Digestive System
Guanghua Wang
▪ Questions and Answers
1. A segment of esophagus lined by columnar epithelium:
a. May be an incidental finding with NO clinical significance
b. Changes to stratified squamous epithelium by 25 weeks of gestation
c. May indicate Barrett esophagus
d. May indicate heterotopic gastric mucosa
e. All of the above
View Answer
1. e. Esophageal mucosa lined by columnar epithelium changes to stratified squamous epithelium by 25 weeks of gestation, and patches may persist in early infancy without any clinical significance. It has to be differentiated from ectopic gastric mucosa, which also shows glandular layer beneath the surface epithelium. Barrett esophagus is a possibility but requires demonstration of the presence of goblet cells and positive endoscopic findings.
2. Normal findings in the lower esophagus and gastroesophageal junction include all of the following EXCEPT:
a. The basal layer of the distal esophagus thicker than the rest of esophagus
b. Abrupt transition between squamous mucosa and oxyntic mucosa
c. Glycogenated squamous mucosa above the Z-line
d. Squamous mucosa with submucosal mucous glands
e. The presence of goblet cells
View Answer
2. e. The presence of goblet cells is not a normal finding in esophagus and may indicate Barrett esophagus. Cardiac mucosa may be found in the gastroesophageal junction and may have mild glandular distortion. Cardiac mucosa, however, is not normally found in children and in up to 30% of the adult population.
3. All of these statements are correct about esophagus EXCEPT:
a. Esophagus length in adults varies with the height of the individual and ranges from 25 to 30 cm.
b. Esophageal mucosa has three components: squamous epithelium, muscularis mucosae, and the lamina propria.
c. It may be normal to find glands similar to those of the gastric cardia in the lamina propria of the distal esophagus.
d. Submucosal mucous gland complexes in the esophagus are most prominent at the upper and lower ends of the esophagus.
e. Heterotopic gastric mucosa known as the “inlet patch” often results in peptic ulcer or carcinoma.
View Answer
3. e. In most instances, the esophageal heterotopic mucosa is benign; it rarely results in peptic ulceration or carcinoma. The distance of the esophagogastric junction from the teeth averages 40 cm in adults.
4. A mediastinal cyst lined by columnar mucosa is a/an:
a. Bronchogenic cyst
b. Enterogenous cyst
c. Gastrointestinal duplication
d. Thymic cyst
e. All of the above
View Answer
4. e. All of these cysts can be lined by columnar mucosa. Bronchogenic cyst should have, in addition, cartilage and respiratory glands. The enterogenous cysts are lined by glandular mucosa without muscle coat. Gastrointestinal duplications have smooth muscle coat in addition to an alimentary mucosal lining. Thymic cyst can be located in the mediastinum or neck, and lymphoid tissue in the wall of thymic cyst is mainly of thymic origin and usually includes Hassall corpuscles.
5. Failure of the tracheal bud to develop normally from the primitive foregut during embryonic life results most commonly in:
a. Esophageal web
b. Tracheomalacia
c. Esophageal atresia with tracheoesophageal fistula
d. Duodenal atresia
e. Zenker diverticulum
View Answer
5. c. Esophageal atresia occurs approximately 1 in 4000 live births, and it usually occurs together with tracheoesophageal fistula. Sometimes, a baby has atresia without fistula. The upper esophagus ends blindly, and there is a fistula between the lower portion of the esophagus and trachea.
6. A 25-year-old man complains of epigastric abdominal pain. Which of the following statements about his biopsy shown in Figure 6.1 is NOT true?
a. This disease is a frequent reason to be referred to a gastroenterologist.
b. Patients with this disease often have decreased esophageal sphincter pressure.
c. The presence of intraepithelial neutrophils indicates severe disease.
d. It is often associated with hiatus hernia.
e. The presence of eosinophils in squamous mucosa is a specific histological feature for the diagnosis.
View Answer
6. e. Reflux esophagitis is caused by retrograde flow of gastric and, sometimes duodenal contents into the esophagus. It is histologically characterized by intraepithelial eosinophils, increased intraepithelial lymphocytes, basal cell hyperplasia, and elongated papillae. The presence of neutrophils reflects the acute erosive or ulcerative esophagitis. Infectious esophagitis and esophagitis caused by ingestion of caustic substances have to be excluded before the diagnosis of reflux esophagitis is made. Intraepithelial eosinophils are important for the diagnosis but can also be found in other diseases, such as allergic esophagitis.
7. All of the following about Barrett esophagus are correct EXCEPT:
a. Barrett dysplasia is defined as a neoplastic change of the epithelium confined to the basement membrane of the glands with no evidence of invasion.
b. High-grade dysplasia in a biopsy with Barrett esophagus indicates there is about 70% chance that carcinoma is already present.
c. The metaplastic Barrett esophagus epithelium can be complete intestinal metaplasia or incomplete intestinal metaplasia.
d. Incomplete intestinal metaplasia may be more prone to enter the dysplasia-carcinoma sequence than complete intestinal metaplasia.
e. Grading dysplasia in Barrett esophagus is based solely on cytologic features.
View Answer
7. e. Four mucosal features are needed to grade dysplasia in Barrett esophagus, including: surface maturation, glandular architecture, cytologic features, and inflammation around mucosa.
8. The diagnosis of Barrett esophagus is made through:
a. Barium swallow findings in a patient with a history of esophageal reflux disease
b. Characteristic endoscopic findings, and biopsy showing histology of esophageal reflux disease
c. Characteristic histologic findings of Barrett esophagus, such as goblet cells, present in the esophageal biopsy
d. Characteristic endoscopic findings of Barrett esophagus and evidence of intestinal metaplasia by biopsy
e. Characteristic endoscopic findings of Barrett esophagus and findings of dysplastic esophageal mucosa in biopsy
View Answer
8. d. According to the American College of Gastroenterology, to make the diagnosis of Barrett esophagus, pathologists need to have both evidence of intestinal metaplasia in biopsy and positive endoscopic findings are needed.
9. This esophageal biopsy (Fig. 6.2) was taken from a white male with a history of reflux esophagitis. He presented with dysphagia and esophageal mass. Genetic alterations implicated in the causation of this lesion include:
a. P53 mutations
b. Myc amplification
c. Microsatellite instability
d. K-ras mutations
e. All of the above
View Answer
9. e. The section shows glandular mucosa with intestinal metaplasia and glandular fullness and complexity of carcinoma in situ. These features are those of Barrett esophagus with high-grade dysplasia. All listed genetic alterations were suggested to be involved in the Barrett esophagus-dysplasia-adenocarcinoma sequence. In addition, EGFR, beta-catenins, erbB2, MCC, and DCC genes are also involved in this sequence.
10. The most common cause of infectious esophagitis in AIDS patients is:
a. Bacterial esophagitis
b. Herpes simplex esophagitis
c. Cytomegalovirus (CMV) esophagitis
d. Candida esophagitis
e. Allergic esophagitis
View Answer
10. d. Candida esophagitis causes most esophageal diseases in AIDS patients followed by CMV and herpesvirus infection. Candida esophagitis can also occur in other immunosuppressive disorders, diabetes and antibiotic therapy and may occasionally occur in immunocompetent individuals. Bacterial esophagitis is unusual and generally occurs in patients with granulocytopenia.
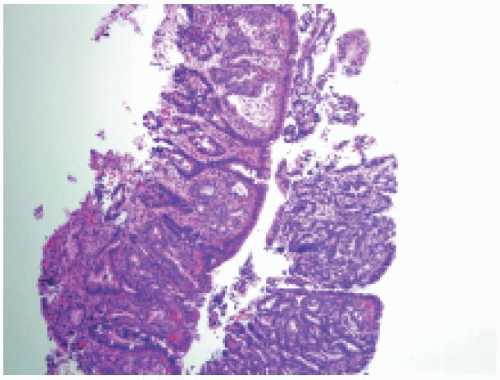
11. This esophageal biopsy (Fig. 6.3) was taken from a 35-year-old man with intermittent dysphagia with food
impaction. Endoscopy showed multiple esophageal rings. Which of the following statements about this lesion is NOT true?
impaction. Endoscopy showed multiple esophageal rings. Which of the following statements about this lesion is NOT true?
a. The esophagus normally does NOT contain any eosinophils; their identification in esophageal biopsy represents a pathologic change.
b. The cause of this lesion is most likely associated with parasite infection.
c. The lesion is characterized by a prominent intraepithelial eosinophilic infiltrate.
d. The differential diagnosis in esophageal biopsy with eosinophils infiltrate includes reflux esophagitis, parasitic infection, drug reactions, or eosinophilic esophagitis.
e. Eosinophilic infiltrate in eosinophilic esophagitis is present in all parts of esophagus, while in reflux esophagitis, eosinophilic infiltrate is mainly found distally and taper proximally.
View Answer
11. b. The figure exhibits features of eosinophilic esophagitis. The food allergy is a common cause of eosinophilic esophagitis. Most affected patients have clinical evidence of food and airborne allergen hypersensitivity. Many patients have a history of atopic disease. In contrast, parasitic infection is not a common cause of this disease
12. The best test to define esophageal reflux is based on:
a. Clinical symptoms of heartburn, regurgitation, and dysphagia
b. Characteristic appearance on upper GI endoscopy
c. Biopsy changes showing infiltration by eosinophils
d. Ambulatory pH monitoring
e. Response to medications
View Answer
12. d. pH dropping to less than 4 is a strong indication of reflux. Biopsy changes are not specific, and similar histology can occur in allergic esophagitis.
13. Which of the following statements is true about this esophageal mass (Fig. 6.4)?
a. This type of lesion is more common in women than in men.
b. When associated with Barrett esophagus, it has a better prognosis than when not associated with Barrett esophagus.
c. It is three times more common in Barrett esophagus than in the general population.
d. It is more common in whites than in blacks.
e. It is the most common esophageal cancer.
View Answer
13. d. Adenocarcinoma of the esophagus is more common in white men and represents only 5%-10% of all esophageal cancers. Associated Barrett esophagus increases the risk of developing adenocarcinoma by 30-40 folds and worsens the prognosis of these tumors.
14. Which of the following is NOT considered as a risk factor in general for the development of squamous cell carcinoma of the esophagus?
a. p53 gene mutations
b. HPV infection
c. Smoking
d. Heavy consumption of alcohol
e. APC gene mutations
View Answer
14. e. Esophageal squamous cell carcinoma develops as the result of a sequence of changes that include esophagitis, atrophy, mild to severe dysplasia, carcinoma in situ and finally, invasive cancer. Both genetic and environmental factors are involved in the pathogenesis of the esophageal squamous cell carcinoma. This type of cancer also shows great geographical diversity in its incidence. High incidence is noted in Northwest France, Northern Italy, East European countries, Iran, Central China, South Africa and Southern Brazil. In addition to the listed environmental risk factors, other factors include high intake of nitrosamines, thermal injury, and prior radiotherapy. Besides p53 mutation, other genetic alterations that are important in its pathogenesis include: (a) disruption of cell cycle control (inactivation of p16, via homozygous loss or promoter methylation, and amplification of Cyclin D1); (b) activation of oncogenes (FGFR and c-myc gene amplification); and (c) loss of tumor suppressor genes (such as loss of heterozygosity of RB gene). However, there is no convincing evidence that APC gene mutations play a crucial role in the development of esophageal squamous cell carcinoma.
15. Which of the following concerning type of mucins in complete intestinal metaplasia complicating chronic gastritis is true?
a. The predominant mucin type is sialomucin.
b. There is over-expression of MUC-1 mucin.
c. There is over-expression of MUC5AC mucin.
d. There is co-expression of MUC-2 and MUC-6.
e. The predominant mucin type is neutral mucin.
View Answer
15. a. In complete intestinal metaplasia (resembling small intestinal epithelium), the predominant mucin type is sialomucin with expression of MUC-2 and absence of expression of MUC1, MUC5AC, and MUC-6. In incomplete intestinal metaplasia (resembling colonic epithelium), metaplastic cells may secrete, in addition to sialomucins, neutral mucins or sulfomucins. The cells strongly express MUC1, MUC2, MUC5AC5, and MUC6 mucin proteins.
16. Chronic atrophic gastritis caused by Helicobacter pylori is mainly associated with increased incidence of:
a. Diffuse-type gastric carcinoma
b. Intestinal-type adenocarcinoma
c. Squamous carcinoma
d. Hepatic-type adenocarcinoma
e. Carcinoid tumor
View Answer
16. b. It is true that infection with H. pylori is very common; the Centers for Disease Control and Prevention (CDC) estimates that about 20% of persons less than 40 years of age and about 50% of persons over 60 years of age are infected in the United States. However, most infected people do not have symptoms and only a small percentage develop disease. Gastric and duodenal ulcers can be caused by other reasons, but the most common cause is H. pylori infection. H. pylori infection is associated with a 1%-2% lifetime risk of stomach cancer and a less than 1% risk of gastric MALT lymphoma. H. pylori-associated chronic atrophic gastritis is the commonest precursor lesion for intestinal type adenocarcinoma.
17. Mutation in E-cadherin gene or alteration of its gene expression predisposes to:
a. Hereditary diffuse gastric carcinoma
b. Intestinal-type adenocarcinoma
c. Squamous carcinoma
d. Hepatoid-type adenocarcinoma
e. Carcinoid tumor
View Answer
17. a. Germline mutations in the gene coding for E-cadherin leads to an autosomal-dominant predisposition to hereditary diffuse gastric carcinoma.
18. Predisposing lesions for the development of gastric carcinoma include which of the following?
a. Gastritis and intestinal metaplasia
b. Gastric Ulcer
c. Hyperplastic polyp
d. Adenoma
e. All of the above
View Answer
18. e. Gastric carcinoma does not arise de novo from a normal mucosa. Chronic atrophic gastritis and intestinal metaplasia commonly precede and or accompany intestinal type adenocarcinoma. H. pylori associated gastritis is the commonest gastric precursor lesion to gastric carcinoma. Since gastric ulcer and gastric carcinoma share similar risk factors, patients with gastric ulcer are at greatly increased risk of developing gastric carcinoma. Gastric adenomas have a different frequency of malignant transformation, which depends on their size and histological grade. Gastric carcinoma may develop from gastric hyperplastic polyps with intestinal metaplasia and or dysplasia.
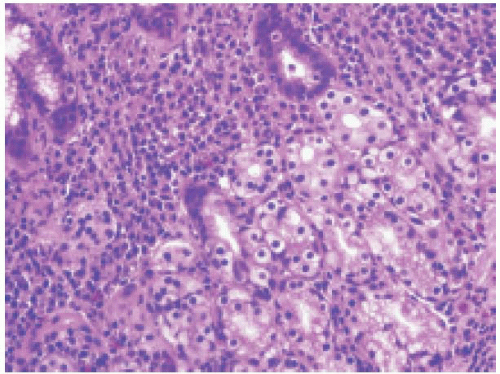
19. This gastric biopsy (Fig. 6.5) was from a 63-year-old woman with a history of chronic atrophic gastritis. All of the following statements are true about this lesion EXCEPT:
a. This type of lesion usually arises from Enterochromaffin-like (ECL) cells of the stomach.
b. Chronic atrophic gastritis is a predisposing factor.
d. This lesion occurs in association with multiple endocrine neoplasia type 2 (MEN2).
e. Mutation and/or loss of heterozygosity (LOH) at the MEN1 locus is associated with the development of this lesion.
View Answer
19. d. The section shows gastric lamina propria with small nests and gland-like lesion. The higher magnification (picture not shown) showed that tumor cells have uniform nuclei, diffuse chromatin and inconspicuous nucleoli. These features are those of carcinoid tumor. The formation of glands in gastric carcinoid tumor like this case can mimic adenocarcinoma. Five types of gastric carcinoid tumors are recognized, including ECL (enterochromaffin-like) cell tumor associated with type A chronic atrophic gastritis, ECL cell tumor with combined MEN-1 and Zollinger-Ellison syndrome, sporadic ECL tumor, Non-ECL tumors, and ECL cell tumor with achlorhydria and parietal cell hyperplasia. Hypergastrinemia, autoimmune chronic atrophic gastritis, MEN type 1, and Zollinger-Ellison syndrome are all predisposing factors for the development of gastric carcinoid tumor. There is no evidence that carcinoid tumor is associated with MEN type II.
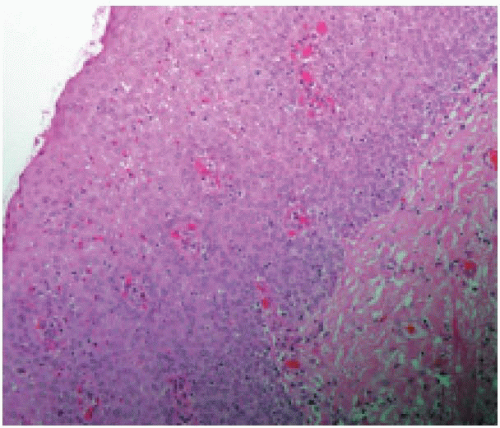
20. This section (Fig. 6.6) was taken from the stomach fundus. In addition to features of chronic gastritis, there is proliferation of cells that measure less than 0.5 mm and are positive for chromogranin immunostain (stain not shown). What is the best designation for this entity?
a. Carcinoid
b. Neuroendocrine carcinoma
c. Neuroendocrine cell hyperplasia
d. Gastrinoma
e. Early carcinoid
View Answer
20. c. If the collection of neuroendocrine cells is less than 0.5mm, it is best classified as neuroendocrine cells hyperplasia. The term “carcinoid” is usually applied to collection of neuroendocrine cells measuring more than 0.5 mm.
21. All following statements are true concerning gastrointestinal stromal tumor (GIST) EXCEPT:
a. Most GISTs are sporadic, affecting individuals in age group of 50-60 years, and have a slight male predominance.
b. The type or location of mutation in C-kit may determine the patient’s prognosis and treatment response.
c. PDGFR-α mutations are significantly associated with higher frequency of epithelioid or mixed morphology GIST tumors and impart a favorable prognosis.
d. Gastrointestinal autonomic nerve tumor (GANT) is a variant of GIST and often stains positively for neuron-specific enolase (NSE), S-100, synaptophysin, chromogranin, and neurofilament protein.
e. Tumors larger than 10 cm, with no detectable mitotic activity do not recur or metastasize.
View Answer
21. e. Gastrointestinal stromal tumors (GIST) are found mostly in the stomach and can be benign or malignant depending on the size and the mitotic rate. Tumors larger than 10 cm can recur and metastasize regardless of the mitotic rate. GANT tumors represent a GIST variant that have ultrastructural features of autonomic neurons, including cell processes with neurosecretory type dense core granules and arrays of microtubules.
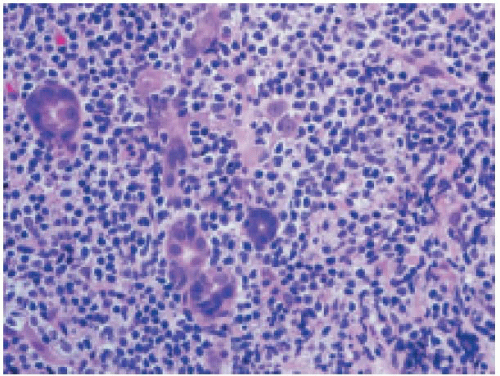
22. A 45-year-old man presented with a gastric mass. Histology of the lesion is shown (Fig. 6.7). Immunostains show that neoplastic lymphoid cells are positive for CD20, CD43, and bcl-2 and are negative for CD3, CD5, and CD10. Which of the following is NOT true of this lesion?
a. t(11;18) API2/MALT1, t(14;18)/IGH-MALT1, t(1;14)/IGH-BCL-10, and t(3;14)/IGH-FOXP1 translocations can all be found in this lesion.
b. 60%-70% of patients with this lesion have t(11;18) API2/MALT1 translocation.
c. It is associated with H. pylori infection.
d. Patients with this lesion and t(11;18)(q21;q21) translocation do not respond to antibiotics treatment for H. pylori eradication.
e. t(11;18) API2/MALT1 translocation is usually negative in gastric large B-cell lymphoma arising from this type of lesion.
View Answer
22. b. t(11;18) API2/MALT1, t(14;18)/IGH-MALT1, t(1;14)/IGH-BCL-10, and t(3;14)/IGH-FOXP1 translocations are all associated with mucosa-associated lymphoid tissue (MALT) lymphoma. Only t(11;18) API2/MALT1 translocation is specifically associated with MALT lymphoma. Detection rate of t(11;18) API2/MALT1 translocation varies with different organ sites, but is only found in about 25%-30% of gastric MALT lymphomas.
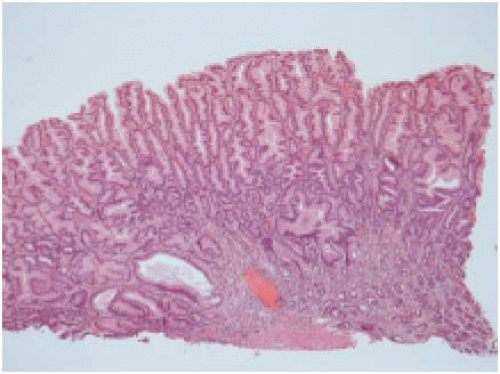
23. This gastric biopsy (Fig. 6.8) was from a 45-year-old man with symptoms of epigastric pain, anorexia, weight loss, and peripheral edema. Which of the following is NOT part of the clinicopathologic features described in this lesion?
a. Clustered incidence in adult and middle-age men
c. Atrophy of oxyntic glands
d. Prominent chronic inflammatory cell infiltrate
e. Mucosal cysts
View Answer
23. d. The clinical presentation and histologic features are those of Ménétrier disease. Inflammation is usually minimal in Ménétrier disease. This disease is rare and usually occurs in men between 30-60 years of age. The disease is characterized by giant gastric folds. Large gastric folds are also found in Zollinger-Ellison syndrome, peptic ulcer, Crohn disease, eosinophilic gastritis, and gastric lymphoma. So, the presence of foveolar cell hyperplasia alone, which creates large gastric folds, is not sufficient to make a diagnosis of Ménétrier disease.
24. All following statements are true about gastric polyps EXCEPT:
a. The majority of gastric polyps is nonneoplastic.
b. Fundic gland polyps and hyperplastic polyps are two most common types of gastric polyps.
c. Fundic gland polyp can occur sporadically or in the setting of familial adenomatous polyposis (FAP), and it can develop after a prolonged use of proton pump inhibitors.
d. Most hyperplastic polyps develop on a background of chronic gastritis.
e. Inflammotory fibroid polyps are most commonly found in children.
View Answer
24. e. About 80%-90% of gastric polyps are nonneoplastic. Different genetic alterations are involved in pathogenesis of fundic gland polyp formation. Sporadic fundic gland polyps contain activating mutations of the β-catenin gene while fundic gland polyps in the setting of FAP contain APC gene mutations. Histologically fundic gland polyps show hyperplastic expansions of oxyntic mucosa with cystic dilatation. Most hyperplastic polyps develop on a background of chronic gastritis. Histologically, they exhibit foveolar hyperplasia with edematous stroma infiltrated with plasma cells, lymphocytes, eosinophils, mast cells, and neutrophils. Some hyperplastic polyps contain epithelial dysplasia that may have a potential for a malignant transformation. Inflammatory fibroid polyps occur mainly in adults and in general are considered as reactive in nature. Histologically, they are consisted of spindled fibroblast-like cells with inflammatory cells and abundant small blood vessels formed in the submucosa. Generally, they do not have epithelial proliferation.
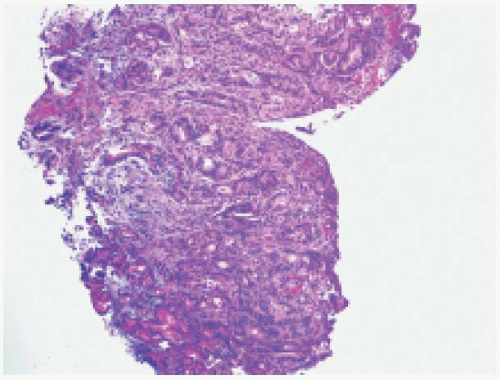
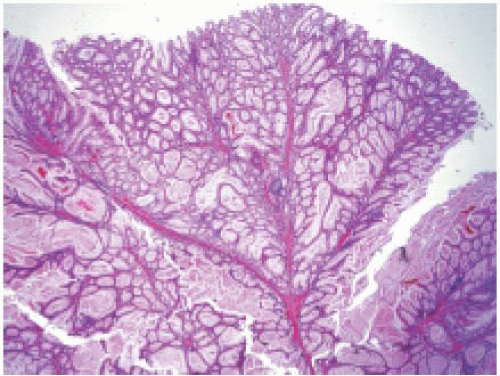
25. This section (Fig. 6.9) was taken from a 22-year-old man who was found to have multiple small intestinal polyps. All sections show similar histologic features as demonstrated in this image. Which of the following genes is involved in its pathogenesis?
a. APC gene
c. STK11
d. SMAD4
e. PTEN
View Answer
25. c. The section shows a polyp with an infrastructure of arborizing smooth muscle dividing the nondysplastic glands into lobules, which is the characteristic histologic feature of hamartomatous polyp, Peutz-Jeghers type. Peutz-Jeghers syndrome is an inherited cancer syndrome with autosomal dominant trait. Mucocutaneous melanin pigmentation and hamartomatous intestinal polyposis are characteristic features. It is associated with gene SKT11 (Serine/Threonine protein kinase), with nearly complete penetrance.
26. A 55-year-old male presents with abdominal pain, dysphagia, and gastrointestinal bleeding and abdominal mass. The histology of lesion is shown (Fig. 6.10). Neoplastic cells are positive for CD117, CD34, and S-100. This lesion may be associated with all of the following EXCEPT:
a. Mutations in PDGFRA or C-KIT genes
b. Ultrastructural features of neuronal cell processes
c. Neurofibromatosis type I
d. Extra-adrenal paraganglioma
e. Familial trait in majority of cases
View Answer
26. e. This patient has a gastrointestinal stromal tumor (GIST). Constitutive activating mutations in C-KIT or PDGFRA genes can be found in approximately 85% and 4%-18% of GISTs, respectively. Approximately 12% of GISTs does not have C-KIT or PDGFRA mutation. In addition to mutations in C-KIT and PDGFRA genes, GIST is commonly associated with losses in chromosomes 14 and 22. Rare GIST tumors that show ultrastructural evidence of neuronal cell processes are termed gastrointestinal nerve tumors. Some GISTs occur in patients with neurofibromatosis type 1 or Carney triad (which includes GIST, pulmonary chondroma, and functioning extra-adrenal paraganglioma). GISTs in the setting of neurofibromatosis type I generally lack C-KIT or PDGFRA mutations. The mutation responsible for Carney triad is not yet identified. Familial or autosomal dominant form of GIST can occur but is rare, which develop due to germline activating mutations in C-KIT or PDGFRA gene.
27. Which of the following statements is true about infantile hypertrophic pyloric stenosis HPS?
a. It is more common in female children
b. It is seen in 1 in 20,000 infants
c. It has no recognizable pattern of inheritance
d. Majority of patients present at birth with abdominal mass
e. The outer longitudinal muscle fibers are hyperplastic and hypertrophic
View Answer
27. c. It is true that there is no recognizable pattern of inheritance for this identity. HPS is more common in boys with a male to female ratio of approximately 4:1. The incidence is approximately 1 in 200 to 400 of live births. Majority of patients with HPS are asymptomatic till the first few weeks of life. Histologically, hyperplasia and hypertrophy of inner circular muscle fibers are the main histological features and, in contrast, the outer longitudinal muscle fibers appear to be unremarkable.
28. Duodenal atresia is a feature of patients with:
a. Cystic fibrosis
b. Total colonic aganglionosis
c. Turner syndrome
d. Down syndrome
e. Absent pancreas
View Answer
28. d. Duodenal atresia is associated with Down syndrome, not cystic fibrosis. Approximately 20%-40% of all infants with duodenal atresia have Down syndrome. Approximately 8% of all infants with Down syndrome have duodenal atresia. Cystic fibrosis is however associated with jejunoileal atresia.
29. This is a duodenal biopsy (Fig. 6.11) from a 25-year-old woman with a history of chronic diarrhea and anemia. The patient has a positive serologic test for transglutaminase antibody . Which of the following immunostains will be positive in the majority intraepithelial lymphocytes?
a. CD20
c. CD4
d. Anti-gliadin antibody
e. T-cell intracytoplasmic antigen (TIA-1)
View Answer
29. b. The image exhibits a typical histologic feature of Celiac disease. Celiac disease is characterized by a marked intolerance to dietary gliadin. Intraepithelial lymphocytosis with villous atrophy and crypt hyperplasia are the main histological features of Celiac disease. A large infiltrate of CD8+ T-lymphocytes is usually found in the epithelium, while CD4+ T-lymphocytes infiltrate the lamina propria. The extensive infiltration of the small intestinal epithelium by CD8+ T cells of unknown Ag specificity is one of the diagnostic hallmarks of Celiac disease.
30. Lymphoid depletion in the intestinal lamina propria is seen in patients with:
a. Common variable immunodeficiency
b. IgA deficiency
c. Nezelof Syndrome
d. Severe combined immunodeficiency (SCID)
e. Adenoviral infection
View Answer
30. d. Severe combined immunodeficiency (SCID) represents a constellation of genetically distinct syndrome. They all have defects in both humoral and cellmedicated immune responses and have different inheritance patterns. SCID caused by mutation in the common gamma chain (γc) is inherited in an X-linked recessive pattern. Histologically, intestinal lamina propria is devoid of lymphocytes and plasma cells in SCID patients. Instead, there are many vacuolated PAS-positive macrophages in the lamina propria. Lymphoid hyperplasia can be seen in IgA deficiency, common variable immunodeficiency, and adenoviral infection. Plasma cells are absent in common variable immunodeficiency. Nezelof syndrome (a form of thymic dysplasia) is an autosomal recessive congenital immunodeficiency condition due to underdevelopment of the thymus (but some children may exhibit an X-linked mode of inheritance). In general, lymphoid tissue is hypoplastic in Nezelof syndrome. However, GI biopsies generally show increased numbers of plasma cells and neutrophils in lamina propria.
31. Microscopic colitis is typically seen in patients with:
a. Chronic watery diarrhea
b. Nodular mucosa on colon endoscopy
c. Male gender
d. Bloody diarrhea
e. Laxative abuse
View Answer
31. a. Collagenous colitis and lymphocytic colitis are referred to collectively as microscopic colitis. Patients with microscopic colitis are usually women who present with chronic watery diarrhea and have normal appearing mucosa on endoscopy. Histology usually shows lymphocytic or collagenous colitis.
32. Which of the following statements is true about the difference between Crohn disease and ulcerative colitis?
a. Granulomas are only found in Crohn disease, not in ulcerative colitis.
b. The rectum is not involved in Crohn disease, while it is commonly affected in ulcerative colitis.
c. Crohn disease is not complicated by colorectal carcinoma
d. The ileum is not involved in ulcerative colitis
e. Ulcerative colitis has a higher incidence than Crohn disease
View Answer
32. e. Both Crohn disease and ulcerative colitis are inflammatory bowel disease; they share many features clinically and histologically. Since the course of the diseases and treatments may be different, it is important to differentiate these diseases. Unfortunately, in some cases it may not be possible to differentiate one from the other. Histologic features can be seen in both lesions, although more often in one than other. The presence of focal active colitis, granulomas, and involvement of the upper gastrointestinal tract with skip lesions favor Crohn disease. Ulcerative colitis is generally confined to the colon. The ileum can be involved in ulcerative colitis (backwash ileitis). Ulcerative colitis affects the rectum in 95% of patients, while rectal involvement can occur in up to 50% in Crohn disease. Although ulcerative colitis has higher risk to develop colon cancer than Crohn disease does, patients with Crohn disease still have increased risk to develop intestinal cancer than in the general population. It is true that ulcerative colitis has higher incidence than Crohn disease




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree