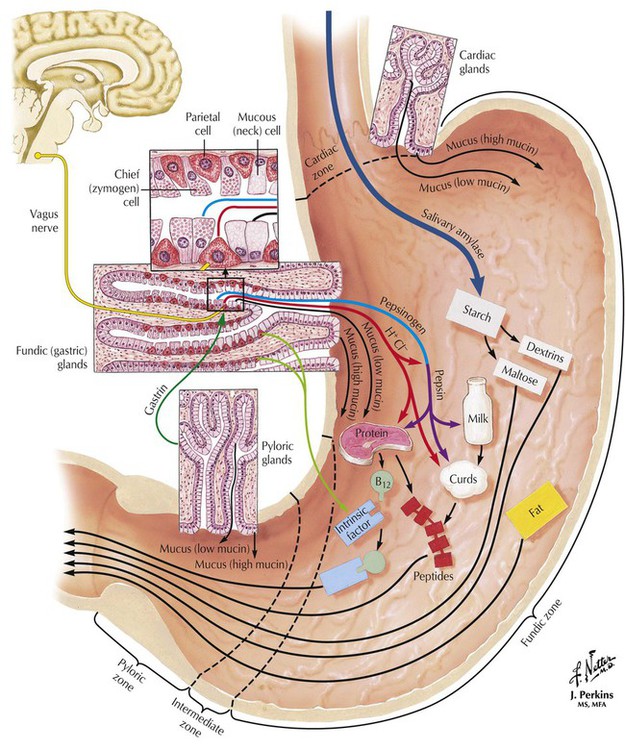
The stomach’s parietal cells secrete approximately 2 L of acid a day as hydrochloric acid. This acid eradicates bacteria, aids in digestion by solubilizing food, and maintains optimal pH (1.8-3.2) for the function of pepsin, a digestive enzyme. H+,K+-ATPase (the proton pump) is expressed on parietal cell apical membranes and uses energy from ATP hydrolysis to pump hydrogen ions into the lumen in exchange for potassium ions. Three regulatory molecules stimulate acid secretion—ACh, histamine, gastrin—and one inhibits acid secretion—somatostatin. ACh increases acid secretion by stimulating muscarinic (M1) receptors. Histamine, a paracrine hormone released from enterochromaffinlike cells, stimulates acid secretion by activating H2 receptors. Gastrin, a hormone released by G cells (endocrine cells in gastric epithelium), increases acid release by activating gastric receptors. Somatostatin is also secreted by gastric endocrine cells and, with prostaglandins, opposes the stimulatory actions of gastrin.
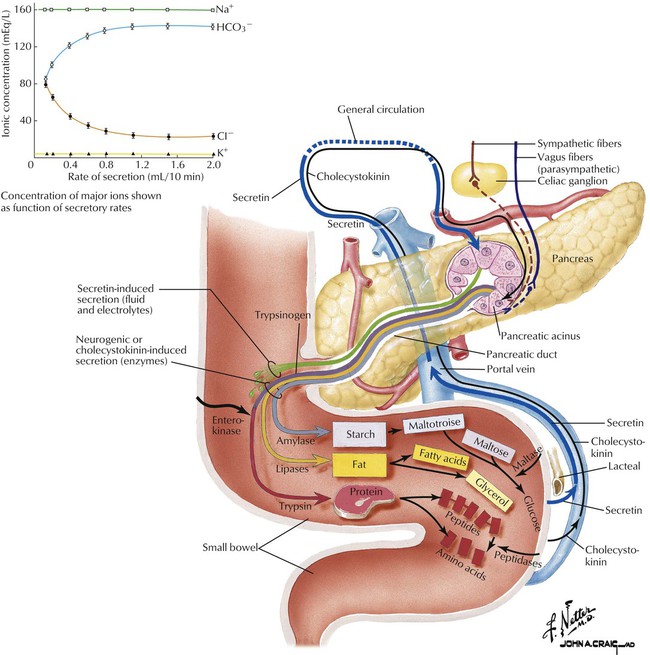
Exocrine pancreas secretion is under neural and endocrine control. Pancreatic secretions, the major mechanism for neutralizing gastric acid in the small intestine, are stimulated by food entering the stomach and chyme entering the small intestine. The vagus nerve innervates the pancreas (and the stomach) and applies a low-level stimulus for secretion in anticipation of a meal. The most important stimuli for pancreatic secretion come from 3 enteric nervous system hormones. CCK is synthesized and secreted by duodenal endocrine cells in response to partly digested proteins and fats in the small intestine. CCK is released into blood and binds to receptors on pancreatic acinar cells, which induces digestive enzyme secretion. Secretin, secreted in response to acid in the duodenum, stimulates pancreatic secretion of water and bicarbonate. Gastrin, like CCK, is secreted by the stomach and stimulates acid secretion by parietal cells and digestive enzyme secretion by pancreatic acinar cells.
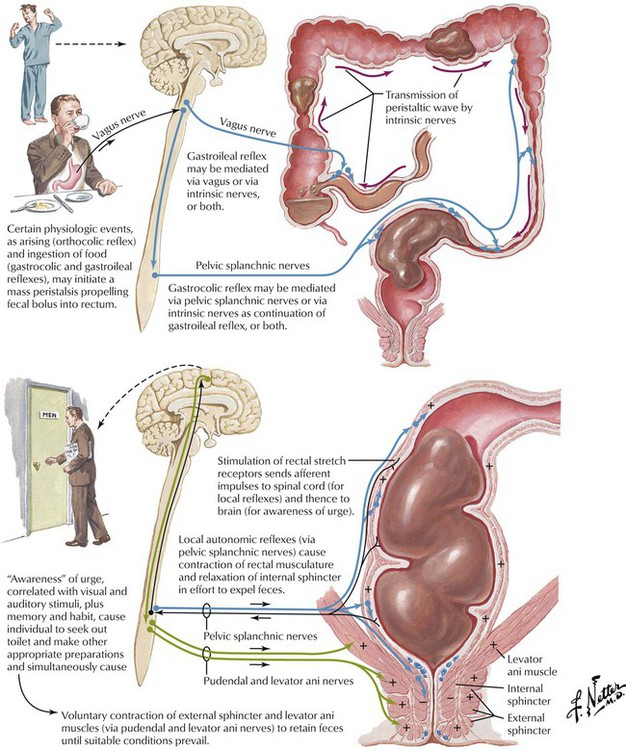
Defecation (passing of feces through the rectum and anus) occurs via relaxation of the involuntary and voluntary internal anal sphincter and heeding the rectosphincteric reflex; it is prevented by external anal sphincter contraction. The rectum filling with fecal material causes the urge to defecate. When the external anal sphincter relaxes, rectal smooth muscle contracts to force feces out. The presence of food in the stomach increases colon motility. A rapid parasympathetic response (stimulated GI motility by depolarizing smooth muscle cells) is initiated; CCK and gastrin mediate a slower hormonal response. Disorders of large intestine motility may be caused by emotional factors via the extrinsic autonomic nervous system; IBS, a disorder worsened by stress, causes constipation or diarrhea. Megacolon (Hirschsprung disease), the absence of the colon enteric nervous system, causes intestinal contents near the constriction to accumulate and severe constipation.
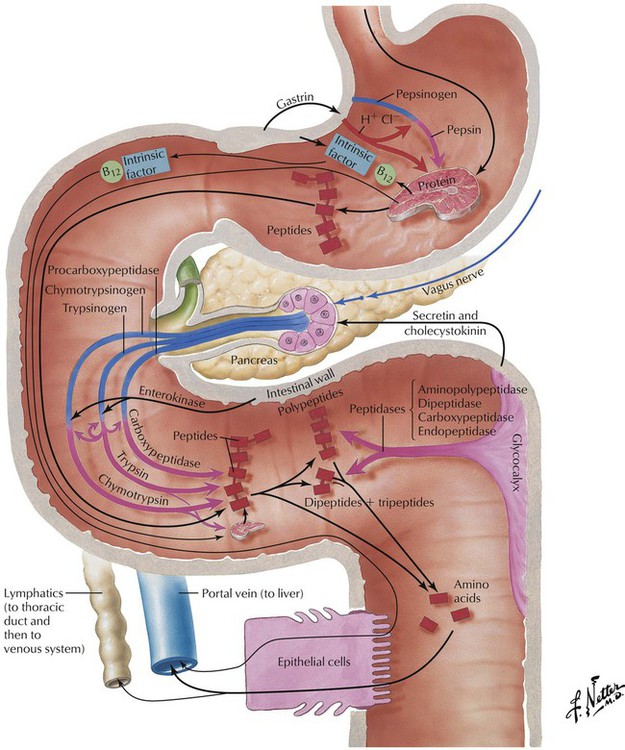
Proteolytic enzymes are packaged in vesicles in an inactive form and are thus protected against the harsh pH conditions of the GI tract. Pepsin is a stomach enzyme derived from pepsinogen that is active at low pH. Pepsin cleaves the peptide bond between acidic (aspartic or glutamic acid) and aromatic (phenylalanine, tyrosine) amino acids. This endonuclease catabolizes proteins into smaller peptides. Trypsin is a pancreatic enzyme derived from trypsinogen that is active at slightly basic pH. Trypsin hydrolyzes peptide bonds adjacent to the basic amino acids lysine and arginine, thus hydrolyzing proteins into smaller peptides. Other endopeptidases, such as chymotrypsin and enterokinase, digest proteins into multiple amino acid fragments. Pancreatic carboxypeptidase is an exopeptidase that hydrolyzes dipeptides at the carboxyl end. Small intestine aminopeptidase is an exopeptidase that hydrolyzes dipeptides from the amino end. Finally, dipeptidase liberates free amino acids.![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


