Dorsalis Pedis, Tarsal, and Plantar Artery Bypass
Frank B. Pomposelli
Bernadette Aulivola
Introduction
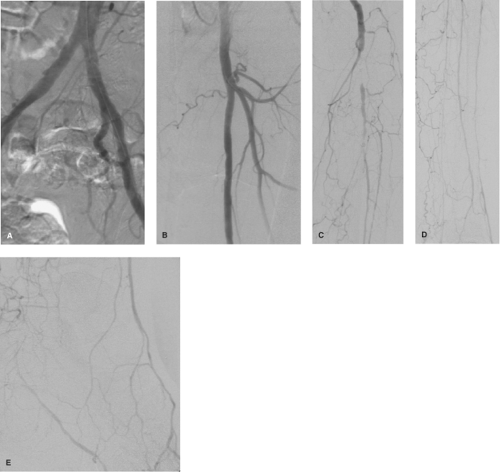
Arterial reconstruction to the arteries of the distal ankle and foot has become commonplace in those patients with occlusive disease of the infrapopliteal vessels, precluding bypass to a more proximal target vessel. This is especially the case in patients with diabetes mellitus presenting with ischemic foot lesions due to a characteristic pattern of occlusive disease, where the tibial and peroneal arteries are occluded but the foot vessels, especially the dorsalis pedis artery, remain patent (Fig. 1). In our early experience, extending vein bypass grafts to the dorsalis pedis artery (DP bypass) when no other vessel was patent expanded our ability to salvage limbs in patients who would otherwise have required amputation. Our initial results with these patients were impressive enough that we standardized our technique and began performing DP bypass in patients in preference to other more proximal target arteries. We also found that pedal bypass could be performed safely in patients presenting with foot infection and ischemia and worked well for healing heel ulcers. In the era preceding the widespread application of endovascular therapy for limb ischemia, pedal bypass comprised 30% of all limb salvage bypasses done in our practice, which was comprised of a large proportion of diabetic patients due to our longstanding affiliation with the Joslin Diabetes Center.
As is the case in other vascular domains, endovascular options for treatment of tibial vessel occlusive disease have been increasingly investigated and reported over the past several years. Our own experience with infrapopliteal angioplasty and selective stenting in 176 limbs over a 3-year period revealed that this treatment is a technically feasible, and a reasonable option for revascularization of the ischemic foot in many patients. However, technical success was decreased with progressive TransAtlantic Intersociety Consensus (TASC) classification severity (Table 1). Technical success was 93% overall, but decreased from 100% in TASC A, B, and C lesions to 75% in TASC D lesions. Infrapopliteal angioplasty patency rates at 1 and 2 years were inferior to that noted in the surgical bypass population, and presumably would decline further with a longer duration of follow up. Extensive tibial occlusive disease has proven to
be the most common pattern encountered, underscoring the continued importance of extreme distal bypass to the foot arteries in limb salvage for foot ischemia in these patients. This chapter will outline our evaluation and approach to foot-level arterial bypass for limb salvage.
be the most common pattern encountered, underscoring the continued importance of extreme distal bypass to the foot arteries in limb salvage for foot ischemia in these patients. This chapter will outline our evaluation and approach to foot-level arterial bypass for limb salvage.
Arterial insufficiency can present with a spectrum of clinical signs and symptoms. In some patients, arterial insufficiency may be completely asymptomatic, diagnosed on the basis of nonpalpable foot pulses alone. As chronic arterial insufficiency progressively worsens, patients may present with symptoms of intermittent claudication, which manifests typically as cramping or tiredness in the calves with walking, relieved by rest. More severe symptoms of arterial insufficiency are categorized as critical limb ischemia, which can present as ischemic rest pain or tissue loss. Tissue loss represents the most severe manifestation if critical limb ischemia and may present as nonhealing ulceration or gangrene. This chapter focuses on revascularization in patients presenting with critical limb ischemia. Often, in the diabetic population, critical limb ischemia is noted in patients with no discernable history of prior claudication. This illustrates that the development of severe critical limb ischemia does not always follow an orderly progression through each stage of ischemia severity.
Table 1 Transatlantic Inter-Society Consensus (TASC) Classification of Occlusive Disease in the Tibial Arteries | |||||
|---|---|---|---|---|---|
|
Patient Selection
Foot-level arterial bypass is reserved for patients with limb-threatening ischemic symptoms including rest pain, nonhealing ulcers, gangrene, or poor healing of toe amputations or other foot surgery. These revascularization procedures are not appropriate for the treatment of intermittent claudication. In fact, claudication is rarely improved by pedal level bypass, since the arteries of
the calf are occluded and rarely adequately perfused through the pedal circulation.
the calf are occluded and rarely adequately perfused through the pedal circulation.
Patients with extensive tissue loss, in whom lower extremity revascularization is considered, may be evaluated by a podiatrist to confirm options for foot salvageability preoperatively. If progression of ulceration or gangrene precludes salvage of the foot, revascularization may be contraindicated, as the patient may be best served with primary major amputation. It is important to keep in mind that foot salvageability is dependent not only on adequate arterial perfusion, but also on adequate nutritional support and treatment of concomitant foot infection with antibiotics and possible incision and drainage. Foot salvage also, at times, requires toe, ray, or other minor foot amputations to achieve infection control and healing. The confirmation of an arterial bypass target vessel is a prerequisite to planning inframalleolar bypass. This is generally achieved by performance of preoperative imaging studies of the lower extremity arterial system. In very rare cases, when no suitable bypass target artery is identified, the patient may not be a suitable candidate for revascularization.
Comprehensive, high-quality intra-arterial digital subtraction angiography (DSA) is a key component in the planning process for DP or other inframalleolar vessel bypass (Fig. 1). Appropriate evaluation of the lower extremity circulation includes imaging of the entire arterial tree from the renal arteries to the base of the toes in all patients with critical limb ischemia. Proper imaging of the foot vessels requires magnified anteroposterior and lateral views in order to fully appreciate the quality of the DP, tarsal, and plantar arteries to assess their potential use as outflow target vessels. Magnetic resonance angiography (MRA) is used infrequently in our practice, and is generally reserved for those patients who are unable to undergo DSA, some due to severe contrast allergies. Some data suggest that occult foot vessels on DSA may be unmasked with MRA, resulting in successful bypass to these vessels. “Blind” operative exploration may also be performed in the case of nonvisible foot arteries on DSA in cases where patency is suspected on the basis of an audible Doppler signal, although this is rarely required due to the precise imaging capabilities of modern DSA. The less invasive nature of MRA makes it a more attractive imaging option in certain patients. In the past, MRA was considered a safer option than DSA for arterial imaging in the patient with chronic renal insufficiency given the risk of iodinated contrast-induced nephropathy with DSA. However, more recent data suggest that gadolinium-induced nephrogenic systemic fibrosis and acute renal insufficiency are more common than previously noted. Nearly all patients in our practice undergo intra-arterial DSA imaging prior to lower extremity bypass surgery.
Given that many patients with tibial artery occlusive disease have diabetes and chronic renal insufficiency, care must be taken to perform arterial imaging in the safest way possible. This often entails taking precautionary measures prior to DSA imaging. In patients with a creatinine level of ≥1.5 mg/dL or an estimated glomerular filtration rate (GFR) of <30 mL/min/1.73 m2, corresponding to Stage 4 or 5 chronic kidney disease, premedication with N-acetylcysteine, intravenous fluid hydration, and sodium bicarbonate infusion should be considered. Our protocol for premedication with N-acetylcysteine includes an oral dose of 600 mg of a 20% solution administered twice daily on the day before and the day of the procedure. Sodium bicarbonate infusion has been demonstrated to have a more significant protective effect against contrast-induced nephropathy than sodium chloride infusion. The protocol for sodium bicarbonate infusion utilizes a 150 mEq/L sodium bicarbonate in D5 W solution administered as a bolus of 3 mL/kg/h for 1 hour prior to the procedure and 1 mL/kg/h for 6 hours after the procedure.
The decision to perform inframalleolar bypass is made on the basis of several important anatomic and clinical factors. The goal of restoring a palpable foot pulse when possible in patients with diabetes and tissue loss is based upon our observation that this end point most reliably leads to healing and foot salvage in the setting of the compromised biology of the ischemic diabetic foot. If a more proximal outflow target artery cannot achieve that goal, preferential bypass to the DP artery should be considered. In situations of ischemic rest pain without tissue loss, the DP artery should be chosen as the outflow target vessel when it is the best-quality vessel for bypass or the only available outflow vessel as determined on DSA evaluation. In circumstances where a more proximal outflow vessel would restore a palpable foot pulse and tissue loss is the indication, DP bypass is not necessarily the procedure of choice. In cases of tissue loss or gangrene, however, DP bypass is often chosen in preference to a patent peroneal artery, given the technical ease of this bypass configuration. However, when the peroneal artery is evaluated to be a superior target vessel to the DP artery on DSA, or when the length of available autogenous vein conduit is inadequate for bypass to the DP artery, peroneal bypass is performed. In cases of severe dorsal foot infection, or when the indication for arterial reconstruction is claudication alone, DP bypass is not preferentially performed. Bypass to the tarsal or plantar arteries is indicated less frequently and is generally preserved for cases in which the DP artery is not a viable option for bypass outflow.
Many limbs requiring DP, tarsal, or plantar artery bypass have undergone previous ipsilateral limb revascularization. In our own published collection of 98 tarsal or plantar bypasses over a 13-year period, approximately 18% had undergone previous bypass procedures and 5% had undergone previous DP bypass on the ipsilateral extremity. The most frequent indication for bypass in these patients was tissue loss present in 95%, with ischemic rest pain in an additional 3%, and failing graft in 2%. All cases of tarsal or plantar artery bypass had no other reasonable bypass outflow target, including the DP artery.
In addition to DSA imaging of the affected extremity, preoperative planning includes routine duplex vein mapping for assessment of the most appropriate vein conduit for bypass graft use. In some cases, the availability of autogenous vein conduit may alter anatomic planning for inframalleolar level bypasses. In our experience, patients presenting for inframalleolar arterial reconstruction have undergone ipsilateral lower extremity revascularization in approximately 18% of cases and coronary artery bypass grafting in just over 20% of cases. Given their prior history of other revascularization procedures, ipsilateral greater saphenous vein, the conduit of choice, is not always available for use. Our preoperative venous mapping protocol includes evaluation of bilateral greater and lesser saphenous veins and, when indicated, evaluation of bilateral upper extremity basilic and cephalic veins. When ipsilateral greater saphenous vein is not available for use, contralateral greater saphenous or arm vein may be used as bypass conduit. Venous mapping provides crucial information regarding possible vein conduit, including vein diameter and the presence of vein thrombosis or sclerosis. Vein diameter of >2 mm is desirable for adequate conduit. Especially in the upper extremity veins, which have typically undergone multiple punctures for blood draws or intravenous lines, preoperative venous mapping provides critical information regarding the condition of the vein. In patients with end-stage renal disease on hemodialysis, arm vein is generally not considered as a conduit
option. Venous mapping can also be used to plan composite vein conduit construction to yield adequate total length to bridge between the inflow and outflow target vessels.
option. Venous mapping can also be used to plan composite vein conduit construction to yield adequate total length to bridge between the inflow and outflow target vessels.
Dorsalis Pedis Artery Bypass
The overall strategy of DP bypass is designed to simplify the procedure and minimize the use of prosthetic graft material. The key principles include the use of distal inflow artery sites and short, translocated, greater saphenous vein grafts, whenever possible. Short vein grafts with distal inflow have been demonstrated to result in acceptable limb salvage even in the face of poor arterial runoff and high outflow resistance. In rare cases of questionable adequacy or patency of an inframalleolar artery for bypass outflow, exploration of the target artery may be performed first such that extensive dissection is not carried out only to realize that the outflow vessel is inadequate.
Bypass procedures originating from the femoral level with an intact greater saphenous vein are well suited for use of the in situ technique with angioscopy for valve lysis under direct visualization. Vein tributaries are ligated with silk suture. The length of saphenous vein needed is confirmed. The saphenofemoral junction is divided and the stump on the femoral vein is oversewn with a silk suture ligature. The saphenous vein is divided distally at the appropriate location. The use of an angioscope with a pump irrigation system facilitates valve lysis and allows for thorough evaluation of the vein conduit for webs or stenoses. The angioscope is inserted into the proximal end of the vein graft and a long flexible valvulotome is inserted from the distal end for valve lysis and vein graft inspection prior to performing the anastomoses (Fig. 2). Use of the pump irrigation system has been shown to decrease the amount of crystalloid infused while aiding in the clarity of the angioscopic examination. When transposed vein conduit is used, the vein may be harvested and angioscopy and valve lysis may be performed on a side table prior to performing the anastomoses. When the greater saphenous vein is unavailable, unusable, or of inadequate length, contralateral saphenous vein is preferred, provided the contralateral leg has normal or near-normal arterial circulation. When contralateral ischemia is present, arm vein is the preferred source of alternative conduit. When arm vein is not available, the lesser saphenous vein may be used if the caliber and quality are thought to be adequate. Composite grafts composed of multiple vein segments may also be used, but are only required on occasion. The quality of arm and composite vein conduits should be evaluated with angioscopy. Vein conduit may be utilized in a reversed, nonreversed, or in situ fashion, although preference to in situ conduit exists for bypasses with inflow at the femoral level. For translocated vein conduit, the reversed vein technique is used if the distal vein is of greater caliber; otherwise the vein is positioned in the nonreversed orientation after valve lysis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree