201 Diabetic retinopathy
Instruction
Examine the fundus in these patients.
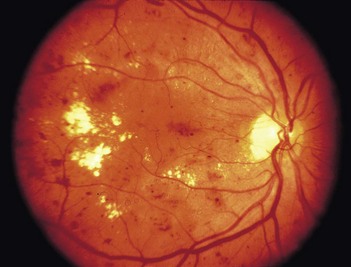
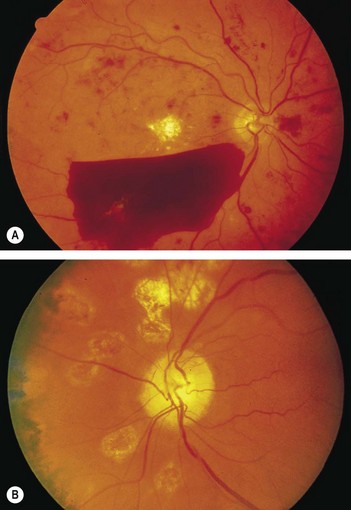
• You will be expected to comment on whether it is background (Fig. 201.1) or proliferative (Fig. 201.2) retinopathy.
• You may have a clue about the underlying diabetes, either from a diabetic chart or from the presence of diabetic fruit juices at the bedside.