2 eggs
¾ c. puffed rice cereal
1 slice white toast
1 Tbsp jelly
2 tsp. soft margarine
½ c. reduced-fat or whole milk
Sugar, pepper (optional)
NO SALT
¼ c. mashed potatoes
½ c. mixed vegetables
1 oz white roll
2 tsp. soft margarine
1 cookie
NO MILK
½ c. vitamin C-fortified apple juice
NO SALT
2 tsp mayonnaise
1 tomato slice
1 c. leafy greens salad
1 Tbsp. vinaigrette
½ c. fruit cocktail canned in heavy syrup
NO MILK
½ c. vitamin C-fortified apple juice
NO SALT
½ c. carrot sticks
1 deli meat sandwich
Carry-Out Meals and Snacks for Dialysis
Patients with renal disease may need to be away during the day for dialysis or other appointments. Sending along an appropriate meal will make their day easier and more comfortable. Perishable foods should be well-chilled and packed in insulated containers with appropriate utensils. Note: regulations at the dialysis unit may limit what is appropriate for that meal’s time frame and convenience (i.e., lunch needs to be consumed after dialysis is over).
The following are suggestions for simple, portable meals:
- Sandwiches on bread, pocket bread or flour tortillas: Meat (roasted beef, pork, poultry) with margarine or mayonnaise or egg salad, chicken/turkey salad, or tuna salad.
- Chef salad and bread: Cubed meat, tuna, and/or egg with lettuce and low potassium raw vegetables; salad dressing, dinner roll, muffin, unsalted crackers, popcorn, or pretzels.
- Low or medium potassium fruit: Small apple, blueberries, grapes, raisins, applesauce, pineapple, or canned, drained fruit such as peaches, pears, fruit cocktail.
- Low or medium potassium raw vegetable: Cucumber slices, green pepper strips, lettuce, broccoli, carrots, cauliflower, celery, radishes, turnips.
- Beverage (regular or sugar-free depending upon diet requirements): Apple juice, grape juice, cranberry juice cocktail, lemonade, punch, carbonated beverages including ginger ale, lemon-lime, and root beer.
*Note: be sure to check for sodium on all canned and bottled beverages
- Snacks: To add calories to a meal or for a midmorning or midafternoon snack: Bagel with cream cheese, graham crackers, unsalted crackers, tortilla chips, unsalted pretzels, rice cakes, vanilla wafers, animal crackers, approved cookies, and sweetened gelatin cup.
- DO NOT SEND: Bologna, cheese, peanut butter, ham, ham salad, banana, melon, fresh orange, dried fruit, tomato, milk, orange juice, grapefruit juice, tomato juice, or cola beverages
Potassium in Foods
Menu modifications can be made using the “higher” and “lower” potassium food lists.
Table 9.2 Potassium (K+) Content in Selected Foods
| Food Category | Foods High in Potassium (≥250 mg K+/Serving) | Foods Lower in Potassium (120–250 mg K+/Serving) Lowest K+ sources are bolded (≤120 mg K+/Serving) |
| Vegetables | Artichoke Asparagus Beans, dried, cooked, (includes baked beans, lentils and limas) Beet greens, cooked Beets Brussels sprouts Collards, cooked Kale Kohlrabi Parsnips Potato, baked, boiled or prepared from frozen Potato, mashed, from homemade Spinach, cooked Pumpkin, canned Salsa Squash, winter, cooked Sweet potato, cooked Swiss chard, cooked Tomato (whole, juice or sauce) Vegetable juice | Bamboo Shoots Bean sprouts Beets, canned, drained Broccoli Cabbage Carrots Cauliflower Celery Corn Cucumber, peeled Eggplant Green Beans Green/Red Peppers Lettuce, iceberg Mixed Vegetables, canned or frozen Mushrooms, ¼ cup Mustard greens, cooked Okra Onions Peas Potatoes, mashed, made with water, boxed flakes or granules Radishes Spinach, fresh Turnips Turnip Greens, cooked Water Chestnuts Wax (Yellow) Beans Zucchini/Summer Squash |
| Fruits | Avocado Banana Cantaloupe Dried fruit, raisins Honeydew melon Kiwifruit Mango Nectarine Orange (fruit and juice) Papaya Pomegranate Prunes (fruit and juice) | Apple (including juice) Applesauce Apricots Blackberries Blueberries Cherries Cranberries (juice and all forms) Fruit Cocktail Grapes (including juice) Grapefruit, ½ medium Peaches, raw and canned Pear, raw Pears, canned Pineapple (including juice) Plums, raw and canned Raspberries Strawberries Tangerines (Mandarin Oranges) Tropical Fruit Mix, canned Watermelon |
| Dairy Products | Milk, fresh or canned Yogurt | Cottage cheese |
| Protein Foods | Dried beans and peas such as pork and beans, refried beans, split peas, kidney beans, lentils. Soybeans, cooked | Peanut butter, 1 tbsp |
| Others | Salt substitutes (containing potassium chloride) Low sodium broth and bouillon (may contain potassium chloride; check nutrient analysis before using) | 2 Tbsp. Ketchup, chili sauce, taco sauce or salsa. |
*Unless otherwise noted, portions are ½ cup or, if whole, 1 medium piece.
Nutrient values from (11) Agricultural Research Service (ARS) Nutrient Database for Standard Reference, Release 22. For a comprehensive list of selected foods containing potassium, refer to website http://www.nal.usda.gov/fnic/foodcomp/search/.
Phosphorus in Foods
Menu modifications can be made using the phosphorus substitutions listed in Table 9.4. It is important to note that too much emphasis on dietary phosphorus restriction means less protein and nutrient intake for persons on dialysis. It is best to treat patients with phosphate binders before unnecessary restriction of phosphorus.
Table 9.3 High Phosphorus Foods
| Food Category | Foods High in Phosphorus |
| Vegetables | Lima beans, cooked legumes (dry beans and peas) |
| Fruits | None |
| Grains | Whole wheat bread, corn tortillas, corn bread, whole wheat bread, biscuits, brown rice, pancakes, waffles, muffins. Cereals made with bran or whole grains (shredded wheat, oats) |
| Dairy Products | Milk, cheese, pudding, yogurt, cottage cheese Eggnog |
| Protein Foods | Beef, pork, lamb, veal, poultry, fish, eggs Legumes (dry beans and peas) such as pork and beans, refried beans, split peas, kidney beans Nuts and seeds, peanut butter Soybeans, tofu |
| Oils, Solid Fats | None |
| Added Sugars | Desserts containing >1 oz chocolate Cake doughnuts Ice cream Cream pies |
| Others | Breads and desserts made with baking powder |
Nutrient values from (11) Agricultural Research Service (ARS) Nutrient Database for Standard Reference, Release 22. For a comprehensive list of selected foods containing phosphorus, refer to website http://www.nal.usda.gov/fnic/foodcomp/search/.
Table 9.4 Phosphorus Substitutions
| Instead of: | Replace with: |
| Milk | Half and half cream (½ c. on cereal) or nondairy creamer |
| Hard cheese | Cream cheese |
| Ice cream | Sherbet, sorbet |
| Baked beans, lima beans | Mixed vegetables or green beans |
| Nuts or seeds | Unsalted popcorn and pretzels |
| Peanut butter (2 Tbsp serving) | Limit to 1 Tbsp. with jelly |
| Chocolate | Graham crackers, animal crackers, hard or jellied candy |
| Whole grain bread | White or rye bread, enriched |
| Whole grain cereals | Rice or corn cereal |
| Cola and pepper-type carbonated drinks, beer or bottled beverages with added phosphoric acid | Root beer, orange, lemon-lime, ginger ale, coffee, tea |
Emergency Dialysis Diet
Emergencies such as snowstorms, floods, or illness may cause someone to miss a scheduled dialysis treatment. The guidelines in Table 9.5 can help prevent complications.
Table 9.5 Emergency Dialysis Diet
Adapted from Mary Greeley Medical Center, Dialysis Center patient education information “Iowa Snowstorm Diet” by Debra Hassebrock, RD, LD. Used with permission.
| Potassium | Choose only the lowest potassium fruits, vegetables and juices Limit fruits to 1 ½ c. daily. Limit vegetables to ½ c. daily. Limit juice to ½ c. daily. |
| Phosphorus | Limit fluid milk to ½ c. daily. Avoid cheese, yogurt and ice cream. |
| Protein Foods | Limit meat, poultry, fish and eggs to a total of 4 oz. daily. Avoid high sodium items like peanut butter, ham, bacon, sausage, hot dogs, and processed lunchmeats. |
| Fluids | Limit salty foods to avoid drinking too much water or other beverages. Drink only half the amount of fluids usually allowed. |
| Carbohydrates | Eat more buttered white bread or rolls, rice, buttered pasta, cereal (without nuts and fruit), low salt crackers, vanilla wafers, bagels, English muffins, tortillas, angel food cake, unsalted pretzels and popcorn, rice cakes or animal crackers to satisfy hunger. |
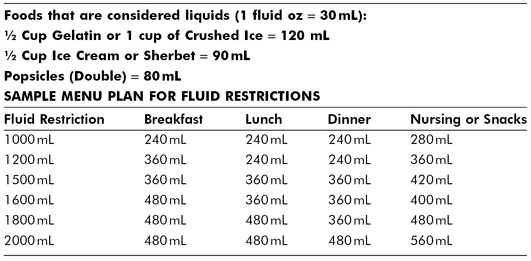
FLUID RESTRICTIONS
All foods contain some fluid; however, only foods liquid at room temperature or that become liquid when swallowed—such as gelatin—need to be counted.
Table 9.6 Fluid Restrictions
REFERENCES
1. Lopes AA, Elder SJ, Ginsberg N, et al. Lack of appetite in haemodialysis patients-associations with patient characteristics, indicators of nutritional status and outcomes in the international DOPPS. Nephrology Dialysis Transplantation. 2007;22:3538–46.
2. American Dietetic Association. Position paper of the American Dietetic Association: Liberalization of the diet prescription improves quality of life for older adults in long-term care. J Am Dietetic Assoc. 2005;105:1955–65.
3. Brink BR, & Reams SM. Renal diets for nursing facilities: A team approach. The Consultant Dietitian. 1997;21(1):4–6.
4. Chazot C, & Kopple JD. Vitamin metabolism and requirements in renal disease and renal failure. In: Kopple & Massry’s Nutritional Management of Renal Disease (ed. Kopple JD, & Massry SG), 2nd ed., pp. 315–56. Philadelphia: Lippincott Williams & Wilkins, 2004.
5. Moe SM. (2004) Calcium, phosphorus and vitamin D metabolism in renal diseases and chronic renal failure. In: Kopple & Massry’s Nutritional Management of Renal Disease (ed. Kopple JD, & Massry SG), 2nd ed., pp 261–85. Philadelphia: Lippincott Williams & Wilkins, 2004.
6. Wilkins KG, & Juneja V. Medical nutrition therapy for renal disorders. In: Krause’s Food and Nutrition Therapy, (eds L.K. Mahan & S. Escott-Stump), 12th ed., p. 940. St. Louis: Saunders Elsevier, 2008.
7. National Kidney Foundation. K/DOQI clinical practice guidelines for nutrition in chronic renal failure. American Journal of Kidney Disease. 2000;35(Suppl 2).
8. Biesecker R, & Stuart N. Nutritional management of adult hemodialysis patient. In: A Clinical Guide to Nutrition Care in Kidney Disease (eds. Byham-Gray L., & Wiesen K.), p. 45. Chicago: Renal Dietitians Dietetic Practice Group of the American Dietetic Association and Council on Renal Nutrition of the National Kidney Foundation, 2004.
9. McCann L. (2004) Nutritional management of adult peritoneal dialysis patient. In: A Clinical Guide to Nutrition Care in Kidney Disease (eds. Byham-Gray L., & Wiesen K.), p. 64. Chicago: Renal Dietitians Dietetic Practice Group of the American Dietetic Association and Council on Renal Nutrition of the National Kidney Foundation, 2004.
10. Sarkar SR, Kotanko P, & Levin NW. Interdialytic weight gain: Implications in hemodialysis patients. Seminars in Dialysis. 2006;19:429–33.
11. Ag Research Service Nutrition Database, Release 22: nal.usda.gov/fnic/foodcomp/search.
12. Wiggins KL. Renal Care: Resources and Practical Applications. Chicago: ADA-RPG, 2004.
13. Renal Practice Group of the American Dietetic Association. National Renal Diet, Professional Guide, 2nd ed. Chicago: ADA-RPG, 2002.
14. Yap HJ, Chen YC, Fang JT, et al. Star fruit: A neglected but serious fruit intoxicant in chronic renal failure. Dialysis & Transplant. 2002;31:564–67, 597.
NUTRITIONAL GUIDELINES FOR LIVER DISEASE
Liver (hepatic) disease may require physician ordered protein, sodium, fat, calorie controlled, or fluid intake restrictions. The goal of nutrition therapy in patients with liver disease is to maintain the best nutritional status possible and manage the symptoms of liver disease without causing further damage to the liver.
Alcoholic liver disease develops when the liver has too much alcohol to handle and is not able to process it. The first stage of alcoholic liver disease is fatty liver in which fat deposits in the liver. Fatty liver can be reversed by avoiding alcohol.
Nonalcoholic liver disease develops when dietary intake of excess fat exceeds the liver’s capacity to process it. When the body transfers fat from other parts of the body to use and the liver is not able to metabolize it, more fat deposits in the liver. Fatty liver can be caused by many factors (other than alcohol) including obesity, excessive calorie intake, protein malnutrition, chronic use of total parenteral nutrition, intestinal bypass for obesity, diabetes and insulin resistance, and infection. Fatty liver can be reversed if the reason for the damage can be removed.
When damage is done to the liver, permanent scarring (cirrhosis) can lead to liver failure or liver cancer. Fluid retention is a complication of cirrhosis that can cause abdominal swelling (ascites) or edema. If liver disease progresses, it can lead to hepatic encephalopathy (type of brain damage from a build up of ammonia).
Diet Principles
The type of liver disease and other conditions your patient will affect what nutritional modifications are needed.
1. Calories from a variety of foods are needed to maintain a healthy weight and help the liver function as well as it can. If weight loss is needed it should be done slowly, not more than 1 pound per week. Smaller meals and snacks throughout the day may help ensure adequate calorie intake at 25–35 kcal/kg dry weight.
2. Protein is important for liver cell repair. A malnourished patient will need adequate amounts of protein to prevent breakdown of the body’s protein stores. Dairy and vegetable proteins are easier to tolerate than animal proteins. Protein restrictions should be cautioned due to the risk of malnutrition. If a protein restricted diet is necessary, use the following guidelines for reducing protein intake from a General Diet.
3. Carbohydrates. Complex carbohydrates high in fiber, whole grain foods, and a variety of fresh fruit and fresh vegetables should be encouraged. Fiber goal should be 25 grams per day. Excess calories in the form of simple, refined carbohydrates can cause hyperglycemia and more fat deposits in the liver.
4. Fat intake should be 30% or less of total daily calories. Avoid as much saturated fat and trans fats as possible to help decrease hyperlipidemia. Refer to the Heart Healthy Diet in Chapter 7. Be sure to incorporate essential fatty acids (linoleic and linolenic fatty acids). Some patients may have problems with digestion or absorbing fat, which then is lost in the stool; medium chain triglycerides (MCT) oil is absorbed more easily by the body and may be useful in meeting energy needs.
5. Sodium should be limited to maintain normal fluid and electrolyte balance. Those that have fluid retention and swelling in the abdomen wall (ascites) or the legs (peripheral edema) need a Low Sodium Diet (Chapter 8).
6. Fluids may need to be limited (1,000–2,000 mL of fluid per day) if serum sodium levels are low or if fluid retention is not well controlled. See Fluid Restrictions in Chapter 9.
7. A vitamin supplement with adequate B-complex vitamins, vitamins A, C, D, E, and K, and folate may be needed. Thiamin may need to be higher in alcoholic liver diseases. Avoid mega-vitamin supplements, especially vitamins A and D. Excess vitamin A is toxic to the liver.
8. Alcohol should be avoided to allow the liver a chance to heal, rebuild, and a chance for new cells to grow.
9. Beware of “natural” diet treatments and herbal remedies because many are quite dangerous and toxic to the liver.
10. In malnourished patients, enteral nutrition support at 1,200 calories and 45 grams of protein per day may be needed plus oral intake. (1,2)



