16 Diabetes mellitus and hyperlipidaemia
Diabetes Mellitus
Who classification of diabetes
Type 2 diabetes mellitus
Type 2 DM (> 90% of total) results from a progressive fall in insulin secretion with, in addition, resistance to the action of insulin. It is frequently associated with obesity and the ‘metabolic syndrome’ (p. 429). Early in the disease, there may be high levels of circulating insulin, in contrast to type 1 diabetes. Hyperglycaemia results from a progressive failure of the pancreatic β-cells to maintain high levels of insulin secretion to overcome peripheral resistance. The diagnosis is therefore often delayed since endogenous insulin levels are initially sufficient to prevent ketogenesis and a catabolic state. Intercurrent illness, with increased insulin resistance secondary to release of stress response hormones, is associated with worsening glycaemic control and consequent dehydration. The presentation is often with a concurrent illness in an adult with a history of polyuria, polydipsia and malaise over some weeks.
Higher-risk population groups that may benefit from screening for type 2 diabetes include:
Other types of diabetes
Diagnosis
Diagnostic criteria
• Impaired glucose tolerance (IGT)
Management of diabetes
The aims of management are to:
Insulin therapy
Insulin is the only therapy suitable for the treatment of type 1 diabetes and in cases where endogenous insulin production has been significantly reduced, such as haemochromatosis. Interruptions in insulin therapy render these individuals at risk of ketosis. Insulin is also used to cover periods of intercurrent illness in type 2 diabetes when insulin resistance is increased, or there are concerns that hepatic or renal clearance of an oral drug may be impaired. Progressive β-cell failure is seen in type 2 diabetes and thus oral antidiabetic agents may with time fail to control glycaemia adequately. While there is often resistance to injectable therapy, either through patient preference or a fear of weight gain, initiation of insulin in this group of patients should not be delayed.
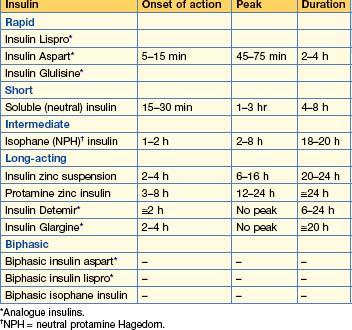
Insulin formulations (Table 16.1)
Principles of insulin treatment
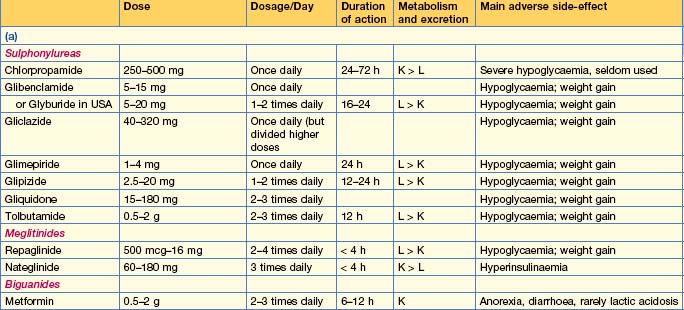
Oral antidiabetic drugs (Table 16.2)
Insulin secretagogues
Insulin sensitizing agents
Intestinal enzyme inhibitors
Other therapies
• Incretins
Practical management of type 1 DM
Monitoring
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree