15
Drug Therapy of Hypertension, Edema, and Disorders of Sodium and Water Balance
This chapter will be most useful after having a basic understanding of the material in the section on hypertension in Chapter 27 Drug Therapy of Myocardial Ischemia and Hypertension in Goodman & Gilman’s The Pharmacological Basis of Therapeutics, 12th Edition (pp 765-785), as well as material in Chapter 25 Regulation of Renal Volume and Vascular Volume and Chapter 26 Renin and Angiotensin. In addition to the material presented here, the 12th Edition contains:
• The molecular structures of drugs used to treat hypertension, edema, and other disorders of Na+ and water balance
• Figure 25-1 The anatomy and nomenclature of the nephron
• Figure 25-5 Changes in the extracellular fluid volume and weight with diuretic therapy
• An extensive discussion of the functions and effects of the renin-angiotensin system in Chapter 26
LEARNING OBJECTIVES
 Understand the mechanisms of action of drugs used to treat hypertension, edema, and other disorders of Na+ and water balance.
Understand the mechanisms of action of drugs used to treat hypertension, edema, and other disorders of Na+ and water balance.
 Know the untoward effects of drugs used to treat hypertension, edema, and other disorders of Na+ and water balance.
Know the untoward effects of drugs used to treat hypertension, edema, and other disorders of Na+ and water balance.
 Know which patients should be treated and when treatment should be initiated.
Know which patients should be treated and when treatment should be initiated.
 Know which drugs are most effective in treating individual hypertensive patients with specific comorbidities, including diabetes mellitus, congestive heart failure, and renal disease.
Know which drugs are most effective in treating individual hypertensive patients with specific comorbidities, including diabetes mellitus, congestive heart failure, and renal disease.
 Know which drugs can be used in combination.
Know which drugs can be used in combination.
 Know how to set treatment goals based on target blood pressures and other clinical measures.
Know how to set treatment goals based on target blood pressures and other clinical measures.
DRUGS INCLUDED IN THIS CHAPTER
• Acetazolamide (DIAMOX, others)
• β Adrenergic receptor antagonists (many; Table 15-1; see Chapter 7)
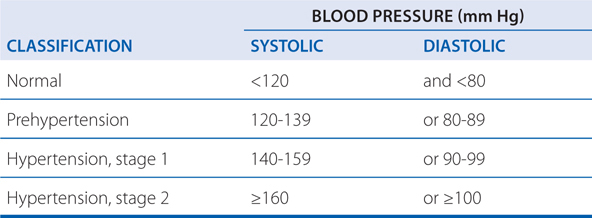
TABLE 15-1 Criteria for Hypertension in Adults
• Aliskiren (TEKTURNA)
• Amiloride (MIDAMOR, others)
• Amiloride/hydrochlorothiazide (generic)
• Amlodipine (NORVASC)
• Bendroflumethiazide (NATURETIN)
• Benzapril (LOTENSIN, others)
• Bumetanide (BUMEX, others)
• Candesartan cilexetil (ATACAND)
• Captopril (CAPOTEN, others)
• Chlorothiazide (DIURIL)
• Chlorthalidone (HYGROTON)
• Clevidipine (CLEVIPREX)
• Clonidine (CATAPRES, others)
• Conivaptan (VAPRISOL)
• Desmopressin acetate (1-deamino-8-D-arginine vasopressin, DDAVP, others)
• Diazoxide
• Dichlorphenamide (DARAMIDE)
• Diltiazem (CARDIZEM)
• Doxazosin (CARDURA, others)
• Enalapril (VASOTEC, others)
• Enalaprilat (VASOTEC INJECTION, others)
• Eplerenone (INSPRA, others)
• Ethacrynic acid (EDECRIN, others)
• Felodipine (PLENDIL)
• Fenoldopam (CORLOPAM)
• Fosinopril (MONOPRIL, others)
• Furosemide (LASIX, others)
• Glycerin (OSMOGLYN)
• Guanabenz (WYTENSIN)
• Guanadrel
• Guanfacine (INTUNIV, TENEX)
• Human recombinant ANP (carperitide, available only in Japan)
• Human recombinant BNP (nesiritide, NATRECOR)
• Hydralazine (APRESOLINE)
• Hydrochlorothiazide (HYDRODIURIL)
• Hydroflumethiazide (SALURON)
• Indapamide (LOZOL)
• Irbesartan (AVAPRO)
• Isosorbide (ISMOTIC)
• Isradipine (DYNACIRC)
• Lisinopril (PRINIVIL, ZESTRIL, others)
• Losartan (COZAAR)
• Mannitol (OSMITROL, others)
• Methazolamide (GLAUCTABS)
• Methyclothiazide (ENDURON)
• Methyldopa (ALDOMET, others)
• Metolazone (MYKROX, ZAROXOLYN)
• Minoxidil (LONITEN)
• Moexipril (UNIVASC, others)
• Nicardipine (CARDENE)
• Nifedipine (PROCARDIA ER)
• Nisoldipine (SULAR)
• Nitroprusside
• Olmesartan medoxomil (BENICAR)
• Perindopril (ACEON)
• Polythiazide (RENESE)
• Prazosin (MINIPRESS, others)
• Quinapril (ACCUPRIL, others)
• Quinethazone (HYDROMOX)
• Ramipril (ALTACE, others)
• Reserpine
• Spironolactone (ALDACTONE, others)
• Telmisartan (MICARDIS)
• Terazosin (HYTRIN and others)
• Terlipressin (LUCASSIN)
• Tolvaptan (SAMSCA)
• Torsemide (DEMADEX, others)
• Trandolapril (MAVIK, others)
• Triamterene (DYRENIUM)
• Triamterene/hydrochlorothiazide (DYAZIDE, MAXZIDE, others)
• Trichlormethiazide (NAQUA)
• Urea (UREAPHIL, currently not available in the United States)
• Valsartan (DIOVAN)
• Vasopressin (8-L-arginine vasopressin, PITRESSIN, others)
• Verapamil (CALAN, others)
MECHANISMS OF ACTION OF DIURETICS
A 43-year-old man has a blood pressure of 138/88 taken during his annual examination. He has no other health problems and his blood laboratory results are in the normal range. He is modestly overweight and has a family history of cardiovascular disease.
a. What, if any, are the therapeutic options for this patient?
This patient is considered to have prehypertension (see Table 15-1). It is appropriate to recommend nonpharmacological approaches to reduce his risk of developing hypertension. The lifestyle modifications that could lower this patient’s blood pressure include:
• Reduction in body weight
• Restricting sodium consumption (the Dietary Approaches to Stop Hypertension [DASH] diet may be particularly useful)
• Restriction of ethanol intake to modest levels
• Increased physical activity
OVERVIEW OF NEPHRON ANATOMY, NOMENCLATURE, AND FUNCTION (see Figure 25-1 in Goodman & Gilman’s The Pharmacological Basis of Therapeutics, 12th Edition)
• The basic urine-forming unit of the kidney is the nephron.
• The nephron consists of a filtering apparatus, the glomerulus, connected to a long tubule portion that reabsorbs substances the body must conserve, and leaves behind and/or secretes substances that must be eliminated.
• The nephron can be divided into 4 major anatomical and functional regions:
▶ The proximal tubule
▶ The loop of Henle (which consists of the proximal straight tubule, the intermediate tubule, the thick ascending limb)
▶ The distal convoluted tubule
▶ The collecting duct
• Normally ~65% of filtered Na+ is reabsorbed in the proximal tubule; this part of the tubule is highly permeable to water.
• Approximately 25% of filtered Na+ is reabsorbed in the loop of Henle.
• The distal convoluted tubule actively transports NaCl and is impermeable to water.
• The fine control of ultrafiltrate composition and volume takes place in the collecting duct.
• The transport that occurs in a specific segment of the nephron is primarily determined by the transporters present in the epithelial cells and the whether they are located on the luminal or basolateral membrane.
b. A year later at his next annual examination, the patient’s blood pressure is 142/91. What, if any, are the therapeutic options for this patient?
This patient’s prehypertension has progressed to stage 1 hypertension (see Table 15-1). In addition to emphasizing the importance of the lifestyle modifications listed above, this patient should be started on antihypertensive drug therapy.
c. What are the considerations in choosing an appropriate antihypertensive drug therapy for this patient?
Choice of an antihypertensive drug should be driven by the likely benefit in an individual patient, taking into account concomitant diseases such as diabetes mellitus, problematic adverse effects of specific drugs, and cost. National guidelines recommend diuretics as preferred initial therapy for most patients with uncomplicated stage 1 hypertension who are unresponsive to nonpharmacological measures. Patients also are commonly treated with other drugs (see Table 15-2): β receptor antagonists, ACE inhibitors/AT1-receptor antagonists, and Ca2+ channel blockers.
TABLE 15-2 Classification of Antihypertensive Drugs by Their Primary Site or Mechanism of Action
Diuretics
1. Thiazides and related agents (hydrochlorothiazide, chlorthalidone, chlorothiazide, indapamide, methylclothiazide, metolazone)
2. Loop diuretics (furosemide, bumetanide, torsemide, ethacrynic acid)
3. K+-sparing diuretics (amiloride, triamterene, spironolactone)
Sympatholytic drugs (see Chapter 7)
1. β receptor antagonists (metoprolol, atenolol, betaxolol, bisoprolol, carteolol, esmolol, nadolol, nebivolol, penbutolol, pindolol, propranolol, timolol)
2. α receptor antagonists (prazosin, terazosin, doxazosin, phenoxybenzamine, phentolamine)
3. Mixed α-β receptor antagonists (labetalol, carvedilol)
4. Centrally acting adrenergic agents (methyldopa, clonidine, guanabenz, guanfacine)
5. Adrenergic neuron blocking agents (guanadrel, reserpine)
Ca2+ channel blockers (verapamil, diltiazem, nisoldipine, felodipine, nicardipine, isradipine, amlodipine, clevidipine, nifedipinea)
Angiotensin-converting enzyme inhibitors (captopril, enalapril, lisinopril, quinapril, ramipril, benazepril, fosinopril, moexipril, perindopril, trandolapril)
AngII receptor antagonists (losartan, candesartan, irbesartan, valsartan, telmisartan, eprosartan, olmesartan)
Direct renin inhibitor (aliskiren)
Vasodilators
1. Arterial (hydralazine, minoxidil, diazoxide, fenoldopam)
2. Arterial and venous (nitroprusside)
aExtended-release nifedipine is approved for hypertension.
PRINCIPLES OF DIURETIC ACTION
• Diuretics increase the rate of urine flow.
• Clinically useful diuretics also increase the rate of Na+ excretion (natriuresis), as well as an anion such as Cl–.
• Most diuretics are used to reduce extracellular fluid volume by decreasing total NaCl content.
• With chronic diuretic administration, renal compensatory mechanisms adjust Na+ excretion to match Na+ intake (see Figure 25-5 in Goodman & Gilman’s The Pharmacological Basis of Therapeutics, 12th Edition).
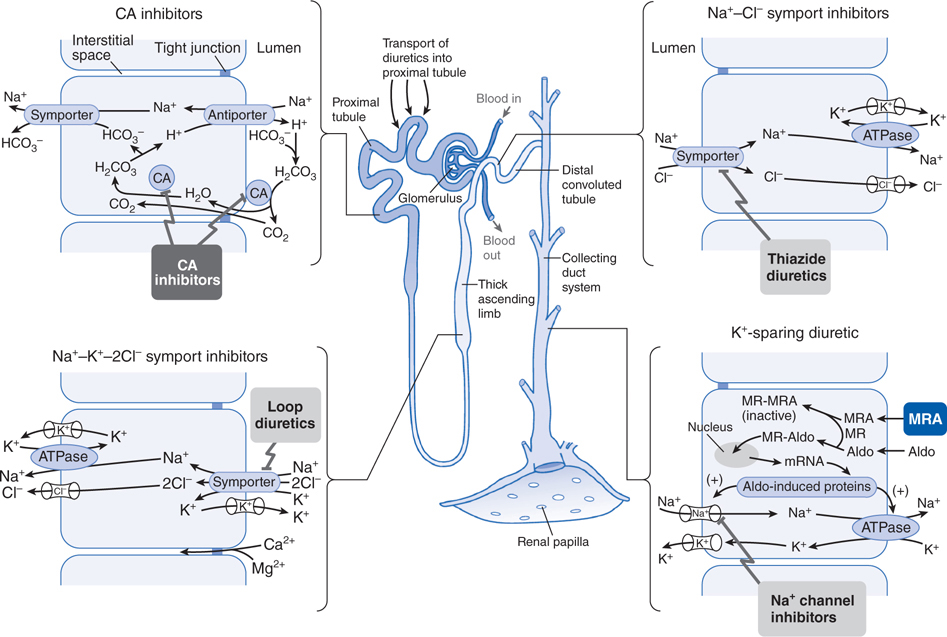
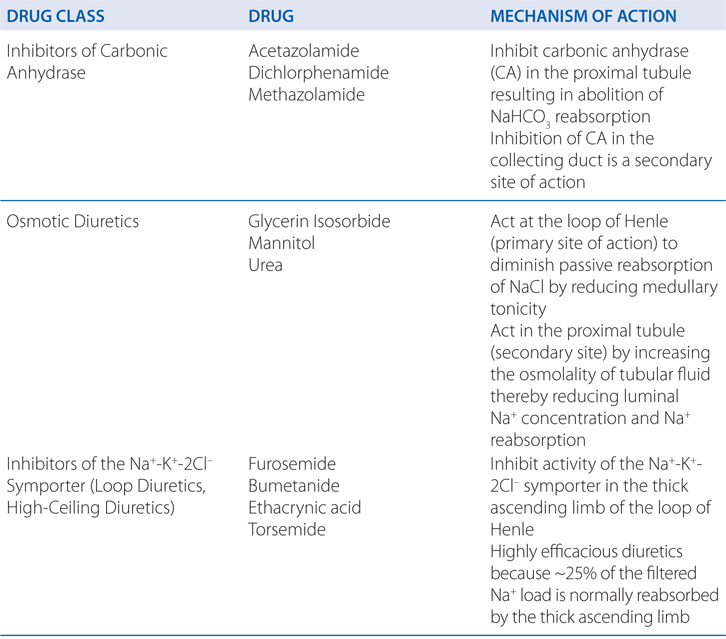
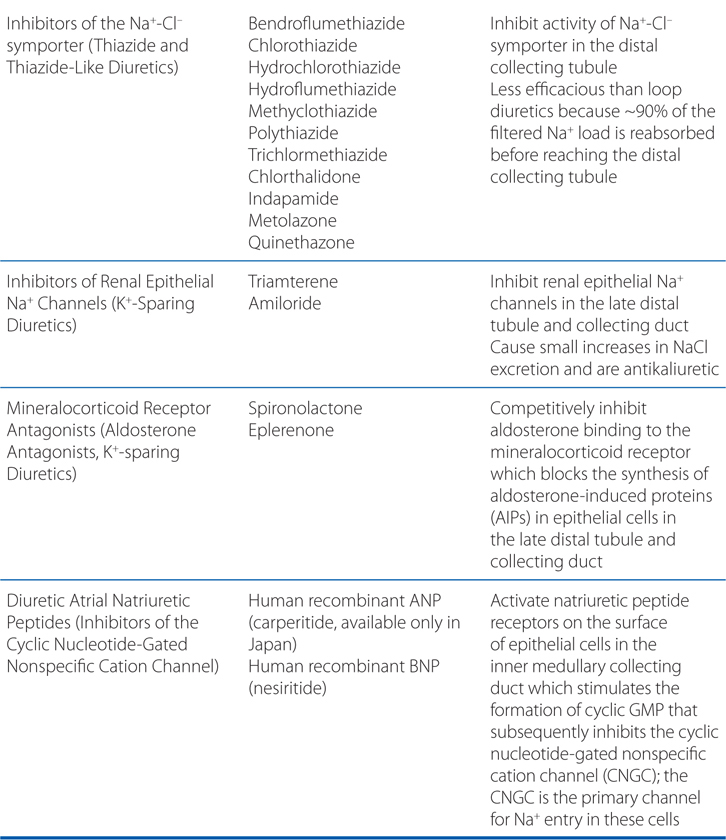
• Diuretics are classified based on their mechanism of action and their site of action in the nephron (Table 15-3 and Figure 15-1).
TABLE 15-3 Excretory and Renal Hemodynamic Effects of Diureticsa
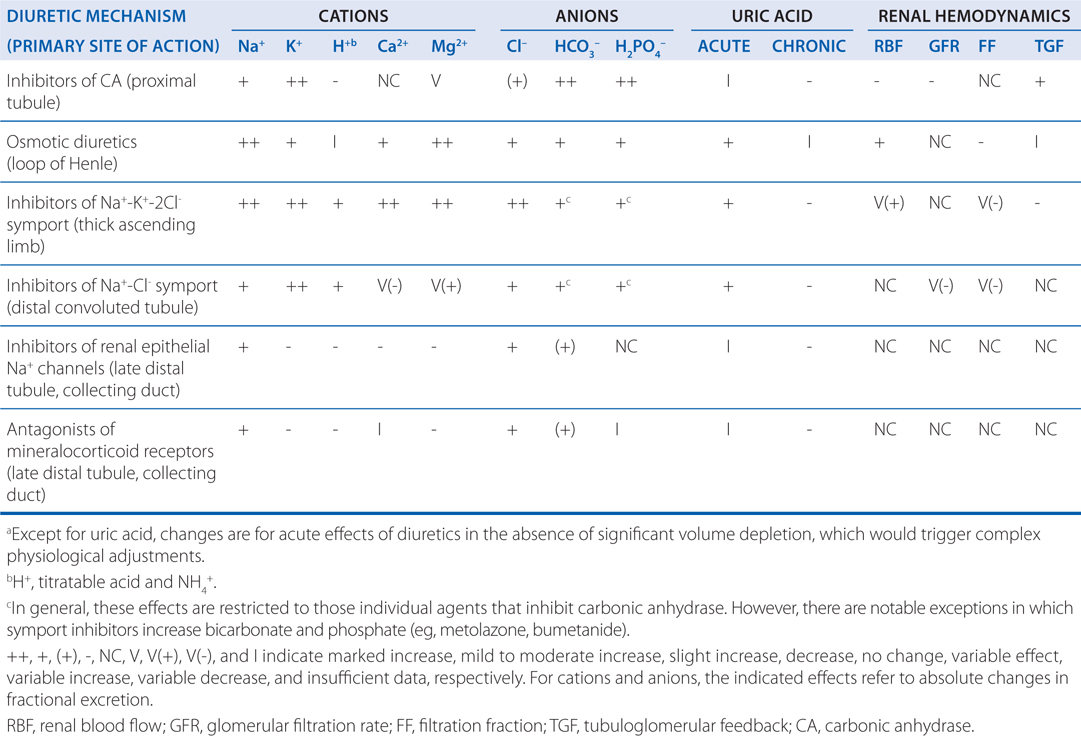
FIGURE 15-1 Summary of the site and mechanism of action of diuretics. Three important features of this summary figure are worth special note. 1. Transport of solute across epithelial cells in all nephron segments involves highly specialized proteins, which for the most part are apical and basolateral membrane integral proteins. 2. Diuretics target and block the action of epithelial proteins involved in solute transport. 3. The site and mechanism of action of a given class of diuretics are determined by the specific protein inhibited by the diuretic. Aldo, aldosterone; CA, carbonic anhydrase; MR, mineralocorticoid receptor; MRA, mineralocorticoid receptor antagonist.
d. He is prescribed hydrochlorothiazide (12.5 mg daily). What is the mechanism of action of this drug in reducing blood pressure?
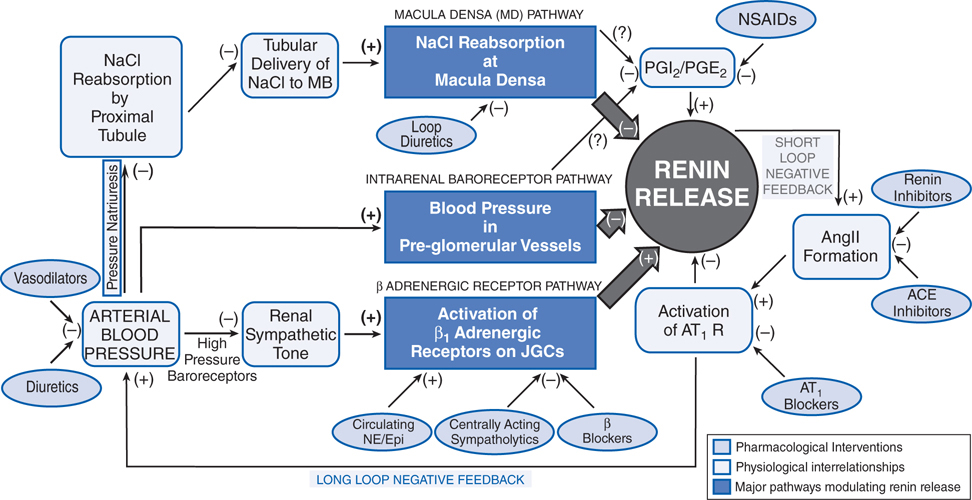
The initial action of the thiazide diuretics is to decrease extracellular volume by interacting with a thiazide-sensitive NaCl cotransporter expressed in the distal convoluted tubule in the kidney (see Figure 15-1), which enhances Na+ excretion in the urine, leading to a fall in cardiac output and a consequent reduction in mean arterial pressure. However, the hypotensive effect is maintained during long-term therapy due to decreased vascular resistance; cardiac output returns to pretreatment values and extracellular volume returns almost to normal due to compensatory responses such as activation of the renin-angiotensin system (RAS; Figure 15-2). The explanation for the long-term vasodilation induced by these drugs is unknown. Hydrochlorothiazide may open Ca2+-activated K+ channels, leading to hyperpolarization of vascular smooth muscle cells, which leads in turn to closing of L-type Ca2+ channels and lower probability of opening, resulting in decreased Ca2+ entry and reduced vasoconstriction. Hydrochlorothiazide also inhibits vascular carbonic anhydrase, which hypothetically may alter smooth muscle cell cytosolic pH and thereby cause opening of Ca2+-activated K+ channels with the consequences noted. The major action of thiazide diuretics on the NaCl cotransporter—expressed predominantly in the distal convoluted tubules and not in vascular smooth muscle or the heart—has contributed to repeated suggestions that these drugs decrease peripheral resistance as an indirect effect of negative sodium balance. That thiazides lose efficacy in treating hypertension in patients with co-existing renal insufficiency is compatible with this hypothesis.
FIGURE 15-2 Schematic portrayal of the 3 major physiological pathways regulating renin release. ACE, angiotensin-converting enzyme; AngII, angiotensin II; AT1 R, angiotensin subtype 1 receptor; JGCs, juxtaglomerular cells; MD, macula densa; NE/Epi, norepinephrine/epinephrine; NSAIDs, nonsteroidal anti-inflammatory drugs; PGI2/PGE2, prostaglandins I2 and E2.
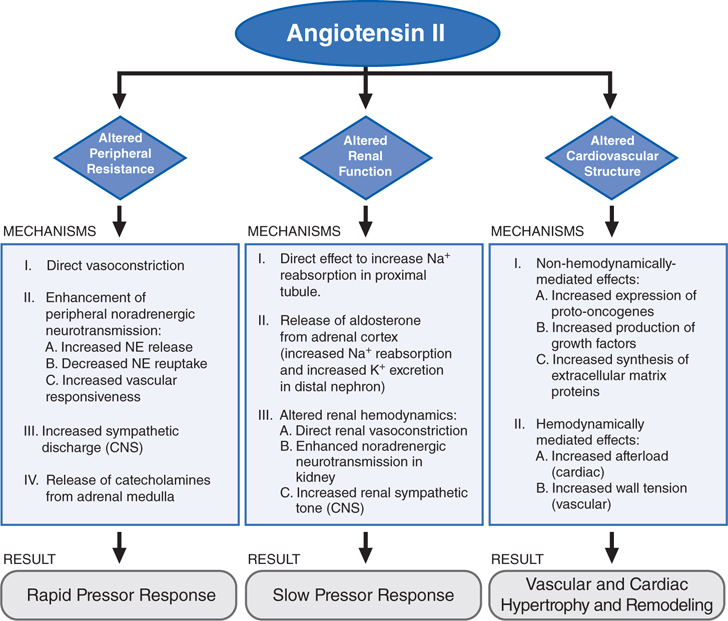
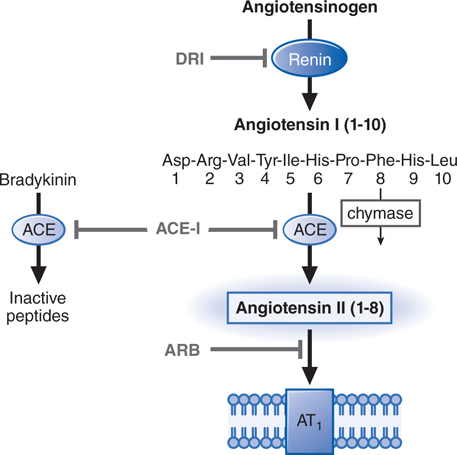
MECHANISMS OF ACTION OF INHIBITORS OF THE RENIN-ANGIOTENSIN SYSTEM (RAS; see Table 15-4)
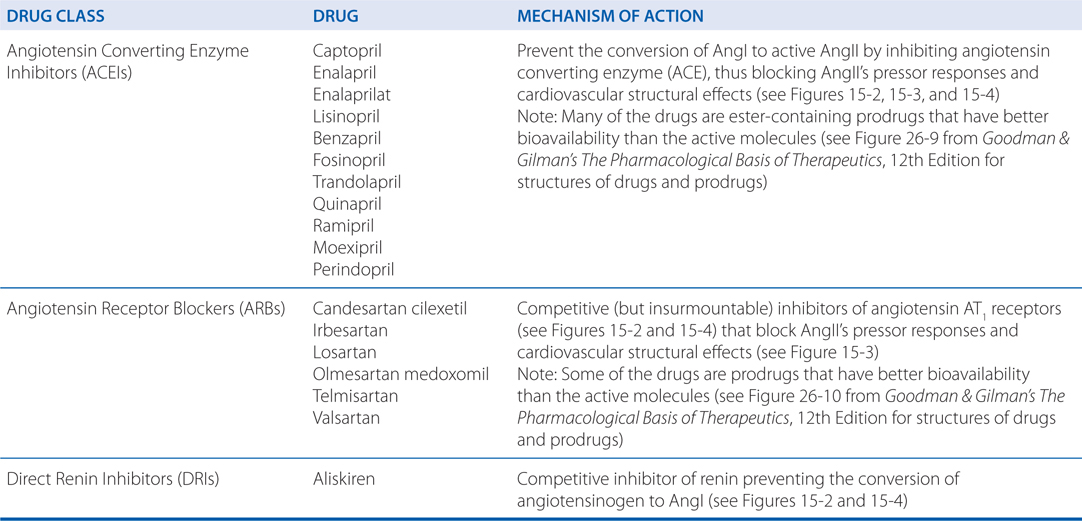
TABLE 15-4 Effects of Anti-hypertensive Agents on Components of the RAS
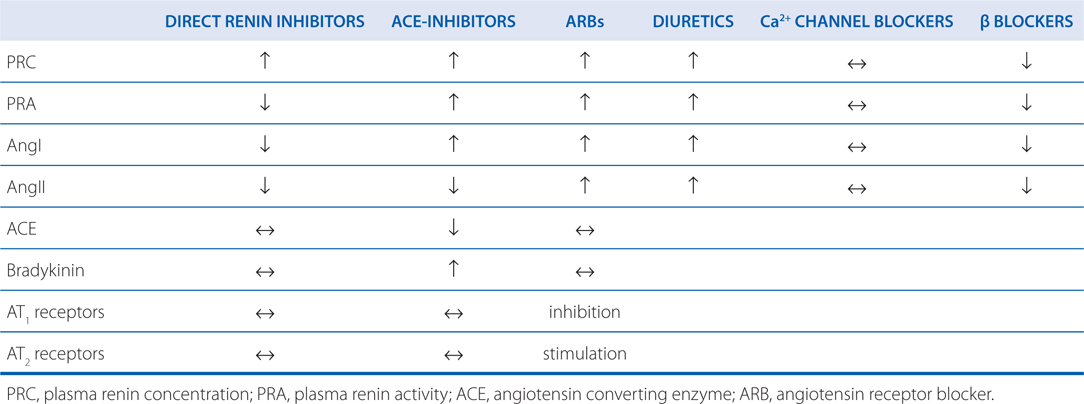
FIGURE 15-3 Summary of the 3 major effects of AngII and the mechanisms that mediate them. NE, norepinephrine.
FIGURE 15-4 Inhibitors of the RAS. ACE-I, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; DRI, direct renin inhibitor.
A 68-year-old woman is being treated with 25 mg of hydrochlorothiazide for her hypertension. During her most recent checkup, her blood pressure was 161/93 and she was also diagnosed with type 2 diabetes.
a. What changes should be made in her treatment?
This patient has stage 2 hypertension (see Table 15-1) and an important comorbidity, type 2 diabetes mellitus. The risk of cardiovascular disease, disability, and death in hypertensive patients is increased markedly by concomitant cigarette smoking, diabetes, or elevated low-density lipoprotein; the coexistence of hypertension with these risk factors increases cardiovascular morbidity and mortality to a degree that is compounded by each additional risk factor. Because the purpose of treating hypertension is to decrease cardiovascular risk, other dietary and pharmacological interventions may be required to treat these comorbid conditions. ACE inhibitors/AT1-receptor antagonists should be first-line drugs in the treatment of diabetics with hypertension in view of these drugs’ well-established benefits in slowing the development and progression of diabetic glomerulopathy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree