Distal Gastrectomy with Billroth I or Billroth Ii Reconstruction
Rudolf Bumm
J. Rüdiger Siewert
Partial gastrectomies consist of the removal of the distal portion of the stomach. According to the type of disease (ulcer or carcinoma) and the location of the basic disease (duodenal ulcer, gastric ulcer, high-gastric ulcer), they are performed as antral, two-thirds, four-fifths, or high subtotal gastrectomy. Distal partial gastrectomy is named according to the type of anastomosis between the small intestine and the gastric remnant, regardless of the extent of the gastrectomy.
The Billroth I (BI) operation is a gastroduodenostomy that can be performed end-to-end or end-to-side. In the Billroth II (BII) reconstruction the gastrojejunostomy is performed end-to-side. As an alternative, Roux-Y (RY) reconstructions can be done (see Chapter 82). A decisive difference between the BI and BII procedure is that in BI reconstruction the duodenal passage remains intact. Because of anastomotic requirements, the BI operation is, as a rule, performed as an antrectomy. Gastroduodenostomy is difficult or impossible after more extended gastrectomies, because direct anastomoses between gastric fundus and duodenum may not be free of tension and followed by postoperative complications. Therefore, for the more extended partial gastrectomy, a BII or RY reconstruction should be favored. Furthermore, it is an interesting but unexplained clinical impression that mobility of the duodenum seems to be better in women and one can do a BI with greater resections than with males.
Historical Note
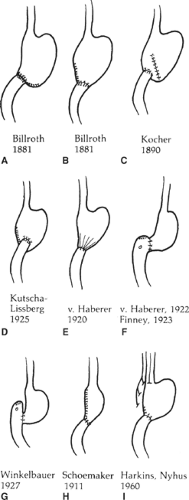
Pean and Rydigier attempted partial gastrectomies in 1879 and 1880, respectively, with neither of their patients surviving. Theodor Billroth performed the first successful partial gastrectomy on a patient who had antral carcinoma in 1881. He reconstructed the gastrointestinal passage by a superior end-to-end gastroduodenostomy with the duodenum anastomosed to the lesser curvature side of the stomach (Fig. 1A). Billroth later changed his surgical technique by effecting the anastomosis to the greater curvature (Fig. 1B). The reconstruction of the gastroduodenal passage in the BI operation has undergone numerous modifications. The end-to-end anastomosis (EEA) was performed as a posterior or anterior gastroduodenostomy, or the duodenal end was connected to the entire circumference of the cut edge of the stomach (Fig. 1C to E). End-to-side gastroduodenostomy was performed by anastomosing the stomach to the side of the duodenum opposite the major duodenal papilla or entirely below the level of the papilla (Fig. 1F, G). Further modifications are the tube-shaped resection for ulcers high on the stomach and subsequent reanastomosis of the duodenum to the greater curvature side of the stomach (Fig. 1H), and antrectomy performed in combination with gastric vagotomy and followed by an EEA (Fig. 2).
The technique most frequently used today is the Schoemaker modification of the BI operation, with partial closure of the stomach remnant along the lesser curvature and an inferior gastroduodenostomy.
Arguments in Favor of Bi Gastrectomy
A leading argument in favor of BI anastomosis as compared with other forms of gastrectomy (e.g., BII) is the preservation of the duodenal passage. The question arises as to whether the important functions of the duodenum are dependent on the presence (or absence) of the food passage.
Acids are neutralized in the duodenum by pancreatic and duodenal bicarbonate through neural and hormonal regulation. After distal stomach resection, this regulation is disturbed regardless of the type of anastomosis. Proportioned, regulated stomach emptying is no longer possible because the antrum and pylorus are gone, and the value of providing a duodenal passage cannot
be properly assessed because rapid and uncoordinated emptying of the stomach precludes the function of the digestive process that normally takes place in the duodenum. However, the benefit of the duodenal passage is clearer with regard to the function of the pancreas, the changes in the stomach remnant, and the function of the cardia.
be properly assessed because rapid and uncoordinated emptying of the stomach precludes the function of the digestive process that normally takes place in the duodenum. However, the benefit of the duodenal passage is clearer with regard to the function of the pancreas, the changes in the stomach remnant, and the function of the cardia.
The duodenal brake, a mechanism for shutting off acid, does not operate even if food passes the duodenum because of the denervation of transection. However, release of hormones in the duodenum does not necessarily require innervation. Better absorption of calcium and iron in the duodenum are proven advantages of the BI hookup.
Experimental and clinical investigations indicate undisturbed pancreatic function, even after gastrectomy, but altered pancreatic function is apparent after gastrojejunostomy (BII). Fat loss in the feces is considerably greater after BII resection than after gastroduodenostomy. This loss may indicate insufficient digestion of food by pancreatic enzymes.
In a recent randomized comparison between patients after BI and RY reconstructions, endoscopic examination revealed that the frequency of bile reflux and degree of inflammation in the remnant stomach were less in the RY group than in the BI group, which is most likely due to the absence of pylorus in the RY group. However, RY reconstructions did not prevent esophagitis and were associated with more initial stasis complications.
Even histologic changes of the stomach mucosa characteristic of chronic atrophic gastritis seem to be present to a lesser degree after a BI resection than after BII. The same is true for the frequency of carcinoma of the stomach remnant.
Cardiac function tests demonstrate similar lower esophageal sphincter pressures in reaction to a test meal before and after gastroduodenostomy. After BII resection, the tonicity of the lower esophageal sphincter decreases, but this functional disturbance of the cardia is rarely of clinical relevance.
Arguments in Favor of Bii Gastrectomy or Ry Reconstruction
The main argument in favor of BII reconstructions is that a larger portion of the stomach can be resected and lymphadenectomy is easier. In all cases in which a BI reconstruction could only be accomplished with tension, one should choose BII. In some cases a BII reconstruction results in early dumping symptoms (see following discussion). Those patients should undergo, if conservative treatment fails, relaparotomy and reconstruction according to RY. The RY offers a better control to avoid enterogastric reflux into the gastric remnant and is the method of choice when early dumping or reflux problems occur.
Gastric Ulcer
The main indication for partial gastric resections is gastric ulcer, and this is usually a recurrent ulcer after adequate antisecretory treatment and eradication of Helicobacter pylori. Partial gastrectomy is the method of choice because
the gastric ulcer is removed in toto during distal resection and can be examined histologically,
the point of least resistance on the antrum–corpus border of the lesser curvature is eliminated,
the number of chief cells is reduced by removal of a part of the fundus,
the antrum as the point for the formation of gastrin is eliminated,
the remainder of the stomach is partly vagotomized by dissection of the lesser curvature above the resection border and the standard reconstruction for partial gastrectomy in gastric ulcer patients is BI.
Prepyloric Ulcer
Prepyloric ulcers represent a good indication for partial gastric resections. Because of its secretory behavior, this ulcer type was, as far as the surgical and therapeutic consequences were concerned, previously included with duodenal ulcers and historically represented an indication for vagotomy only. However, results after 5 years of using this procedure showed relatively high recurrence rates; therefore, it can be concluded that prepyloric ulcers would be better regarded as gastric ulcers as far as surgical treatment is concerned. Partial gastric resections for prepyloric ulcers should, in our view, be combined with selective gastric vagotomy.
Complicated Ulcers
Although elective ulcer surgery has strongly decreased in the decade of potent antisecretory drugs, the frequency of operations for complicated ulcers has remained relatively stable.
The classic indications for partial gastric resections in ulcer surgery are perforation, bleeding, obstruction, and intractability. In addition, gastric “ulcers” may mask or be at risk for the development of gastric adenocarcinoma. Therefore, all gastric ulcers must be biopsied and followed until healing. Giant gastric ulcers (>3 cm) have a 30% incidence of harboring a cancer.
Early Carcinoma and Carcinoma of the Antrum
Partial gastric resections cannot be recommended as a standard treatment of locally advanced gastric cancer because a total gastrectomy with adequate lymphadenectomy is the method of choice. As an exception, in our institution patients with well-differentiated and early (T1/T2 N0) gastric adenocarcinomas undergo subtotal gastric resection, in which four-fifths of the stomach is resected with a standard D2 lymphadenectomy, and a BII or RY reconstruction is done. In the Far East, mucosal cancers of the antrum are common and more frequently resected by partial gastrectomy and BI reconstruction. Sentinel lymph node dissection after distal gastrectomy for early gastric cancer has been evaluated with conflicting short-term and open long-term results. Therefore, the general use of this technique for discriminating between partial or total gastrectomy for early gastric cancer cannot yet be recommended.
Gastroduodenostomy with Anastomosis to the Side of the Greater Curvature of the Stomach
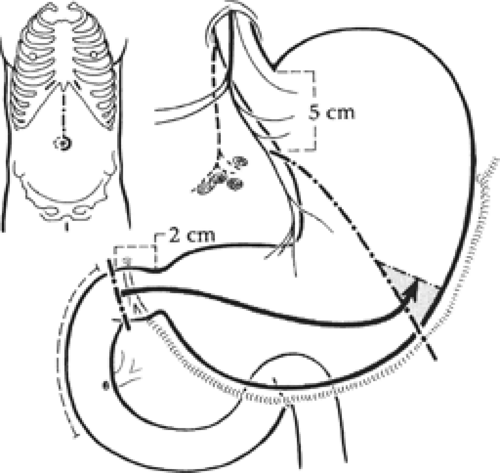
As a rule, midline epigastric incision is the best approach (Fig. 2). Alternatively, a transverse epigastric rectus muscle-cutting incision or an upper vertical muscle-splitting incision to the right can be made.
The dissection of the stomach begins at the middle of the greater curvature by incision of the gastrocolic ligament. Thus, the omental bursa is opened. The dissection for gastric ulcers can be done between the gastroepiploic vessels and the gastric wall. In carcinoma, the greater omentum corresponding to the extent of the resection of the greater curvature must be removed at the same time. When the omental bursa has been opened, the flimsy part of the gastrohepatic omentum may be pierced by the
finger, and a soft rubber Penrose drain can be placed around the stomach. The dissection is then continued step-by-step along the greater curvature toward the duodenum. Near the pylorus, the greater curvature of the omentum becomes thick and divides into a front and back layer. The dissection should be continued bluntly in the loose intermediate tissue in the direction of the duodenum; the layers of tissue carrying the vessels should then be ligated individually.
finger, and a soft rubber Penrose drain can be placed around the stomach. The dissection is then continued step-by-step along the greater curvature toward the duodenum. Near the pylorus, the greater curvature of the omentum becomes thick and divides into a front and back layer. The dissection should be continued bluntly in the loose intermediate tissue in the direction of the duodenum; the layers of tissue carrying the vessels should then be ligated individually.
The preparation of the duodenum begins above or just below the second portion of the duodenum from a lateral direction, the so-called Kocher maneuver. The peritoneal reflection is sharply cut along the lateral duodenal wall between the second portion of the duodenum and the beginning of the hepatoduodenal ligament. By putting traction on the second portion of the duodenum medially, the retroperitoneal tissue is loosened (part bluntly, part sharply) until the duodenum is mobilized. In this way, a good general exposure can be achieved; this important maneuver facilitates the subsequent gastroduodenostomy. The preparation of the free first part of the duodenum is then continued.
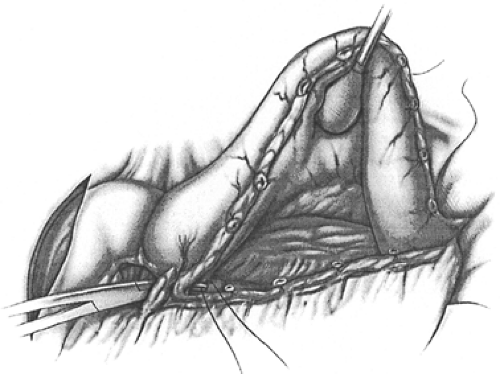
By stretching the stomach, the dissection proceeds along the greater curvature toward the left medial duodenal wall, then toward the back wall, and finally toward the lateral duodenal wall as far as the beginning of the hepatoduodenal ligament. In this way, 3 to 5 cm of the back wall of the duodenum can be exposed, usually without technical difficulty. The transition from the free first part of the duodenum to the part fixed dorsally on the pancreas can be recognized from the course of the gastroduodenal artery (Fig. 3). At this point, the serosa reaches from the duodenum to the head of the pancreas. The surgeon must be especially careful here because the artery is important for the blood supply to the duodenum and the pancreas.
After mobilization of the duodenum, the dissection is continued along the lesser curvature of the stomach. The right gastric artery is divided between clamps and ligated (Fig. 4). Difficulties may arise as a result of penetration of a gastric ulcer. Frequently, a penetrating gastric ulcer can be pinched free of underlying tissue by finger pressure.
We recommend addition of a selective vagotomy of the gastric remnant only for benign ulcer surgery in which gastric hypersecretion is assumed as one of the main pathogenetic factors, that is, in cases with multiple ulcers or prepyloric ulcers. In these rare cases we carefully divide the vagal branches of the anterior and posterior vagus that lead to the gastric remnant and leave the hepatic vagal branches intact.
In every case, the dissection must leave an adequate portion of intact stomach wall for subsequent anastomosis with the duodenum. According to the localization of the ulcer, the dissection of the stomach along the lesser curvature can be continued to the proximal resection line. The layers of the gastrohepatic omentum rest at varying intervals on the front or back wall of the stomach. These layers encompass a tissue rich in fat within which the branches of the left gastric artery and vagal branches are found. The dissection proceeds by bluntly forcing
the intermediate tissue apart and individually severing the front and back layer of the gastrohepatic omentum. As long as the ascending trunk of the left gastric artery is not directly involved, it should remain intact during the resection.
the intermediate tissue apart and individually severing the front and back layer of the gastrohepatic omentum. As long as the ascending trunk of the left gastric artery is not directly involved, it should remain intact during the resection.
The actual resection starts with the cutting of the duodenum between holding or guy sutures. The duodenum is temporarily closed with a sponge; the resection borders of the stomach are then determined.
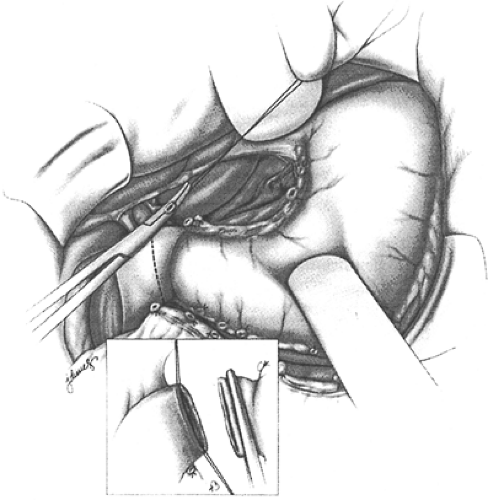
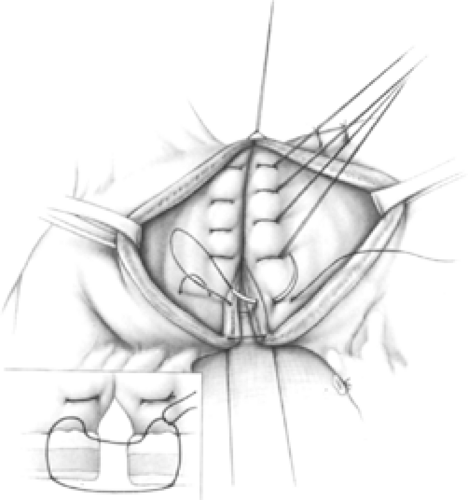
A sewing instrument (e.g., stapler, TA-90 (Covidien) or TL90 (Ethicon)) facilitates the final step of stomach removal. The incision follows at an angle of 45 degrees to the lesser curvature (Fig. 2). The staple line can, but need not, be oversewn (Fig. 5). After removal of the distal portion of the stomach, a clamp is fitted at right angles to the greater curvature. The clamp is thus pushed far enough orally for the removal level to correspond in size to the duodenal lumen. The remaining aboral end is cut off after stay sutures are placed at each cut edge (Fig. 5). It is recommended that the so-called von Haberer submucosal sutures (4-0 polyglycolic acid) be used in the front and back walls to achieve hemostasis. The anastomosis should be performed without clamps.
The end-to-end gastroduodenostomy is accomplished by anastomosing the duodenum to the end of the greater curvature. For this purpose, the two cut surfaces are placed adjacent to each other and two corner
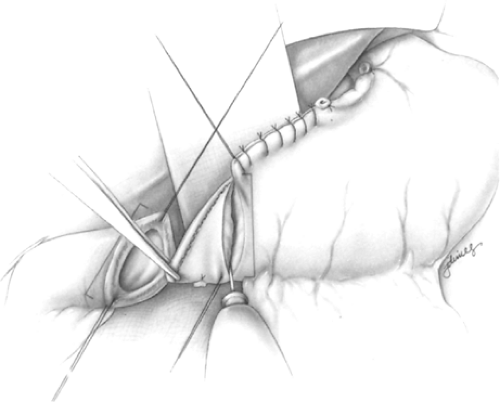
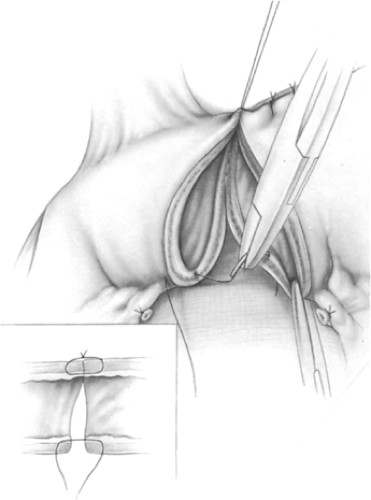
stitches are placed, starting at the stomach through the seromuscular layers with tangential grasping of the mucosa. At the duodenum, this stitch is done from inside to outside. The corner suture at the lesser curvature is tied, whereas the suture on the opposite side is left open (Fig. 6). The back wall is reconstructed by interrupted back stitches (3-0 polyglycolic acid). These stitches start through all layers of the back wall at the cut edge of the lesser curvature from inside to outside and go through all layers of the posterior wall of the duodenum from outside to inside. The suture is led back grasping only the mucosa, first of the duodenum and then of the stomach (Fig. 7). Knotting these sutures leads to an exact coaptation, especially at the level of the mucosa (Fig. 7, inset). The front wall is best closed with one row of interrupted sutures through all layers with tangential stitches of the mucosa with the same technique as the corner stitches (Fig. 8). Special attention must be paid to the so-called Jammerecke (angle of sorrow) on the lesser curvature (Fig. 9). It is advisable to use the triple seromuscular structure, which includes the duodenal walls as well as the front and back wall of the stomach. Another alternative is shown in Figure 10.
stitches are placed, starting at the stomach through the seromuscular layers with tangential grasping of the mucosa. At the duodenum, this stitch is done from inside to outside. The corner suture at the lesser curvature is tied, whereas the suture on the opposite side is left open (Fig. 6). The back wall is reconstructed by interrupted back stitches (3-0 polyglycolic acid). These stitches start through all layers of the back wall at the cut edge of the lesser curvature from inside to outside and go through all layers of the posterior wall of the duodenum from outside to inside. The suture is led back grasping only the mucosa, first of the duodenum and then of the stomach (Fig. 7). Knotting these sutures leads to an exact coaptation, especially at the level of the mucosa (Fig. 7, inset). The front wall is best closed with one row of interrupted sutures through all layers with tangential stitches of the mucosa with the same technique as the corner stitches (Fig. 8). Special attention must be paid to the so-called Jammerecke (angle of sorrow) on the lesser curvature (Fig. 9). It is advisable to use the triple seromuscular structure, which includes the duodenal walls as well as the front and back wall of the stomach. Another alternative is shown in Figure 10.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree