47 Drugs in pregnancy and lactation
Drugs in pregnancy
Drugs in pregnancy
There is now a greater appreciation of the risks of drug use in pregnancy, and it is generally accepted that maternal pharmacotherapy should be avoided or minimised where possible. Nevertheless, it has been estimated that over 80% of expectant mothers take three or four drugs at some stage of pregnancy (Headley et al., 2004) with a significant number of women taking medication at the time their pregnancy is detected. Indications for drug use range from chronic illnesses such as epilepsy and depression to those commonly associated with pregnancy such as hypertension, urinary tract infections and gastro-intestinal complaints.
Drugs as teratogens
A teratogen is defined as any agent that results in structural or functional abnormalities in the fetus, or in the child after birth, as a consequence of maternal exposure during pregnancy. Examples of drugs that are known to be human teratogens are shown in Box 47.1. The teratogenic mechanism for most drugs remains unclear, but may be due to the direct effects of the drug on the fetus and/or as a consequence of indirect physiological changes in the mother or fetus. Perhaps the best known, and most widely studied teratogen is thalodimide, a mild sedative that was widely marketed as a remedy for pregnancy-related nausea and vomiting. In 1961, thalidomide was withdrawn from the UK market following numerous reports of severe anatomical birth defects in infants of mothers who took the drug in early pregnancy. Whereas external congenital anomalies such as limb abnormalities, spina bifida and hydrocephalus may be obvious at birth, some defects may take many years to manifest clinically or be identified. Examples of delayed effects of teratogens are the behavioural and intellectual disorders associated with in utero alcohol exposure and the development of clear-cell vaginal cancer in young women following maternal intake of diethylstilboestrol, used first in the 1930s for the prevention of miscarriage and preterm delivery (Herbst et al., 1971).
Critical periods in human fetal development
Pre-embryonic stage (weeks 0–2 post-conception)
The first two weeks post-conception are regarded as the pre-embryonic stage and describe the period up to implantation of the fertilised ovum. Teratogenic exposure during the pre-embryonic stage is thought to elicit an ‘all-or-nothing’ response, leading either to death of the embryo or complete recovery and normal development of the fetus. Fetal malformations following drug exposure during this period are therefore thought to be unlikely, except where the half-life of the drug is sufficient to extend exposure into the embryonic stage. A good example of the latter is isotretinoin and related vitamin A derivatives which have half-lives up to a week, and which when used systemically, for example, for the treatment of acne and psoriasis, are recognised teratogens (Nulman et al., 1998).
Fetal stage (weeks 9–38 post-conception)
During the fetal stage, the fetus continues to develop, grow and mature and, importantly, remains susceptible to some drug effects. This is especially true for the central nervous system, which can be damaged by exposure to certain drugs, for example, ethanol, at any stage of pregnancy. The external genitalia also continue to form from the seventh week until term, and consequently, danazol, which has weak androgenic properties, can cause virilisation of a female fetus if given in any trimester after the eighth week of pregnancy when the androgen receptors begin to form (Rosa, 1984).
Further examples include the angiotensin-converting enzyme (ACE) inhibitors, which if given in the second and third trimesters can result in fetal renal dysfunction and subsequent oligohydramnios, that is, reduced amniotic fluid volume (Sedman et al., 1995). The non-steroidal anti-inflammatory drugs (NSAIDs) are another important group of drugs that may cause problems specifically in the third trimester. These drugs inhibit prostaglandin synthesis in a dose-related fashion and, when given late in pregnancy, may result in premature closure of the fetal ductus arteriosus and fetal renal impairment (Koren et al., 2006). NSAIDs should therefore be avoided during the third trimester.
Principles of teratogenesis
Timing of exposure
The stage of pregnancy at which a drug exposure occurs is key to determining the likelihood, severity or nature of any adverse effect on the fetus. Risk both between and within trimesters may be variable. For example, folic acid antagonists, for example, trimethoprim, are associated with an increased risk of neural tube defects if exposure occurs before neural tube closure (third to fourth week post-conception), but not after this period (Hernandez-Diaz et al., 2001). It has also been suggested that trimethoprim should be avoided after 32 weeks’ gestation in view of the theoretical risk of severe jaundice in the neonate as a result of bilirubin displacement from protein binding, although clinical evidence to support this is lacking (Dunn, 1964). Unfortunately, the precise period of teratogenic risk is known for very few substances. One drug for which this period has been established is thalidomide, where exposure between days 20 and 36 post-conception is associated with a high risk of congenital malformation (Lenz, 1988; Newman, 1986).
Species
Teratogenicity of a drug may be species dependent. Interestingly, preclinical thalidomide studies in mice and rats did not result in congenital malformation in the offspring (Breitkreutz and Anderson, 2008; Miller et al., 2009; Vorhees et al., 2001). Birth defects or other adverse reproductive outcomes observed in animal studies cannot therefore be simply extrapolated to the human situation. Further, the drug dose and route of administration used in early animal studies may not be comparable to clinical use in humans.
Genotype and environmental interaction
Not all fetuses exposed to known teratogenic drugs show evidence of having been affected in utero. It remains undetermined as to whether this variable susceptibility to teratogenic drugs is a result of genetic differences in the exposed mothers, the fetal genotype, modifying environmental factors or a combination of all three. Malformations are reported to occur in only 20–50% of infants born to mothers exposed to thalidomide during the period of greatest risk for embryopathy, that is, days 20–36 post-fertilisation (Lenz, 1966; Newman, 1985). Similarly, maternal treatment with systemic isotretinoin during the first trimester results in fetal malformation in only 18–35% of the live born infants, with a further 30% of children exhibiting developmental delay in the absence of physical deformity (Benke, 1984; Braun et al., 1984; Hill, 1984).
Pharmacological effect
The neonate can also be adversely affected by maternal drug therapy (see Table 47.1). It is generally only at birth that signs of fetal distress are observed due to in utero drug exposure or the effects of abrupt discontinuation of the maternal drug supply. The capacity of the neonate to eliminate drugs is reduced, and this can result in significant accumulation of some drugs, leading to toxicity. Neonatal withdrawal effects may require treatment.
Table 47.1 Examples of drugs with pharmacological effects on the fetus or neonate
| Drug | Possible adverse pharmacological effect | Notes |
|---|---|---|
| ACE inhibitors | Fetal and neonatal hypoxia, hypotension, renal dysfunction, oligohydramnios and intra-uterine growth retardation | Monitor fetus if long-term therapy in the second or third trimester |
| β-Blockers, for example, atenolol | Neonatal bradycardia, hypotension and hyperglycaemia | Neonatal symptoms are usually mild and improve within 48 h. No long-term effects |
| Benzodiazepines | ‘Floppy infant syndrome’ | Risk if regular use in third trimester |
| Withdrawal reactions | Neonatal observation recommended | |
| Corticosteroid (high dose) | Fetal adrenal suppression | Dependent on dose and treatment interval |
| NSAID | Premature closure of the ductus arteriosus (affecting fetal circulation) and fetal renal impairment (decreased urine output) | Avoid repeated use after week 28. If unavoidable, fetal circulation monitored regularly |
| Opioids | Neonatal withdrawal symptoms | Risk if used long-term |
| Respiratory depression | Risk if used near term | |
| Phenothiazines | Neonatal withdrawal and transient extrapyramidal symptoms | Observation for at least 48 h. Symptoms may last for several weeks |
| Tricyclic and SSRI antidepressants | Neonatal withdrawal symptoms | Risk if used long-term and/or near term. Observation for at least 48 h |
(adapted from Schaefer et al., 2007)
Maternal pharmacokinetic changes
There are a number of maternal changes which occur during pregnancy and are summarised in Table 47.2.
Table 47.2 Summary of pharmacokinetic changes during pregnancy (adapted from Schaefer et al., 2007)
| Absorption | Change during pregnancy |
|---|---|
| Gastro-intestinal motility | ↓ |
| Lung function | ↑ |
| Skin blood circulation | ↑ |
| Distribution | |
| Plasma volume | ↑ |
| Body water | ↑ |
| Plasma protein | ↓ |
| Fat deposition | ↑ |
| Metabolism | |
| Liver activity | ↑ ↓ |
| Excretion | |
| Glomerular filtration | ↑ |
Absorption
Gastric and intestinal emptying time increases by 30–40% in the second and third trimesters (Pavek et al., 2009) and could be important in delaying absorption and time to onset of action for some drugs (Loebstein et al., 1997). There is also a reduction in gastric acid secretion in the first and second trimesters and an increase in mucus secretion. As a consequence of the increase in gastric pH, the ionisation, and hence absorption, of weak acids and bases can be affected.
Distribution
The volume of distribution of drugs may be altered because of an increase of up to 50% in blood (plasma) volume and a 30% increase in cardiac output. Renal blood flow increases by up to 50% at the end of the first trimester and uterine blood flow increases and peaks at term (36–42 L/h). There is also a mean increase of 8 L in body water (60% to placenta, fetus and amniotic fluid and 40% to maternal tissues). As a consequence, there may be increased dosage requirements for some drugs to achieve the same therapeutic effect, provided these effects are not offset by other pharmacokinetic changes. Both the total plasma and the free-drug concentrations of phenytoin, carbamazepine and valproic acid decrease during pregnancy, but the free-drug fraction (ratio of free to total plasma concentration) may increase (Pavek et al., 2009).
Metabolism
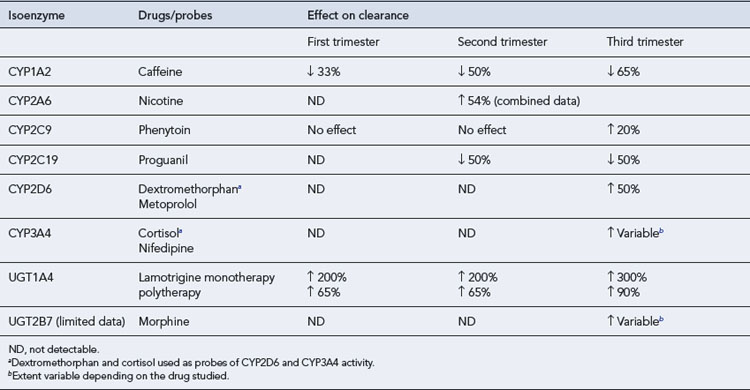
The metabolic activity of cytochrome P450 isoenzymes CYP3A4, CYP2D6, CYP 2A6 and CYP 2C9 and uridine 5′-diphosphate glucuronosyltransferase (UGT) isoenzymes (UGT1a1, UGT1A4 and UGT2B7) is increased during pregnancy. Drugs metabolised by these isoenzymes may therefore require dose adjustment. This may decrease the amount of the drug available for transfer across the placenta and thereby influence fetal exposure. In contrast, the metabolic activity of CYP1A2 and CYP2C19 is decreased during pregnancy and drugs metabolised by these isoenzymes may need dose reduction to minimise toxicity (see Table 47.3).
Excretion
Within the first few weeks of pregnancy, the glomerular filtration rate (GFR) increases by approximately 50%. Consequently, those drugs which are excreted primarily unchanged by the kidneys, for example, lithium, digoxin and penicillin, show enhanced elimination and lower steady-state concentrations. The following drugs have shown pregnancy-induced increases of 20–65% on their renal elimination (Anderson, 2005):
Drug selection in pregnancy
Although there are few, if any, drugs for which safe use in pregnancy can be absolutely assured, only a handful of drugs in current clinical use have been conclusively shown to be teratogenic. In general, drugs that have been used extensively in pregnant women without apparent problems are recommended in preference to new drugs for which there is less experience of use. For example, methyldopa is used rarely to treat hypertension in the non-pregnant state but has historically been preferred in pregnancy because of a long history of safe use (Schaefer et al., 2007). However, older drugs may be less effective in terms of controlling maternal illness and are often associated with an increased side-effect risk profile.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree