Drainage of Hepatic, Subphrenic, and Subhepatic Abscesses
J. Wesley Alexander
Abscesses in the upper abdomen have played an important role in the morbidity and mortality of surgical patients throughout recorded history, having been described by Hippocrates about 400 BC. These can generally be divided into three types: hepatic, subhepatic, and subphrenic, which may differ in their etiology and treatment.
Hepatic Abscess
The classic paper on pyogenic abscess of the liver, written by Oschner, deBakey, and Murray in 1938, provides insights into some of the changes in etiology as well as treatment since the preantibiotic era. In that paper from Charity Hospital in New Orleans, three-fourths of the hepatic abscesses were amebic whereas the remainder were pyogenic. While amebic abscesses remain the most common cause of hepatic abscess worldwide, it is uncommonly encountered in the United States at the current time. In the preantibiotic era, there was definitely a higher frequency of multiple abscesses than now, most of them associated with pylephlebitis. The peak incidence was in patients 30 to 40 years of age. Both diagnosis and treatment have evolved markedly, but the signs and symptoms between the two periods are similar. In untreated cases now as then, mortality can approach 100%.
Abscesses of the liver are basically divided into three categories: pyogenic, amebic, and echinococcal. Echinococcal disease will not be discussed here as it will be presented in other chapters.
Pyogenic Liver Abscesses
Incidence
The incidence of pyogenic abscess of the liver in 1982 was 40 per 100,000 admissions in Germany, but in 1993, the incidence was 20 per 100,000 hospital admissions. It is less in the United States today (about 10/100,000 admissions), but 10 times or even higher in underdeveloped tropical countries. About 80% of liver abscesses in the United States are of the pyogenic type. Most of the patients (65%) are male in their 30s or 40s and about 60% to 75% occur in the right lobe.
Predisposing Factors
The most common underlying diseases associated with pyogenic liver abscess are shown in Table 1. Association with suppurative appendicitis was once the most common predisposing condition but biliary disease is now the most common and involves direct contamination of the biliary tree, usually with obstruction from stones in the common or hepatic ducts, strictures, or malignancies. Abscess can occur from direct extension from a diseased gallbladder. Cholangitis after endoscopic retrograde cholangiopancreatography (ERCP) is an increasing problem as is the increase in performance of complicated procedures associated with a biliary–intestinal anastomosis. Even the presence of an ascaris in the bile ducts has been related to obstruction.
The presence of pylephlebitis from a variety of causes has been of decreasing importance during the past few decades. Pylephlebitis can be associated with appendicitis, diverticulitis, inflammatory bowel disease (especially Crohn’s), pelvic inflammatory disease, and cancer. These abscesses may be
multiple and small, sometimes having the gross appearance of metastatic disease. Pylephlebitis associated with appendicitis was once a common condition, but is now encountered rarely. Treatment of local malignant lesions within the liver by cryotherapy, radiofrequency ablation, or localized chemotherapy is being used increasingly and can cause necrosis, predisposing to infection caused by direct contamination or from blood-borne sources. Even poor dental hygiene has been implicated in pyogenic hepatic abscess, especially in the presence of other pathology such as benign cysts or dead tissue. However, almost a third of the cases cannot be associated with an identified contributing factor.
multiple and small, sometimes having the gross appearance of metastatic disease. Pylephlebitis associated with appendicitis was once a common condition, but is now encountered rarely. Treatment of local malignant lesions within the liver by cryotherapy, radiofrequency ablation, or localized chemotherapy is being used increasingly and can cause necrosis, predisposing to infection caused by direct contamination or from blood-borne sources. Even poor dental hygiene has been implicated in pyogenic hepatic abscess, especially in the presence of other pathology such as benign cysts or dead tissue. However, almost a third of the cases cannot be associated with an identified contributing factor.
Table 1 Selected Underlying Diseases Associated with Pyogenic Liver Abscess | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Diagnosis
Most of the signs and symptoms associated with pyogenic liver abscesses are nonspecific: enlarged and tender liver, fever (about 90%), loss of appetite, pain, and tenderness are common. These contribute only to a high level of suspicion rather than a specific diagnosis. If an abscess is suspected, an ultrasound of the upper abdomen is usually helpful. Many other tests such as magnetic resonance imaging (MRI) and labeled leukocyte scintigraphy may also be supportive, but the most definitive method for diagnosis is computerized tomography (CT), especially when combined with ultrasonography.
Microbial Pathogens
As might be expected from the predisposing conditions, most of the infections are polymicrobial with both aerobic and anaerobic organisms. The most common anaerobes are Bacteroides species and the most common aerobic Gram-negative organisms are Klebsiella and Escherichia. The most common Gram-positive bacteria are Enterococcus and microaerophilic Streptococcus. Thus, very broad spectrum antibiotic coverage is necessary initially and needs to be revised as determined by sensitivities. Choice of antibiotics is discussed elsewhere in this text. Since many of the organisms in the intestinal tract are not culturable, Gram stains are an important part of the evaluation.
Treatment
All pyogenic liver abscesses should be treated with broad-spectrum antibiotics, which cover both Gram-negative and Gram-positive organisms as well as aerobic and anaerobic organisms, unless otherwise indicated by specific culture and sensitivity. Metronidazole is usually included initially to cover both amebic and anaerobic organisms.
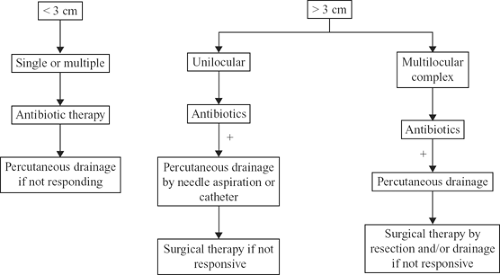
The second necessary component of treatment is to remove the infected material to the extent possible. Numerous articles have been written in the last few years, which have attempted to define the therapeutic role of aspiration versus open surgical procedures. It is now clear that both single or multiple needle aspirations of individual abscesses as well as percutaneous drainage are viable therapeutic options for most cases and should be attempted first when technically safe. Hope et al. have provided a reasonable algorithm for treatment (Fig. 1). For small abscesses, less than 2 to 3 cm, whether single or multiple, antibiotic therapy alone should be attempted first. Direct injection of antibiotics into the abscessed cavity has been described and seems reasonable, but needs further evaluation. For unilocular abscesses greater than 3 cm, either repeated needle aspiration or percutaneous catheter drainage should be attempted before surgery, which results in success rates of 80% to 97%. Some reports suggest that abscesses greater than 10 cm should initially be treated surgically. However, there are certainly enough reports of good results with percutaneous catheter drainage to indicate that it should be given a trial before open surgical drainage when anatomically safe. Most reports indicate that large multilocular abscesses do not respond to percutaneous drainage and may be a prognostic factor. If there is no prompt response to catheter drainage, surgical treatment should be used. Many cases in this category also have underlying biliary tract disease. When there is persistent structural damage to the intrahepatic biliary tree, resection is often necessary. Transphrenic fistulization to the bronchus will usually require open surgery for closure. In patients who require surgical intervention for other underlying problems, drainage or excision of the abscess at the same time should always be considered.
Surgical Intervention
Less than 15% of cases will require surgical drainage. Laparoscopic approaches have been described and may be successful in some cases and a prudent option in cases of rupture. Once the abscess is drained, it
should be treated with closed-suction drainage and continued intensive antibiotic therapy. In the author’s opinion, it is more desirable to perform an extraserosal drainage whenever possible. The technique for open drainage will be described later.
should be treated with closed-suction drainage and continued intensive antibiotic therapy. In the author’s opinion, it is more desirable to perform an extraserosal drainage whenever possible. The technique for open drainage will be described later.
Amebic Liver Abscesses
Worldwide, amebic abscesses are more common than pyogenic abscesses although they are becoming less frequent, especially in developed and emerging countries. Risk factors include old age, malnutrition, immunosuppression, and recent travel to tropical regions, especially where there is poor sanitation. Amebic liver abscesses may be considerably different from pyogenic liver abscesses although many are indeterminant even after extensive testing. In general, they are more often solitary (>90%), occur more often in the right lobe (75% to 90%), are more common in males (90%), have a more insidious onset, are usually larger than pyogenic abscesses, are more likely to rupture, and are more responsive to antibiotic therapy. The diagnosis may be made by the presence of ameba on stains of aspirated fluid from the abscess, which is typically reddish brown (anchovy paste–like), and/or high titers of IgG antiamebic antibody by enzyme-linked immunosorbent assay (ELISA). When negative, the test should be repeated after 1 to 2 weeks to allow time for a better immune response. Once a tentative diagnosis is made, metronidazole is the drug of choice and should be given for 14 days (with >80% resolution). Chloroquine and dehydroemetine are added by many authorities if there is no improvement within 72 to 96 hours. Intestinal cysts may not be killed by antibiotics and should also be treated with paromomycin. Small cysts (<5 cm) may be treated by antibiotics alone, but larger cysts or those not responding to antibiotics should be treated by needle aspiration, sometimes repeatedly. When needle aspirations fail, percutaneous catheter aspiration should be used. Percutaneous drainage associated with intralesional chemotherapy may result in a better clinical response. Open surgical drainage is necessary infrequently, mostly for ruptured or complicated abscesses or when insertion of percutaneous catheters is hazardous. Perforation of these cysts is not infrequent (22% in one series), and most commonly occurs into the pleuropulmonary structures or into the subphrenic space or peritoneal cavity. Ruptured abscesses should be treated additionally with percutaneous catheter drainage, although percutaneous drainage is rarely necessary for survival after rupture.
Subphrenic and Subhepatic Abscesses
Since the etiology and treatment of subphrenic and subhepatic abscesses are similar, they will be discussed together. The major underlying conditions associated with these types of abscesses are shown in Table 2. Symptoms, physical signs, and laboratory results are similar to hepatic abscesses and not specific.
Infections of the subhepatic space are most often associated with disease of the gallbladder and biliary tree. Because of the increased use of laparoscopic cholecystectomy, there is an increasing incidence of abscesses associated with gallstones that were spilled but not retrieved at the time of the initial operation. Quite obviously, prevention can be best accomplished with meticulous removal of such stones at the original operation. Suppurative cholecystitis is another important source of subhepatic abscess, but abscesses in the subhepatic space can occur with any intestinal perforation or infection that reaches the upper peritoneal cavity. Indeed, 80% of subhepatic and subphrenic abscesses are associated with intra-abdominal surgery. Splenic abscesses with or without rupture, and in some cases pancreatitis, are also important etiologic factors for subphrenic abscess. Diagnosis and treatment of the underlying conditions are obviously of great importance for successful management of the abscess. A perforated viscous must be repaired or a necrotic appendix must be removed or the patient will continue to be septic. Although some cases of pancreatitis may result in subhepatic or subphrenic abscesses, this topic will not be discussed here because the issues involved in pancreatic abscesses are generally different.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree