Drug-induced Acute Interstitial Nephritis
Neeraja Kambham, MD
Key Facts
Terminology
Acute tubulointerstitial inflammation due to allergic reaction to a drug
Etiology/Pathogenesis
T-cell-mediated hypersensitivity reaction
Idiosyncratic reaction, not dose dependent
Clinical Issues
Triad of fever, rash, eosinophilia in < 50%
Urine eosinophils
Subnephrotic proteinuria
Recovery of renal function in 60-90%
Microscopic Pathology
Interstitial inflammation with tubulitis, usually with eosinophils
Other features variably present
Granulomata
Fibrosis and atrophy with prolonged drug exposure
Minimal change disease: NSAIDs and others
Papillary necrosis: NSAIDs
Ancillary Tests
EM may show foot process effacement
TBM deposits by IF rarely
Top Differential Diagnoses
Acute tubular injury
Autoimmune AIN
Acute pyelonephritis
Granulomatous AIN due to infection or sarcoidosis
Diagnostic Checklist
Adverse prognostic features: Fibrosis, granulomata, marked inflammation
TERMINOLOGY
Abbreviations
Acute interstitial nephritis (AIN)
Synonyms
Drug-induced acute tubulointerstitial nephritis
Definitions
Acute tubulointerstitial inflammation due to allergic reaction to a drug
ETIOLOGY/PATHOGENESIS
Hypersensitivity Reaction
Usual mechanism believed to be T-cell mediated reaction
Often associated with systemic hypersensitivity manifestations
Idiosyncratic reaction, not dose dependent
Exacerbated response is seen with reexposure
Cross reactivity with similar class of drugs
Cell-mediated/Delayed Hypersensitivity Reaction
Positive skin tests to drug “haptens” can be seen in some patients
Oligoclonal T-cell reactivity to drug in vitro
Granuloma formation within interstitium
Drug molecules act as “haptens” and elicit immunological reaction
Drugs bind covalently to tubular basement membranes (TBM) or tubular epithelial cell components and alter or cross react with endogenous antigens
Antigen/Antibody-mediated Process (Immune Complexes)
Subset of cases have circulating antibodies to inciting drug (e.g., rifampin)
Anti-TBM autoantibodies are occasionally identified
IgE Mediated
IgE antibodies to drugs have been identified in some cases
Drug Classes Implicated
All drug classes have been implicated in AIN
Antibiotics
Penicillins, cephalosporins, sulfonamides, vancomycin, rifampin, tetracyclines, erythromycin and most others (if not all)
NSAIDs
Both COX-1 and COX-2 inhibitors
In some cases, AIN can occur after long-term exposure to NSAIDs
Prolonged use can cause analgesic nephropathy
Nonallergic mechanism of injury
Inhibit renal prostaglandin (vasodilator) synthesis
Nephrotoxicity greater with advancing age, dehydration, preexisting renal disease, cirrhosis
Can cause minimal change disease (secondary)
Diuretics
Thiazides, furosemide, triamterene
Miscellaneous drugs
Phenytoin, allopurinol, cimetidine, diphenylhydantoin, Chinese herbal medicines, captopril, lithium, valproate, warfarin, interferon-α, lamotrigine
Antiviral drugs
Acyclovir, foscarnet, indinavir
Other Possible Lesions to Accompany Drug-induced AIN
Granulomatous interstitial nephritis
Penicillins, polymyxin, rifampin, spiramycin, sulfonamides, vancomycin, acyclovir, thiazides, triamterene, NSAIDs, allopurinol, captopril, heroin, lamotrigine
Papillary necrosis
NSAIDs (acetaminophen, fenoprofen, ibuprofen, indomethacin)
Podocytopathy (minimal change disease)
Mechanism unknown
NSAIDs, penicillins, rifampin, celecoxib, diphenylhydantoin, lithium, interferon-
Membranous glomerulonephritis
NSAIDs, gold, penicillamine
CLINICAL ISSUES
Presentation
Maculopapular rash (˜ 25% of drug-induced AIN)
Onset usually a few days to weeks after drug exposure
Predominantly involves trunk and proximal extremities
Represents systemic manifestation of hypersensitivity reaction
Rash may be absent in NSAID-induced AIN
Fever (˜ 40%)
Arthralgias
Oliguria may be seen
Acute renal failure
Often nonoliguric
Older patients are more susceptible
Hypertension and pedal edema occasionally
Laboratory Tests
Blood
Elevated BUN and serum creatinine
Eosinophilia (˜ 35% > 500/mm3)
Serological studies are usually negative or normal (ANA, anti-DNA antibodies, ANCA, complement)
Urine
Sterile pyuria
WBC casts
Eosinophils in urine
Typical, but not specific to AIN
Proteinuria
Usually subnephrotic, < 1 g/day
Nephrotic range proteinuria may be seen with NSAIDs
Microscopic hematuria may be seen
Fractional excretion of sodium > 1%
Urine cultures are negative
Evidence of proximal and distal tubular defects
Aminoaciduria, glucosuria, phosphaturia, hyperkalemia, urine concentration defects
Natural History
Acute tubular injury and acute renal failure
Subset of untreated cases can progress to chronic renal failure
Treatment
Drugs
Removal of offending drug is 1st line of therapy
Steroid therapy may improve recovery of renal function, especially if started early
Supportive measures for acute renal insufficiency and renal failure
Prognosis
Excellent recovery of renal function in most cases (60-90%) within 1-12 months
Subset of patients are at risk for chronic renal insufficiency
Especially with prolonged intake of offending drug prior to diagnosis, as with over-the-counter NSAIDs
Minimal change disease resolves on discontinuance of drug but may recur on reexposure to same or similar drug
IMAGE FINDINGS
Ultrasonographic Findings
Enlarged kidneys may be seen in presence of interstitial edema
MACROSCOPIC FEATURES
General Features
Gross examination is uncommon as diagnosis is based on kidney biopsy
Enlarged kidneys due to interstitial edema
MICROSCOPIC PATHOLOGY
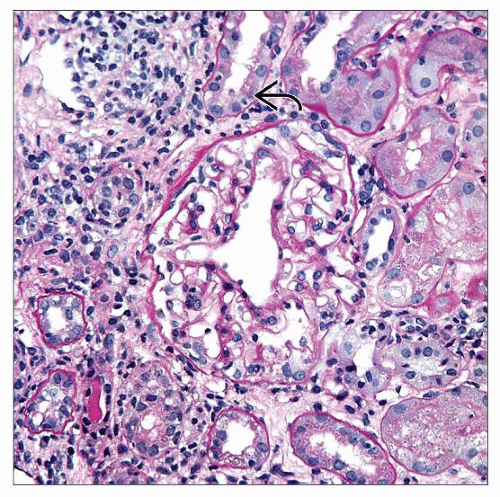
Histologic Features
Interstitial inflammation
Predominantly mononuclear cells, plasma cells, and fewer neutrophils
Eosinophils are usually present
Inflammation may be sparse in NSAID-induced AIN
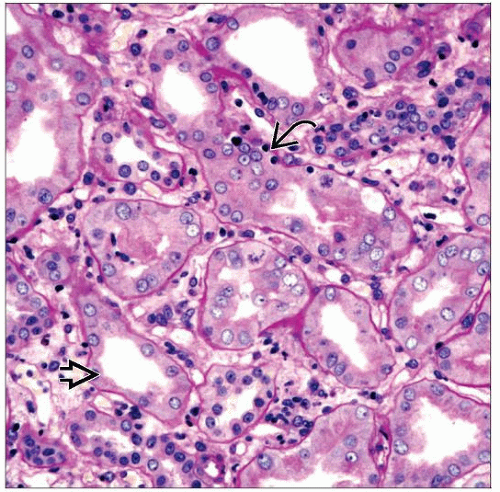
Tubulitis with infiltrating mononuclear inflammatory cells
Disruption of TBM may be seen on PAS stain
Reactive epithelial changes with sloughing, loss of brush border
Eosinophils in tubules
Interstitial edema
Granulomas in interstitium are not uncommon
Noncaseating granulomas with epithelioid histiocytes
Occasional multinucleated giant cells may be seen
Admixed with interspersed interstitial infiltrate
Drug hypersensitivity causes 45% of granulomatous interstitial nephritis in biopsies
Glomeruli and blood vessels are usually spared
Prominent tubular protein droplets
May be observed in cases of NSAID-induced coexistent minimal change disease
Chronic changes may be seen with prolonged use of offending drug
Mild interstitial fibrosis
Thickening of TBMs and tubular atrophy
Ureteral inflammation has been observed in nephrectomy specimens
ANCILLARY TESTS
Histochemistry
Acid-fast bacteria and Gomori methenamine silver
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree