Chapter 4 Drug Interactions
Mechanisms of Drug Interactions
Pharmacokinetic Interactions
Absorption
A given drug may directly reduce the absorption of another drug through the following:
 Chelation
Chelation A chelator is an organic chemical that bonds with and removes free metal ions from solutions. Typically, the molecule being chelated will be a divalent cation (e.g., Ca+2, Mg+2, Fe+2).
A chelator is an organic chemical that bonds with and removes free metal ions from solutions. Typically, the molecule being chelated will be a divalent cation (e.g., Ca+2, Mg+2, Fe+2). There are a few examples of agents that chelate drugs, reducing the absorption of both. The classic example would be tetracycline, which is chelated by calcium. This can inhibit absorption of tetracycline, reducing its antibacterial activity, but perhaps more important, tetracycline can reduce the availability of calcium, which can have dramatic effects on the developing fetus.
There are a few examples of agents that chelate drugs, reducing the absorption of both. The classic example would be tetracycline, which is chelated by calcium. This can inhibit absorption of tetracycline, reducing its antibacterial activity, but perhaps more important, tetracycline can reduce the availability of calcium, which can have dramatic effects on the developing fetus. Binding
Binding Drugs may also bind other drugs, although this is a relatively rare interaction. The classic example would be cholestyramine, a positively charged drug used to lower cholesterol. It lowers cholesterol by binding to negatively charged bile acids in the gut. Consequently, cholestyramine is also capable of binding other negatively charged drugs in the gut.
Drugs may also bind other drugs, although this is a relatively rare interaction. The classic example would be cholestyramine, a positively charged drug used to lower cholesterol. It lowers cholesterol by binding to negatively charged bile acids in the gut. Consequently, cholestyramine is also capable of binding other negatively charged drugs in the gut.A given drug may also indirectly reduce absorption of another drug, by altering the following:
 GI motility
GI motility• Both drugs and food can alter gastrointestinal (GI) motility, enhancing or inhibiting the absorption of other agents.
 The small intestine, with its large surface area, is a key area for drug absorption. Drugs such as anticholinergics, which reduce GI motility, may reduce the rate of absorption by delaying gastric emptying. Slowing the rate of absorption may have an impact on drugs that we want to work quickly, such as analgesics.
The small intestine, with its large surface area, is a key area for drug absorption. Drugs such as anticholinergics, which reduce GI motility, may reduce the rate of absorption by delaying gastric emptying. Slowing the rate of absorption may have an impact on drugs that we want to work quickly, such as analgesics.
 The small intestine, with its large surface area, is a key area for drug absorption. Drugs such as anticholinergics, which reduce GI motility, may reduce the rate of absorption by delaying gastric emptying. Slowing the rate of absorption may have an impact on drugs that we want to work quickly, such as analgesics.
The small intestine, with its large surface area, is a key area for drug absorption. Drugs such as anticholinergics, which reduce GI motility, may reduce the rate of absorption by delaying gastric emptying. Slowing the rate of absorption may have an impact on drugs that we want to work quickly, such as analgesics. Transport proteins, such as P-glycoprotein (Pgp) (Figure 4-1)
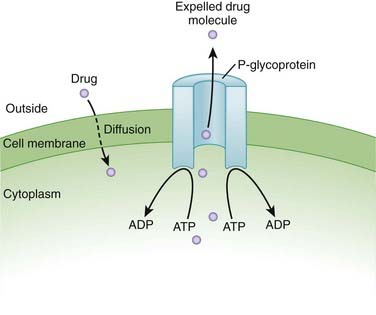
Transport proteins, such as P-glycoprotein (Pgp) (Figure 4-1)• Pgp is one member of a superfamily of efflux transporters that are found in several regions of the body, including the GI tract and the blood-brain barrier. Pgp extrudes drug from the cell (i.e., pumps drug out of the cell).
• In the cells lining the GI tract, these efflux pumps will therefore pump some of the drug that was going to be absorbed back into the GI tract, preventing a proportion of drug from being absorbed.
Metabolism
Phase I Reactions
Cytochrome P-450 Enzymes
Clinically significant drug interactions arise from either induction or inhibition of these enzymes.
Enzyme Inhibition
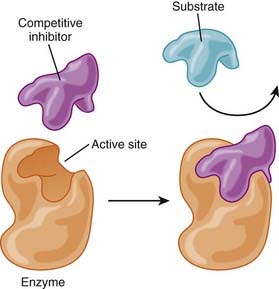
 Competitive inhibition (Figure 4-2)
Competitive inhibition (Figure 4-2) Two drugs are metabolized by the same enzyme system, and one of the drugs binds more readily to the enzyme, resulting in the inhibition of metabolism of the other drug.
Two drugs are metabolized by the same enzyme system, and one of the drugs binds more readily to the enzyme, resulting in the inhibition of metabolism of the other drug.Enzyme Induction
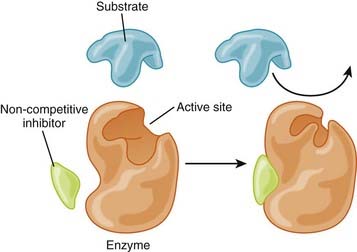
 If the drug is inactivated by that enzyme for the purpose of excretion, an inducer will result in reduced circulating levels of active drug. All things being equal, this will likely result in reduced biologic activity of the drug, perhaps leading to therapeutic failure.
If the drug is inactivated by that enzyme for the purpose of excretion, an inducer will result in reduced circulating levels of active drug. All things being equal, this will likely result in reduced biologic activity of the drug, perhaps leading to therapeutic failure. Most cases of induction are allosteric, although rarely a drug may also induce the enzyme system by which it is metabolized.
Most cases of induction are allosteric, although rarely a drug may also induce the enzyme system by which it is metabolized. What would happen if the patient discontinued drug B?
What would happen if the patient discontinued drug B?• This is a classic example of why monitoring should not end once an interacting drug has been discontinued. This is particularly important if the dose of drug A was increased in order to accommodate the effects of the enzyme inducer. If the dose is not adjusted back down, the patient might experience toxicity from the elevated plasma levels.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree