Chapter 13 Diabetes
Introduction
Type 1 diabetes mellitus (T1DM) — prevalence and incidence
The prevalence of T1DM accounts for about 10% of all cases of diabetes, occurs most commonly in people of European descent and affects more than 2 million people in Europe and North America.1, 2 A recent update reported that in the US the prevalence of diagnosed and undiagnosed diabetes (all forms in all ages as at 2007) totalled 23.6 million people — 7.8% of the population had some form of the disease. That is, those diagnosed accounted for 17.9 million people and undiagnosed 5.7 million people.2
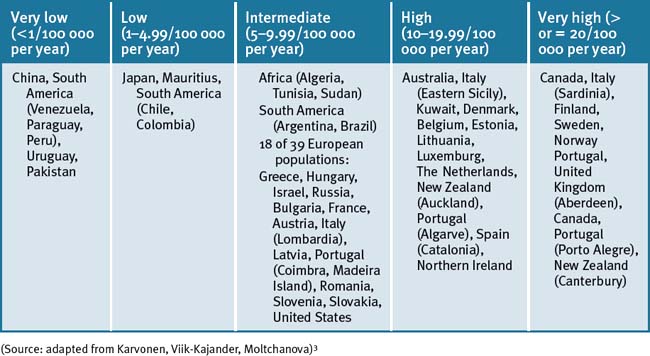
There is also a wide variation in incidence of T1DM from country to country that is evident globally.3 For example, the marked geographic variation in incidence is clearly evident from data that show that a child in Finland has approximately 400 times the likelihood than does a child in Venezuela to acquire the disease.2, 3, 4 Moreover, the incidence of T1DM in children is increasing in Western countries.2, 5, 6 The global incidence of T1DM in children less than or equal to 14 years of age as calculated per 100 000 population has marked variation within ethnic and racial distribution in the world population, as summarised in Table 13.1. The incidence increases with age, highest at 10–14 years of age.
There are also further sub-group variations of T1DM incidence within populations.2, 3, 4 For instance, in the US, non-Hispanic white youth have a higher risk of T1DM.2 A multiethnic, population-based study in the United States estimated the incidence of T1DM (per 100 000 person-years) was 24.3 in children (less than 19 years of age) with the highest rate observed in non-Hispanic white youth (18.6, 28.1, and 32.9 for age groups 0–4, 5–9, and 10–14 years, respectively).7
Type 2 diabetes mellitus (T2DM) — prevalence and incidence
As with T1DM the prevalence of T2DM also varies extensively for different populations from distinct geographical areas.8 At the end of the 20th century, it was estimated that 150 million people in the world had diabetes and the World Health Organization (WHO) predicts that, between 1997 and 2025, the number of patients with T2DM will double to reach about 300 million.9, 10 According to the WHO, T2DM affects up to 7% of Western populations and is increasing in newly industrialised and developing countries.11
The heightened susceptibility and high prevalence of T2DM of Micronesian and Polynesian Pacific Islanders,10, 12 Native Americans,13 Indigenous Australians and Torres Strait Islanders,10, 14 and Asian Indians14 has been well documented.
In Australia, the prevalence of T2DM has been reported to have doubled since 19816, 10 (Table 13.2).
Table 13.2 Australian prevalence of T2DM
| Men | Women | |
|---|---|---|
| Prevalence | 8% | 6.8% |
| Impaired glucose tolerance and/or impaired fasting glucose | 17.4% | 15.4% |
There are a number of risk factors that have been identified with the development of T1DM and T2DM (Table 13.3).
Table 13.3 Risk factors that have been reported to be associated with T1 and T2DM
| Risk factors for T1 and T2DM |
|---|
(Source: adapted from Adamo, Tesson)15
The number of adolescents with T2DM diagnosed yearly is also increasing globally and has been attributed to factors such as weight gain, poor nutrition and lack of exercise.16
Lifestyle — general, education and prevention of T2DM
Intensive lifestyle interventions can reduce the incidence of diabetes in people with impaired glucose tolerance, so encouragement of positive lifestyle strategies is essential where social opportunities arise, such as with school education, religion or in any other social community situations. Lifestyle changes can lead to lifelong changes and reduce the incidence of diabetes or complications associated with diabetes, even after active counselling has ceased.17 A post-intervention follow-up study of participants found the risk of developing T2DM was reduced by 43% over a 7-year median period for those who received intensive lifestyle counselling compared with standard intervention.17
A systematic review and meta-analysis of the literature identified 17 randomised trials of 8084 participants and confirmed the value of intensive lifestyle intervention counselling to prevent and delay T2DM onset in people with impaired glucose tolerance.18 Healthy diet and exercise is much more effective at preventing T2DM than drug therapy. When comparing lifestyle intervention and metformin, a study of 3234 subjects over 3 years with impaired glucose tolerance were randomly assigned to a group of placebo, metformin, or a lifestyle-modification program involving diet and exercise over a 2.8 year follow-up. Lifestyle intervention reduced the incidence of developing T2DM by 58% compared with metformin by 31%.19
The aim of a healthy lifestyle to prevent T2DM:
T2DM is associated with a Westernised lifestyle. Lifestyle management is the most effective way of preventing T2DM, especially with dietary measures and exercise. A recent Cochrane review of the literature emphasises the importance that combined diet interventions and exercise significantly reduces the risk of developing T2DM by up to 37% compared with standard recommendations (RR 0.63) with favourable modest effects on reducing blood lipids and blood pressure compared with exercise or dietary changes alone.20
A study of 577 Chinese adults with impaired glucose tolerance without T2DM from 33 Chinese medical clinics, were randomised to either a control group, or 1 of 3 lifestyle intervention groups that included diet or exercise alone, or diet with exercise over a 6-year period and an assessment of the lifestyle intervention group again in the 20 year follow–up.21
The combined lifestyle intervention group significantly reduced the incidence of developing diabetes by up to 51% over the 6-year period and up to 43% in the 20-year follow-up compared with the control group, and significantly more than the diet and exercise groups alone. This study emphasises the importance of promoting intensive lifestyle changes to prevent diabetes onset, particularly in patients with reported impaired intolerance or at high risk of developing DM.21
Dietary factors and T1DM
Cow’s milk consumption in early infancy
Children fed cow’s milk during the first few days of life are twice as likely to develop T1DM than children who are breast fed.22 The association between T1DM may be explained by the generation of specific immune response to beta casein from cow’s milk exposure, triggering cellular and humoral anti- β casein immune response which may cross-react with beta-cell antigen.23 Overall high cow’s milk consumption (3 or more glasses of cow’s milk a day) was associated with a 5.4 fold increased risk of developing T1DM in young children, and this was higher in children who also had HLA genotype for diabetes.24
Dietary factors and T2DM
Obesity is the main cause of developing T2DM according to large scale studies. Whilst lack of physical activity also contributes, the risk of T2DM rises progressively with increasing Body Mass Index (BMI), increasing waist circumference, and obesity.25
Epidemiologic studies suggest that greater consumption of fruit and vegetables reduces the risk of diabetes mellitus. In a population-based prospective cohort (European Prospective Investigation of Cancer–Norfolk) study, 21 831 individuals aged 40–75 years at baseline were assessed for plasma vitamin C level and habitual intake of fruit and vegetables over a 12-year follow-up period. The researchers found a strong inverse association between plasma vitamin C level and T2DM risk. High plasma vitamin C level and, to a lesser degree, fruit and vegetable intake was associated with a substantially decreased risk of T2DM.26
Cultural factors and prevention
Minority ethnic groups found that upper-middle and high-income countries often suffer a higher prevalence of T2DM than the local population, due to cultural and communication barriers, being of lower socioeconomic backgrounds, and having less access to good quality health care.27
For instance, a UK study of a Bangladeshi community found the Islam norms and teachings offers many opportunities for supporting diabetes prevention. The authors noted that interventions designed for the white population needed to be adapted to be meaningful to the Bangladeshi community. So religion may play an important role in supporting health promotion in any sub-community. Working collaboratively between health educators, health professionals and religious leaders should be explored to promote positive lifestyle changes within communities.28
Breastfeeding and prevention
Women breastfeeding for over 6 months significantly reduces the woman’s risk of developing T2DM later in life. The longer the duration of breastfeeding, the greater the protection against T2DM.
A large scale prospective observational cohort study of 83 585 parous women identified a strong association of duration of breastfeeding and the incidence of T2DM. Whilst controlling for other relevant risk factors such as BMI, the study found that the longer the women breastfed the less likely they would develop T2DM. For each additional year of lactation, women with a birth in the prior 15 years had a decrease in the risk of diabetes of up to 15% amongst participants. Lactation improves glucose homeostasis.29
Gender factors and prevention
Studies indicate, in general, women with risk factors and a family history of diabetes were more likely to obtain diabetes education, gain benefits of self-management and reported higher levels of social support from their diabetes health care team than men did. This highlights the special needs for men with respect to diabetes education, understanding risk factors, prevention, self-care and self-management of T2DM.30
Genetics
Whilst studies suggest T1DM is associated with a wide spectrum of susceptibility and protective genotypes within the HLA class II system, it is likely that increasing environmental exposure is able to trigger these genes even in subjects who are less genetically susceptible.31
T2DM is the most common disease in the Western world today that has a genetic link.32 It is the phenotype for more than 150 genotypes.32, 33, 34 Each of these genotypes is characterised by impaired glucose tolerance and impairment of the control of intermediary metabolism.
Mind–body medicine
Meditation, biofeedback, and hypnosis have all been found to improve T2DM.35
Life stressors and/or depression
Stress may be a contributor to T1DM onset according to a prospective population-based study of almost 6000 children. The study demonstrated children had a threefold risk of developing autoimmunity T1DM if their parents divorced or experienced violence during the child’s infancy within 2.5 years of the event.36 The authors concluded that ‘maternal experiences of serious life events…seem to be involved in the induction or progression of diabetes-related autoimmunity in children’.36 Bullying, a form of stress for a child, is also known to adversely affect glycaemic control and self-management, and increase feelings of depression in T1DM children.37
Research demonstrates that regular use of stress management techniques can significantly reduce blood glucose levels in T2DM. After 1 year, compared with control, stress management reduced HbA1c by up to 1% which is clinically significant. Stress management would be a useful addition to a lifestyle intervention program for diabetics.38
Even daily hot baths for relaxation has been shown to lower fasting serum glucose in diabetics.39 The researchers postulated the benefits could result from increased blood flow to skeletal muscles.
Stress and depression both influence hormonal levels.40 Stress and depression increase cortisol, growth hormone and adrenaline. Cortisol and growth hormone increase insulin resistance, and adrenaline stimulate the breakdown of glycogen into glucose (glycogenolysis).41
Depression is associated with insulin resistance and with diabetes.35 Low mood, mild and moderate depression is 2 to 3 times more common in diabetics than in non-diabetics, and is frequently not diagnosed or treated.42 Insulin resistance is positively associated with the development of diabetes.43 A large prospective scale study of 4847 participants without depression symptoms at baseline, at 3 years, treated T2DM was significantly associated with depression with an odds ratio of 1.52, even after adjusting for BMI, socioeconomic status, lifestyle and diabetes severity, and after excluding T2DM patients on antidepressants possibly for diabetic neuropathy. It was felt that depression contributed to diabetes and diabetes also contributed to depression.44
In another large scale study of more than 4600 patients over 65 years or older, depression symptoms over time was associated with a higher incidence of T2DM after adjusting for other diabetic risk factors.45
In a study of patients with work-related depression, the authors found the presence of depression or depressive symptoms was associated with subsequent increased risk of developing T2DM. The relative risk was 1.25 (95% confidence interval [CI]:1.02–1.48) compared with workers not experiencing depression.46
There is a positive correlation between insulin resistance and severity of depressive symptoms with impaired glucose tolerance before the outbreak of T2DM.47
A recent study found that serotonin receptor agonists can improve glucose tolerance, and reduce plasma insulin levels.48
Hence, the proper management of depression and stress are key factors in reducing the risk and progression of diabetes (see also Chapter 12).
Sunshine and Vitamin D
Vitamin D deficiency plays an important role with both insulin synthesis and secretion by way of vitamin D receptors and vitamin D binding proteins in pancreatic tissues as demonstrated in both human and animal models. The mechanism of action of vitamin D is also thought to occur as a direct action on pancreatic beta-cell function and mediated through regulation of plasma calcium levels, which may explain why vitamin D deficiency may play a role in the causation in T1 and T2DM.49
Lack of sunshine exposure is contributing to vitamin D deficiency as most vitamin D forms in the skin as a result of ultraviolet radiation (UVB wavelength; 290–320 nm) exposure from sunlight.50
People living in the southern regions of the southern hemisphere or the northern regions of the northern hemisphere have a higher risk of vitamin D deficiency, particularly during the winter months. Certain ethnic groups are at increased risk of vitamin D deficiency, especially dark skinned people who cover their skin for religious or cultural reasons, the elderly, babies of vitamin D deficient mothers, and people who are housebound or are in institutional care.51
T1DM
There is a significant body of biologically plausible evidence that strongly suggests that vitamin D plays a role in the prevention of T1DM. Giving infants vitamin D supplementation could protect them from T1DM according to a systematic review of 5 observational studies that showed a reduced risk of T1DM by up to 30% compared with infants not supplemented.52
Sleep
A number of studies have demonstrated a strong link between lack of sleep or over-sleeping with T2DM. The odds of developing T2DM for subjects sleeping 5 hours or less or 9 hours or more was associated with a significant increase risk of developing T2DM or impaired glucose tolerance test. Factors such as more environmental lighting, long working hours, television and personal computers are contributing to shorter sleep durations in Western societies.54, 55
Obstructive sleep apnoea may also be a risk factor for T2DM.56
Insomnia, anxiety and depression may double the risk of diabetes in men by 2.2 times compared with those with low levels of psychological distress, independent of risk factors such as BMI, family history for diabetes, and smoking, according to a study of 2127 men and 31 000 women followed up over 8–10 years. Of interest, women with psychological distress and insomnia did not have a higher risk of diabetes.57
Environment
Smoking
Researchers have combined the best available information from 25 studies in a systematic review which followed the health of 1.2 million people for several years.58
There is an increased risk of T2DM of approximately 50% from smoking and the more a person smoked the higher the risk and vice-versa; smoking preceded the development of T2DM.58 Smoking has an adverse effect on pancreatic function. It may cause internal inflammation and increase abdominal fat, even in thin smokers, which could then lead to an increase in insulin resistance. Smoking becomes even more of a problem when combined with T2DM risk-enhancing behaviours such as obesity and inactivity.59
Further studies have confirmed this association. In a study of 906 participants free of DM at baseline and after multivariable adjustment, the researchers found of the current smokers, 25% developed T2DM at 5 years, compared with 14% of those who never smoked.60
Arsenic exposure
Environmental exposure to low levels of inorganic arsenic in drinking water has been associated with diabetes development. Millions of people world-wide are exposed to inorganic arsenic in water from natural mineral deposits. A cross-sectional USA study of 788 adults aged 20 years or older based on a 2003–2004 survey, urine arsenic levels, and after adjustment for biomarkers such as seafood intake, total urine arsenic was associated with increased prevalence of T2DM. Participants with T2DM had a 26% higher level of total arsenic in their urine than participants without T2DM. After similar adjustment, the odds of developing T2DM led to a 3.6 fold increase risk associated with exposure of arsenic. The authors speculated that arsenic could induce diabetes through oxidative stress, inflammation or apoptosis.61
Physical activity
Physical activity is one of the key modifiable risk factors for hyperglycaemia. Evidence from population-based, cross-sectional studies report that both decreased physical activity and elevated sedentary behaviours, such as television viewing time, are independently associated with raised blood glucose levels in adults without a diagnosis of diabetes.62, 63 Regular exercise benefits T1DM and T2DM. Children with T1DM showed improved haemoglubin A1c (HbA1c) and glycaemic control with regular exercise of at least 3 times weekly compared with children who did not exercise.64, 65
Walking just 30 minutes daily can significantly reduce the incidence of T2DM.66 Walking 2 hours weekly can reduce mortality from all causes by 39% and by 34% from cardiovascular disease in patients with T2DM.67 A study of healthy young sedentary men demonstrated a high intensity aerobic exercise protocol comprising a total of 15 minutes of exercise (6 sessions; 4–6 30-second cycle sprints per session) substantially improved insulin action and glucose tolerance test, and supported the important role of exercise in preventing diabetes.68
The size of cities can influence the risk of diabetes. When a person migrates from a rural environment or third-world country to the city or a Western country the risk of T2DM is significantly elevated.69, 70 If that city happens to be of more than 1 million in population, as described in a recent study,69 then the risk of diabetes increases fourfold. It is thought that the design of cities can influence whether the people walk or not.
The position statements from both the American Diabetes Association and the American College of Sports Medicine, has recommended the use of resistance training as part of a physical activity program to reduce the risk of developing diabetes.71, 72
A Cochrane meta-analysis of 14 randomised controlled trials (RCTs) comparing exercise against no exercise in 377 participants with T2DM found that compared with control and independent of weight loss, exercise intervention significantly improved glycaemic control as indicated by a significant decrease in glycated haemoglobin levels of 0.6% (−0.6% HbA1c, 95%CI −0.9 to –0.3; P < 0.05), reduced visceral adipose tissue, plasma triglycerides but not cholesterol levels.73
Of interest, studies indicate aerobic and resistance training alone improves glycaemic control in T2DM, but improvements were greatest with a combined exercise training of both aerobic with resistance training.74
Tai chi
Tai chi is a Chinese system of slow meditative physical exercise designed for relaxation, balance and health. Tai chi has demonstrated improved balance, gait speed, muscle strength, cardiorespiratory fitness, and quality of life in older adults.75–80
However, recent studies including a systematic review have demonstrated that there is some controversy as to its efficacy for patients with T2DM.81
Recently reported RCTs have demonstrated a change in fasting blood glucose levels.79–82 One RCT demonstrated no significant intergroup differences in fasting blood glucose levels compared with a placebo intervention.83
One Chinese clinical trial84 reported superior effects of tai chi on fasting blood glucose levels compared with walking or running, while 2 other Chinese clinical trials85, 86 reported that there was no difference compared with a self-management program, or no treatment.
Three clinical trials reported assessing the effectiveness of tai chi on HbA1c.83, 84, 85 Of these only 1 RCT85 suggested no effectiveness of tai chi on HbA1c compared with a sham exercise regimen whereas 2 Chinese clinical trials83, 84 failed to report intergroup differences compared with no treatment, self-management, walking or running exercise activities. One recent Chinese clinical trial with women diagnosed with T2DM reported that the tai chi group had significantly improved glycaemic control and serum triglyceride levels.86
Qigong
Qigong is another Chinese health practice that is associated with a system of healing and energy medicine. Preliminary studies show positive effects for qigong and reflexology in T2DM.87, 88
A recent review has concluded that although qigong has beneficial effects on some of the metabolic risk factors for T2DM, there exist methodologic limitations that hence make it difficult to draw firm conclusions about the purported benefits.89 Further clinical trials are warranted.
Further, a recent clinical study adds significant strength to the role of tai chi and/or qigong in the management of the metabolic syndrome and glycaemic control in pre-T2DM.90
Yoga
There are few studies that have investigated the efficacy of yoga in T2DM.
Three small studies from India have demonstrated and suggested that yoga asanas and pranayama can better manage glycaemic control and stabilise autonomic functions in T2DM cases.91, 92, 93 Moreover, in 1 of these studies it was reported that yoga improved sub-clinical neuropathy.93
A recent community-based study of yoga classes for T2DM aimed to demonstrate benefits of yoga for diabetic patients but unfortunately experienced ‘recruitment challenges; practical and motivational barriers to class attendance; physical and motivational barriers to engaging in the exercises; inadequate intensity and/or duration of yoga intervention; and insufficient personalisation of exercises to individual needs’ and these factors need to be considered in any future research.94 It also highlights how research in yoga can be difficult.
A systematic review of the literature identified 25 eligible studies, including 15 uncontrolled trials, 6 non-RCTs and 4 RCTs. Overall, the studies demonstrate yoga showing benefit in several risk indices, including ‘glucose tolerance and insulin sensitivity, lipid profiles, anthropometric characteristics, blood pressure, oxidative stress, coagulation profiles, sympathetic activation and pulmonary function, as well as improvement in specific clinical outcomes’.95 Again, the authors acknowledge the limitations of these studies when drawing firm conclusions and encourage additional high-quality trials to confirm the benefits of yoga in diabetics.95
Diet and nutrition
For both Type 1 and Type 2DM, a low-GI diet can ‘improve glycaemic control in diabetes without compromising hypoglycaemic events’ according to a recent Cochrane review of the literature of 11 relevant RCTs involving 402 participants, although no study reported on mortality, morbidity or costs.96 Low glycaemic diet led to a significant decrease in the glycated haemoglobin A1c (HbA1c) and less episodes of hypoglycaemia compared to high GI diet.96
T1DM
A study of 1776 young children (less than 11.5 years of age) who were at increased risk of genetic type 1 diabetes demonstrated that high dietary GI (hazard ratio [HR]: 2.20, 95% CI: 1.17–4.15) and high glycaemic load (HR: 1.59, 95% CI: 0.96–2.64) were associated with rapid progression of islet autoimmunity (IA) to T1DM. Furthermore it was reported that this was possible due to an increased demand on pancreas beta-cell release of insulin and that the development of IA was not associated with high GI foods.97
High fish consumption in the diet may also play an important role in the prevention of T1DM onset. A 12-year study reported a diet rich in omega-3 oils, primarily from fish and other seafood, can reduce the chances of high-risk children developing pancreatic islet beta cell autoimmunity and T1DM by up to 55%. The researchers speculated that omega-3 fatty acids may accentuate T-helper 1 activity associated with autoimmunity and its anti-inflammatory effects may contribute to its benefits.98
A recent study of 532 people over a 5-year period demonstrated that diets high in fat, saturated fat and lower in carbohydrates were associated with worse glycaemic control in T1DM, independent of exercise and BMI.99
T2DM
A low GI diet is as effective as medication in improving glycaemic control in diabetics. Patients with T2DM should be under the care of a dietician or diabetic educator to continually monitor their diet. Dietary compliance is fundamental in the management of T2DM.100
A recent study has reported that in those individuals that are at risk for developing T2DM a change in lifestyle that includes dietary manipulation with a significant decrease in fat intake and a concomitant increase in vegetable and fruit consumption resulted in marked inhibition of the transition from the pre-diabetic state to manifest T2DM.40
It has been documented that a diet rich in wholegrains and seafood will be high in magnesium.41, 101
There is a strong inverse relationship to T2DM with magnesium.102 Also, such diets may be protective against the development of T2DM.103 Wholegrain intake is inversely associated with homocysteine and markers of glycaemic control, and studies suggest a lower risk of diabetes and heart disease in persons who consume diets high in wholegrains.104
Foods rich in soluble fibre such as oats, legumes, guar gum and psyllium are more slowly absorbed and produce lower blood glucose levels.105 Increasing dietary fibre up to 50g daily (such as raisins and oranges) can improve glycaemic control in patients with T2DM.106 There is increasing evidence that inflammation plays an important role in the pathogenesis of diabetes, as obesity is associated with a pro-inflammatory state.107
A Cochrane review that investigated the potential effects of wholegrain foods for the prevention of T2DM has concluded that studies have consistently demonstrated that a high intake of wholegrain foods or cereal fibre is associated with a lower risk of the development of T2DM.108 However, the evidence for a protective effect coming from prospective cohort studies only has to be considered as weak as with this design no cause and effect relationship could be recognised. Hence, it was further concluded that well-designed RCTs are warranted that are able to draw definite conclusions about the preventive effects of wholegrain consumption on the development of T2DM.108
Fish
Fish is protective towards the development of T2DM apart from having a number of health benefits by preventing cardiovascular disease. In a study of insulin-resistant participants, a high fish diet improved insulin sensitivity compared with participants not eating fish.109 Greater fish intake was associated with a lower risk of macroalbuminuria in a self-defined diabetic population.109
An anti-inflammatory diet can include fish, nuts, flaxseeds, fruits and vegetables, ginger and turmeric.110, 111 Partially hydrogenated oils, as in vegetable oils and margarines, are pro-inflammatory and can increase the risk of T2DM.112
Other protective foods
Garlic, green tea, chilli and onions have all been shown to have beneficial effects in DM. Onion and garlic can decrease blood glucose, cholesterol and blood pressure.113, 114
Two RCTs have found that supplementation with soy protein in T2DM improves fasting insulin, insulin resistance, total and low-density lipoprotein (LDL) cholesterol,115, 116, 117 which also showed soy improved glucose control. They also found that regular consumption of chilli could attenuate postprandial hyperinsulinemia.118
Diets with low GI and glycaemic load will modulate swings in blood glucose levels and insulin secretion because of slower absorption and have been shown to improve haemoglobin A1c (HbA1c).115
Other food considerations
Rice consumption
There are also cultural dietary differences that may contribute to high prevalence of diabetes in specific population groups. For instance, in a cohort of 64 227 Chinese women with no history of diabetes or other chronic disease over a 4.6 year period the authors noted dietary carbohydrate intake and consumption of rice (high GI and load) was positively associated with increased risk of developing T2DM.119
Sugary drinks
T2DM is a common problem amongst African American women. A prospective follow-up study of 59 000 African American women reported on food and beverage consumption between 1995 and 2001 and found, after adjusting for relevant confounders such as BMI, the incidence of T2DM was associated with higher intake of both sugar-sweetened soft drinks and fruit drinks. Two or more soft drinks per day increased the risk by 1.24 (95% confidence interval, 1.06–1.45) and for fruit drinks, the comparable incidence rate ratio was 1.31 (95% CI, 1.13–1.52).120
Artificial flavours
A recent animal study with rats found foods using artificial sweeteners resulted in ‘increased caloric intake, increased body weight, and increased adiposity, as well as diminished caloric compensation and blunted thermic responses to sweet-tasting diets’. These results suggest that consumption of foods containing artificial sweeteners may lead to increased body weight and obesity, and so should be avoided.121
Meat intake
High intake of red meat significantly increases the risk of fatal coronary heart disease (CHD) in women with T2DM. Women who consumed the highest levels of haeme iron and red meat also had a 50% increased risk of developing CHD compared with women who consumed the lowest intake.122
Low fat dairy intake
A large scale prospective women’s health study of 37 183 middle-aged non-diabetic women found low fat dairy and yoghurt consumption significantly reduced the risk of developing T2DM.123
A diet rich in low fat dairy food in T2DM helps reduce weight in the overweight and the researchers found no association between dairy calcium intake and other diabetes or CVD disease indexes.124
Vegetarian, plant-based diet
A review of the literature demonstrates a strong link between vegetarian and plant-based diets in reducing the risk of obesity, T2DM, heart disease and some cancers.125 A diet high in vegetables and vegetarianism can significantly reduce the risk of diabetes, improve glycaemic and lipid control and reduce cardiovascular complications.126, 127
Body weight
Obesity is the main predisposing risk factor for the development of diabetes.128
The prevalence of obesity varies among different racial groups and it is associated with approximately 30% of Chinese and Japanese patients with T2DM. Obesity is found in 60–70% of people in Western countries and, although estimates vary, it is thought that the prevalence of T2DM could be as high as 30% of aboriginal people.129 Pima Indians, Pacific Islanders from Nauru or Samoa will all almost certainly develop T2DM with obesity.130
In a study of 1079 participants, intensive lifestyle intervention for overweight patients with impaired glucose tolerance reduced the 3-year incidence of overt T2DM from 35% to 15% by losing 5 kg compared with the control intervention. Every 1 kg of weight loss resulted in a relative risk reduction of developing TSDM by 16%.131
A number of dietary regimes have been recently reported as alternatives for macronutrient intake and the prevention of chronic diseases.132 A comparative study that included the macronutrient contents of 7-day menu plans from the Omni-Heart Study, Dietary Approaches to Stop Hypertension (DASH), Zone, Atkins, Mediterranean, South Beach, and Ornish diets were evaluated for consistency with the US Food and Nutrition Board’s Acceptable Macronutrient Distribution Ranges and with the dietary recommendations of several health organisations for the prevention of cardiovascular disease, cancer and metabolic syndrome. The intent of the study/analysis was to evaluate the healthfulness of the 3 Omni-Heart Trial diets high-carbohydrate (Omni-Carb), high-protein (Omni-Protein), and high unsaturated fat (Omni-Unsat) diets — and were compared with that of the DASH diet and 5 other popular diets, namely the Atkins, Ornish, South Beach, Mediterranean, and Zone diets. The resultant analysis reported that all 3 Omni study diets were consistent with US national guidelines to reduce chronic disease risk. Further, that, popular diets vary in their nutritional adequacy and consistency with guidelines for risk reduction.132
The Mediterranean diet
The Mediterranean diet with its emphasis on vegetables, grains, fish and olive oil has been shown to reduce the risk of atherosclerosis in diabetic patients.133, 134 There is a significant amount of evidence that strongly suggests that the Mediterranean diet could serve as an anti-inflammatory dietary pattern.135 This could help prevent diseases that are related to chronic inflammations that include visceral obesity, T2DM and the metabolic syndrome.135 The rationale for this evidence is further supported by a recent study that demonstrates that adherence to the Mediterranean diet is inversely associated with risk of developing diabetes and the clustering of hypertension, diabetes, obesity, and hypercholesterolemia among high-risk patients.136, 137
Monounsaturated fatty acids (MUFA) — olive oil and nuts
The MUFA (especially olive oil) in the Mediterranean diet appear to play an important preventative role for T2DM, even in healthy subjects. Insulin sensitivity reduced in healthy subjects on diets high in MUFA compared with diets high in saturated fatty acid. Subjects with the Ala 54 allele of the fatty acid-binding protein 2 gene demonstrated improved insulin sensitivity when the saturated fats were replaced by the MUFA.137
A large prospective cohort study involving over 83 000 university graduates without diabetes at baseline demonstrated high adherence to the Mediterranean diet with an 83% reduced risk of developing T2DM.138
Consumption of nuts and peanuts is related inversely with diabetes risk.139 Nuts may also confer cardiovascular benefit and improve lipid profile for patients with T2DM due to their high content of MUFA and nutritional value.140
After 6 months of adding 30g of walnut to a low-fat diet of T2DM patients, compared with those on no walnuts, the LDL cholesterol dropped by 10% and HDL cholesterol increased.141
Table 13.4 Healthy fats for diabetics’ monounsaturated fats
| Oils and margarines | Vegetables | Nuts |
|---|---|---|
| Polyunsaturated fats: | ||
| Oils and margarines | Fish and other seafood | Nuts and seeds |
| Canola, olive, macadamia, sunflower oil, peanut | Avocados, olives | Almonds, peanuts, cashews, hazelnuts, macadamias, pecans |
| Sunflower, safflower, corn, soybean, sesame, cottonseed, grapeseed, flaxseed oil or linseed | Walnuts, pine nuts, brazil nuts, sesame seeds, sunflower seeds, flaxseed or linseed | |
(Source: adapted from Phillips & Carapetis.)142
The Palaeolithic diet
A randomised control study of 29 patients with ischaemic heart disease plus either glucose intolerance or T2DM were randomised to receive (1) a Palaeolithic (‘Old Stone Age’) diet based on lean meat, fish, fruit, vegetables, root vegetables, eggs and nuts or (2) a Mediterranean-like diet based on wholegrains, low-fat dairy products, vegetables, fruits, fish, oils and margarines. The study demonstrated that the Palaeolithic diet — the basis of diet by humans before the introduction of grains, dairy, salt and refined fats and sugars — improved glucose tolerance with a 26% decrease of GI compared with 7% decrease in patients on the Mediterranean diet and independent of waist circumference.143
The Ornish diet
The Ornish diet was originally designed as a therapy to reverse cardiovascular disease and is also applicable to patients with diabetes. The Ornish diet consists of a low fat, high fibre, basically vegetarian diet with 75% of the kilojoules (calories) obtained from carbohydrates.144–146
Critical components of the Ornish dietary plan also include physical activity, yoga and relaxation therapy. In a group of T2DM patients requiring insulin who had adhered to the plan, 60% no longer required insulin at the end of the study.144
Caffeine
A systematic review of the literature identified coffee consumption as being protective towards the development of T2DM, reducing the risk by up to 35%.147
A large-scale longitudinal study demonstrated a significant reduction in incidence of glucose intolerance and T2DM of up to 64% in white middle-class people who drank regular coffee consumption compared with people who never drank coffee.148 This benefit persisted in those even after ceasing coffee consumption.
Similarly, another large-scale population-based study of approximately 2400 subjects found that coffee consumption was found to be significantly and inversely associated with fasting glucose, 2-hour plasma glucose, and fasting insulin in both men and women compared with non-drinkers of coffee.149
A prospective, community-based cohort of 12 204 non-diabetic, middle-aged men and women assessed risk of caffeine consumption as part of the Atherosclerosis Risk in Communities (ARIC) Study. After adjusting for potential confounders, increased coffee consumption was significantly associated with a decreased risk of diagnosed T2DM in community-based US adults.150
Cocoa
Based on epidemiological data, diets rich in flavanols are associated with reduced cardiovascular risk and may play a role in reversing vascular dysfunction in diabetics. Cocoa is rich in flavanols. In a study of 41 medicated diabetic patients over a 30-day period, dietary intervention with flavanol-rich cocoa (321mg flavanols per dose) significantly increased circulating flavanols, vascular function and flow-mediated dilation of the brachial artery compared with a nutrient-matched control (25mg flavanols per dose). The benefits of flavanol-rich cocoa (321mg flavanols per dose) were dose dependent up to 3 times daily.151
Alcohol
A large-scale US cross-sectional study of 32 000 people found an inverse relationship between alcohol intake and glycaemic control. On average, T2DM patients who drank alcohol in moderate amounts had HbA1c levels 1.2 less than non-drinkers.152
A multicenter trial randomly assigned 109 patients (41–74 years old) with T2DM who abstained from alcohol to receive 150 ml wine (13g alcohol) at dinner or non-alcoholic diet beer (control) each day during a 3-month period. The study found initiation of moderate daily alcohol consumption reduced fasting plasma glucose but not postprandial glucose and improved sleep in T2DM patients. The authors concluded alcohol may have a favourable glycaemic effect on HbA1c. There were no significant changes on liver function tests.153
Nutritional supplements
Vitamins
Antioxidant micronutrients may play a role in the prevention of diabetic complications.154
Vitamin C
A large population study has reported an inverse relationship between serum vitamin C levels and HbA1c.155 Vitamin C also improves endothelium-dependent vasodilatation in T2DM.156 A recently reported trial on the combined use of chromium and vitamins C and E as well as chromium on its own was effective for reducing metabolic dysfunction and improvement of glucose metabolism in T2DM patients.157
A study of 84 patients with T2DM were randomly assigned to either 500mgs or 1000mgs of vitamin C for 6 weeks. Whilst the dose of 500mgs daily vitamin C had no impact on blood parameters, the group taking 1000mgs of vitamin C daily demonstrated significant decrease in fasting blood sugars, triglyceride and LDL cholesterol levels, HbA1c and serum insulin. These results suggest 1000mgs vitamin C may be beneficial for patients with T2DM and reducing the risk of complication.158
A recent Cochrane review has concluded that there were no relevant clinical trials identified for the effective treatment diabetic eye disease with vitamin C and superoxide dismutase.159
Vitamin E
Vitamin E has been reported to be useful in preventing the long-term complications of diabetes through its synergistic antioxidant effect with vitamin C, improvement of insulin sensitivity and reduction of LDL cholesterol oxidation.160 Vitamin E also has been reported in an early study to reduce platelet aggregation and hence the risk of thrombosis.161
Vitamin D and calcium
Our best source of vitamin D is from direct sun exposure.
Vitamin D deficiency is common in T1 and T2DM has been shown to alter insulin synthesis and secretion in animal models of the disease, a result that has also been demonstrated in humans.53, 162
There is a significant body of biologically plausible evidence that strongly suggests that vitamin D plays a role in the prevention of T1DM and T2DM development and management.53, 163
Furthermore, a recent meta-analysis of the literature has noted an increased association between vitamin D and calcium deficiency and postulate combined supplementation with both nutrients may be beneficial in optimising glucose metabolism in both T1DM and T2DM.49, 164
Vitamin B1 thiamine
A recent randomised placebo-controlled pilot study has demonstrated that high dose thiamine supplementation may be beneficial for patients diagnosed with T2DM.165 This small pilot study compared a thiamine supplement administered at a dose of 300mg per day for 3 months to placebo. There was a 2-month washout follow-up. The primary endpoint was a change in urinary albumin excretion. Other markers of renal and vascular dysfunction and plasma concentrations of thiamine were also determined. The study concluded that high-dose thiamine therapy produced a regression of urinary albumin excretion in T2DM patients with microalbuminuria. Thiamine supplements at high dose could provide improved therapy for early-stage diabetic nephropathy. There was, however, no effects observed in glycaemic control, dyslipidaemia or blood pressure. There were no reported adverse effects due to thiamine therapy.165
Vitamin B3 nicotinic acid
A 16 week trial of 148 patients trialled on low dose extended nicotinic acid of 1000 milligrams and 1500md/day and when compared with placebo led to increases in HDL cholesterol by 19 and 24% and reduction in triglycerides by 13 and 28% respectively, with only a slight reduction of LDL cholesterol with the higher dose.166 Nicotinic acid may play a role in diabetics for lipid management. Only 1 subject withdrew from the trial due to flushing from nicotinic acid.
Vitamin K
Vitamin K may be potentially beneficial for insulin resistance. A trial assessing the role of vitamin K supplementation (500 μg/d of phylloquinone) on bone loss, also found that Vitamin K supplementation for 36 months at doses attainable in the diet may reduce progression of insulin resistance in older men, but not women.167
Vitamin B12
Whilst vegan diets may help in the prevention and management of T2DM, there is a risk of patients developing vitamin B12 deficiency especially those taking metformin which interferes with vitamin B12 absorption.168
The risk for vitamin B12 deficiency was accentuated with prolong metformin use or when used in higher doses. Patients on metformin should have their vitamin B12 levels checked annually. The situation is magnified in diabetics on vegan diets, coupled with metformin use needing to have their vitamin B12 levels carefully monitored.169
Multivitamin/mineral supplements
Elevated C–reactive protein levels have been associated with the risk of cardiovascular disease and T2DM. An analysis of the data from a randomised, double-blind, placebo-controlled study was carried out at the end of the trial and it was reported that multivitamin use was associated with lower C–reactive protein levels.172 Recently, it was demonstrated in an RCT that the effects of vitamins C and E, and also when in combination with magnesium and zinc, were a significant improvement of glomerular, but not tubular, renal function in T2DM patients.173 Furthermore, in randomised placebo-control trials after 3 months of using the combined multivitamin and mineral supplements, the treatment group had significant increased HDL cholesterol and apolipoproteins (apo) A1 enzyme levels, and reduced blood pressure in T2DM patients but no change in serum levels of total cholesterol, LDL cholesterol, triglyceride, and apo B levels. This suggests that the multivitamin and mineral supplements may have a favourable cardiovascular benefit by raising HDL levels and reducing blood pressure in T2DM. Supplementation with vitamin C and E and Zn when used alone did not show any benefit.174, 175
Other studies have not been able to demonstrate any benefit of antioxidants on fasting blood glucose levels in T2DM.176
Middle-aged and elderly patients with T2DM experienced a significant reduction of infections such as flu-like illnesses respiratory, gastrointestinal and urinary tract infections, and days off work (17% of diabetics) in those who took a daily multivitamin supplement compared with those who took placebo (90% of diabetics).177 Researchers postulated patients with diabetes were more likely to have suboptimal intake of micronutrients which would explain the positive effect.
Minerals
Chromium
Chromium has been the most widely studied supplement for diabetes as it is essential for the metabolism of glucose and blood lipids by the body. Low levels of chromium are associated with increased risk of T2DM.178
Numerous in vitro and in vivo studies suggest that chromium supplements, particularly niacin-bound chromium or chromium-nicotinate may be effective in attenuating insulin resistance and lowering plasma cholesterol levels.179 Chromium functions as a co-factor for insulin, regulating the activity of insulin. It has been reported that T2DM patients, who are chromium-deficient, are likely to benefit from chromium supplementation.180–189
A recent review has concluded that there was no significant effect of chromium on lipid or glucose metabolism observed in people without diabetes.190 However, chromium supplementation significantly improved glycaemia among patients with diabetes.190 A further review reported that there was greater bioavailability of chromium picolinate compared with other forms of chromium, such as niacin-bound or chromium trichloride. This may explain the comparative superior efficacy in glycemic and lipidemic control.191 The pooled data from the studies that were investigated that used chromium picolinate supplementation for T2DM patients demonstrated substantial reductions in hyperglycaemia and hyperinsulinemia, which then equates to a significant reduced risk for disease complications.191 Collectively, the data supported the safety and therapeutic value of chromium picolinate for the management of cholesterolemia and hyperglycaemia in those patients diagnosed with T2DM.191
Recent studies with selected populations presenting with insulin resistance have also reported significant benefits with chromium picolinate supplementation either alone or in combination with biotin.192–195 In 1 study it was reported that 1000 μg/day of chromium picolinate therapy improved insulin resistance in some HIV-positive patients, however, highlighting that extra caution was warranted in this population.192 Chromium in combination with biotin may have a beneficial effect on reducing atherosclerosis in patients with T2DM.196
Moreover, clinical trials suggest positive effects of chromium in T2DM patients with hypercholesterolaemia, with hypercholesterolemic patients (prescribed statins), moderately obese to obese T2DM patients (prescribed anti glycemic medications) benefited significantly from the combined use of chromium picolinate and biotin190, 194, 195, 196 as ascertained by improved blood lipid and glucose profiles.
There have also been negative findings of chromium on T2DM. A double-blind trial of chromium picolinate 800mcg/day showed no difference in impaired glucose tolerance progression compared with placebo197 and a systematic review of the literature found chromium had no effect on glucose or insulin concentrations in non-diabetics and was inconclusive for diabetics.198
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree