Dermatopathology
EMBRYOLOGY
From what embryologic tissue type is the epidermis derived?
Surface ectoderm
From what embryologic tissue type is the dermis derived?
Mesoderm—depending on location in the embryo dermis may be derived from dermatome, lateral somatic, or neural crest tissue
What is the embryologic origin of cutaneous melanocytes?
Neural crest mesoderm
ANATOMY/HISTOLOGY
What are the three layers of the skin?
- Epidermis
- Dermis
- Subcutaneous tissue
What types of epithelium is the epidermis?
Keratinized stratified squamous epithelium
What are the five layers of the epidermis?
- Stratum corneum
- Stratum lucidum
- Stratum granulosum
- Stratum spinosum
- Stratum basalis
What types of cells compose the stratum basalis?
Squamous cells which have a basophilic, cuboidal to columnar appearance distinct from the eosinophilic, mature-appearing squamous cells of the upper layers in the epidermis
What are the two layers of the dermis?
- Papillary layer
- Reticular layer
What are the small, encapsulated sensory receptors found in the dermis of the palms, soles, and digits of the skin (hint: they are also involved in light discriminatory touch of hairless skin)?
Meissner corpuscles
What is the name of tactile disks that mediate light crude touch?
Merkel corpuscles
What are the large encapsulated sensory receptors found in deeper layers of skin that are involved in pressure, coarse touch, vibration, and tension?
Pacinian corpuscles
Where else are Pacinian corpuscles found?
Joint capsules; serous membranes; mesenteries
What structure connects epidermal basal cells to the underlying extracellular matrix of the basement membrane?
Hemidesmosomes
What structures join adjacent squamous cells together and provide anchoring points for intermediate filaments?
Desmosomes (macula adherens)
What is the function of Langerhans cells?
Antigen-presenting cells; main inducers of antibody response
From where does the epidermis regrow after trauma or removal?
From epidermally derived hair follicles and sweat glands in the dermis
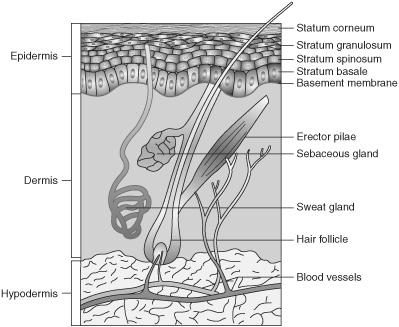
Figure 13.1 Skin layers.
PATHOLOGY
General Principles
What is a macule?
Flat, discolored (hypo- or hyper-pigmented) area of skin <1 cm in diameter
What is a patch?
Flat, discolored area of skin >1 cm in diameter
What is a papule?
Raised area of skin of any color that is <1 cm in diameter
What is a plaque?
Raised area of skin of any color that is >1 cm in diameter
What is a nodule?
A palpable, roughly round lesion arising in the dermis or subcutaneous tissues
What is a vesicle?
A raised, fluid-filled blister measuring <0.5 cm in diameter
What is a bulla?
A raised, fluid-filled blister measuring >0.5 cm in diameter
What is a pustule?
A blister that is filled with pus (generally bacteria and necrotic debris)
What is a wheal?
A “hive,” generally a round lesion resulting from edema in the dermis
What is the term for dilated, superficial blood vessels?
Telangiectasia
What are petechiae?
Nonblanchable pin-point foci of hemorrhage in the skin
What is purpura?
A larger area of hemorrhage in the skin, may be palpable
Which test is designed to ascertain whether a skin lesion will blanch as a result of pressure?
Diascopy
What is an erosion?
The skin lesion that results when all or part of the epidermis is removed (ie, abraded), will not leave a scar
Full-thickness loss of epidermis and loss of all or part of the epidermis, will leave a scar
Define hyperkeratosis:
Excessive keratin production leading to thickening of the stratum corneum
Define lichenification:
Visual appearance of thickened skin with prominent skin markings that occurs secondary to chronic scratching of itchy skin, can be associated with atopic dermatitis
Define ichthyosis:
Excessive cornification of the skin, giving it a scaly appearance
Define hypertrichosis:
Excessive hairiness due to increased formation of hair follicles, may be regional or generalized
What is meant when describing a rash as “annular”?
The rash has a ring-like, possibly targetoid appearance. Lesions may be singular or multiple.
What is meant when describing a rash as “herpetiform”?
That the rash is distributed as grouped papules or vesicles, similar to a herpes simplex rash, but does not necessarily indicate a specific etiology
What is meant when describing a rash as “zosteriform”?
That the rash is distributed as clustered papules or vesicles in a dermatomal distribution, similar to a herpes zoster rash, but does not necessarily indicate a specific etiology
What is meant when describing a rash as “morbilliform”?
That the rash appears as erythematous maculopapules, similar to a measles rash, but does not necessarily indicate a specific etiology
What is meant when describing a rash as having “flexor distribution”? Give examples of this type of rash.
Flexor distribution (aka intertriginous) means that the rash is distributed over the body primarily involving skin covering flexor muscle groups (ie, anterior arm including wrist and elbow crease, posterior legs including knee crease, and femoral crease). Examples include: atopic dermatitis and inverse psoriasis.
What is meant when describing a rash as having “extensor distribution”? Give a classic example of this type of rash.
Extensor distribution means that the rash is distributed over the body primarily involving skin covering extensor surface of limbs (ie, elbows, knees). Psoriasis is classically described as involving extensor surfaces.
What is meant when describing a rash as having a “photosensitive” distribution?
That the rash is distributed over the body in a distribution primarily involving sun-exposed skin while sparing areas covered by clothing or shaded by other body parts (ie, nose or chin)
What is meant when describing a rash as having an “acral” distribution?
That the rash is distributed over the body primarily involving distal portions of the limbs (ie, hands, feet) and head (ie, ears, nose)
Congenital/Inherited
What are nevi?
A nevus is any congenital lesion of the skin. Most often applied to melanocytic nevi (moles) which can be either congenital or acquired. Large congenital nevi (>20 cm) are associated with an increased risk of melanoma later in life.
What is a hemangioma?
The most common tumor of infancy, hemangiomas are benign vascular proliferations which can appear in the skin (most often on the face or scalp). Flat, larger lesions may be referred to as port-wine stains.
What are phakomatoses?
Phakomatoses are a family of neurocutaneous syndromes which have disorders of the central nervous system as well as the skin and retina. The five classic phakomatoses include: neurofibromatosis, tuberous sclerosis, ataxia telangiectasia, Sturge-Weber syndrome, and von Hippel-Lindau disease. Depending on the source, this group may also include incontinentia pigmenti and nevoid basal cell carcinoma syndrome.
What is the most common neurocutaneous disorder?
Neurofibromatosis
What are the multiple, light-brown, freckle-like lesions found in neurofibromatosis?
Café au lait spots
Café au lait spots usually grow along what structures?
Peripheral nerves
On what chromosome is the mutation associated with NF type I found?
Chromosome 17
What are other manifestations associated with NF type I?
Optic gliomas; bone abnormalities; freckling of the axillary or genital area
Hypopigmented macules or ash-leaf spots on the trunk or lower extremities are associated with what disease?
Tuberous sclerosis
What is the tuberous sclerosis triad?
Mental retardation; epilepsy; multiple angiofibromas
A unilateral port-wine stain of the forehead and upper eyelid is associated with what condition?
Sturge-Weber syndrome (encephalotrigeminal angiomatosis)
Which nerve is associated with Sturge-Weber syndrome?
Ophthalmic branch of the trigeminal nerve
How is alkaptonuria inherited?
Autosomal recessive inheritance
What accounts for the discoloration of the skin and urine in alkaptonuria?
Deposition of homogentisic acid
Hemochromatosis has what manifestation in the skin?
Hyperpigmented bronze skin
Which connective tissue disorder is associated with hyperextensible fragile skin, loose joints, and a tendency toward easy bruising and bleeding?
Ehlers-Danlos syndrome
What are possible life-threatening complications associated with Ehlers-Danlos disease?
Arterial or intestinal rupture
What is the name of the group of autosomal recessive diseases of premature aging?
Progeria
Marfan syndrome is due to a defect in which gene?
Fibrillin-1 (FBN1)
On which chromosome is the mutation associated with Marfan syndrome located?
15q21
What is the most common cause of death in a Marfan patient?
Ascending aortic dissection
How is albinism generally inherited?
Autosomal recessive inheritance
What is lacking in the epidermis of albino patients?
Melanin
What condition is associated with multiple neuromas on the eyelid, lips, distal tongue, and/or oral mucosa?
MEN, type 2B
Epidermolysis bullosa acquisita (EBA) is associated with which disease?
Inflammatory bowel disease, especially Crohn disease
What haplotype is frequently found in patients with EBA?
HLA-DR2
Which type of collagen is defective in osteogenesis imperfecta?
Type I collagen
Inflammatory/Autoimmune
Which rash often described as a target lesion that has a red center, pale zone, and a dark outer ring (targetoid)?
Erythema multiforme
What are the common causes of erythema multiforme?
Infections; antibiotics; radiation; chemicals; malignancy
What are the most common causes of nonscarring alopecia?
Telogen effluvium; androgenic alopecia; alopecia areata; tinea capitis; traumatic alopecia
What are the most common causes of scarring alopecia?
Cutaneous lupus; lichen planus; folliculitis planus; linear scleroderma
What is the treatment for rosacea?
Avoid precipitating factors; topical metronidazole; sulfur lotions; oral tetracyclines; isotretinoin
What condition has whitish-red nodules especially on digits and over joints, and is associated with uric acid accumulation?
Gout; the classic gouty tophus of the great toe is called podagra.
What is the most likely cause of xanthomas?
Hyperlipidemia
Sharply demarcated, silvery-white plaques on a patient’s elbows and knees (extensor surfaces) are most likely a manifestation of what disorder?
Psoriasis
What conditions can trigger psoriasis?
Trauma; infection; drugs
Which major histocompatibility markers are associated with psoriasis?
HLA-CW6; B13; B17; B27
What disorder has scaly, thickened plaques that develop in response to persistent rubbing of pruritic sites?
Lichen simplex chronicus
Which disease results from the deposition of collagen in skin that causes a “hardened” and “thickened” appearance and is associated with Raynaud phenomenon?
Scleroderma
What is scleroderma?
Also known as systemic sclerosis, scleroderma is a chronic disease characterized by accumulation of fibrous tissue in the skin and other organs. The etiology is unknown.
Which antibodies are associated with scleroderma?
Scl-70 (diffuse); anticentromere antibodies (localized)
What other conditions are associated with scleroderma?
Hypertension; gastrointestinal disease; pulmonary fibrosis; kidney disease
Which disease is associated with a rash on the face, particularly the malar areas?
Systemic lupus erythematosus (SLE)
Atopic dermatitis is associated with what conditions?
Asthma and allergic rhinitis. These three features together complete the “allergic triad.”
Which test is often helpful in the evaluation of patients with chronic contact dermatitis?
Patch test—small amounts of potential irritants are topically applied to the skin and evaluated over a period of 4 to 7 days for an inflammatory reaction.
What is the most common presentation of contact dermatitis?
Hand eczema, most likely due to occupational exposure
Contact dermatitis is what type of hypersensitivity reaction?
Type IV (delayed hypersensitivity)
What is Reiter syndrome?
Classified as a seronegative spondyloarthropathy, Reiter syndrome is a form of rheumatoid-factor negative arthritis classically associated with urethritis, conjunctivitis, and anterior uveitis.
Eruptive forms of what condition may be associated with Reiter syndrome?
Psoriasis
Which human leukocyte antigen (HLA) types are increased in frequency in patients with dermatitis herpetiformis?
HLA-B8; HLA-DR3; HLA-DQW2
Which rheumatologic disease is associated with a diffuse red rash of the trunk, periungual telangiectasis, proximal muscle weakness, myositis on muscle biopsy, and elevated creatine phosphokinase (CPK) and aldolase?
Dermatomyositis
What is vitiligo?
Partial or complete loss of melanocytes within the epidermis
Vitiligo is most commonly associated with what conditions?
Thyroid disease; pernicious anemia; Addison disease; diabetes mellitus type 1
What are some clinical manifestations of type I hypersensitivity reactions?
Anaphylaxis; urticaria; exanthema; angioedema
Urticaria is what type of hypersensitivity reaction?
Immunoglobin E (IgE)-mediated, type I hypersensitivity reaction
Autoantibodies to desmosomes and desmogleins, the intercellular junctions of epidermal cells, are found in which disease?
Pemphigus vulgaris
Pemphigus vulgaris is associated with which type of autoantibody?
IgG
What are the clinical findings of pemphigus vulgaris?
Patients with pemphigus vulgaris present with multiple, large, often open bullae involving the oral mucosa and skin, especially the scalp, face, axilla, groin, and trunk. They are at high risk of mortality due to secondary infection of open bullae.
Patients with pemphigus vulgaris have an increased incidence of which haplotypes?
HLA-DR4; HLA-DRw6
Touching normal-appearing skin with a sliding motion and having upper portions of the epidermis separate from the basal layer of the epidermis is what physical examination finding?
Nikolsky sign—and is positive (meaning that the layers separate) in pemphigus vulgaris
What are the clinical findings of bullous pemphigoid?
Patients with bullous pemphigoid present with multiple, variously sized, tense (unopened) bullae on erythematous skin distributed over inner thighs, flexor surfaces of the forearm, axillae, groin, and lower abdomen.
What do the autoantibodies in bullous pemphigoid target?
BP1 (bullous pemphigoid peptide 1) and BP2 (bullous pemphigoid peptide 2) in the basement membrane of the epidermis
Bullous pemphigoid is an autoimmune disorder that rarely affects which part of the body (in contrast to pemphigus vulgaris, which affects it frequently)?
Oral mucosa
Dermatitis herpetiformis is often associated with what condition?
Gluten-sensitive enteropathy (eg, Celiac disease)
Mantoux (PPD or TB) skin test, transplant rejection, and contact dermatitis are what type of hypersensitivity reaction?
Delayed hypersensitivity reaction, type IV
Infectious
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


