MEDICAL HISTORY
- Many conditions may be associated with skin disease:
- Autoimmune disease (lupus, dermatomyositis)
- Endocrinopathy (diabetes mellitus, thyroid disease)
- Hepatic dysfunction
- Genetic disorders (neurofibromatosis, Down syndrome)
- Immunosuppression (HIV/AIDS, transplant recipients)
- Malignancy
- Renal dysfunction
- Autoimmune disease (lupus, dermatomyositis)
- Systemic medications are a frequent cause of rash and other skin complaints. All oral medications (especially new medications and antibiotics, antihypertensives, and antiepileptics), herbal supplements, and topical medications should be noted.
- Family history of primary skin diseases such as psoriasis, eczema, and skin cancer should be noted. Family history of autoimmune disorders or allergies may also be important.
- Occupational exposures, living conditions, and sexual history can be contributory.
PHYSICAL EXAMINATION
- Examine the entire skin surface as well as the palms and soles, genitals, oropharynx, and eyes. If there is a concern for or history of melanoma, examine the neck, axillae, and groin for lymphadenopathy.
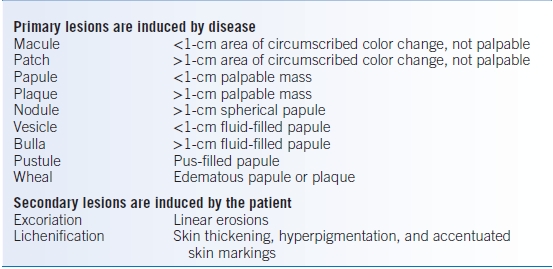
- If a lesion is identified, classify it (see Table 41-2).
TABLE 41-2 Classification of Lesions
Dermatologic Therapies
Skin disorders are characterized by pruritus, inflammation, alterations in hydration, and pain. Identification and treatment of specific underlying conditions should always be attempted.
DRY SKIN CARE
- Almost all itchy skin conditions are improved by the following regimen:
- Take short, cool baths or showers (<5 minutes).
- Use mild, nondrying soaps (e.g., Dove, Oil of Olay, or Cetaphil). Scrubbing or the use of washcloths and loofahs should be discouraged. Limiting the use of soap to the axilla and groin may be necessary.
- After bathing, pat dry and apply thick moisturizers such as petroleum jelly or other thick lubricants (e.g., Eucerin or Cetaphil creams). In general, ointments and creams are more effective than lotions. Patients may be instructed that moisturizers that come in a jar are generally more effective than those that come in a pump dispenser. Moisturizers should be applied while the skin is still damp and may be safely reapplied as often as needed.
WET SKIN CARE
Excessive moisture in intertriginous areas can lead to bacterial or yeast overgrowth and infection.
- Dry the affected area and apply powder or dry dressing of absorptive material. Use of a fan or hair dryer may be helpful prior to application of powder.
- Separate skin surfaces with absorptive materials.
ANTIPRURITICS
- Pruritus and burning can lead to uncontrolled scratching and can perpetuate an underlying condition.
- Topical agents can be used to control symptoms.
- Camphor 1% to 3% and menthol provide a cooling sensation and may be stored in the refrigerator.
- Phenol 0.25% to 2% causes local hypoesthesia but should not be used on raw or ulcerated skin.
- Topical anesthetics (benzocaine), antihistamines (diphenhydramine), and neomycin are best avoided because of a high rate of contact dermatitis.
- Camphor 1% to 3% and menthol provide a cooling sensation and may be stored in the refrigerator.
- Systemic antihistamines (H1 receptor antagonists) are most useful in the treatment of urticaria but are also helpful in other pruritic skin disorders. First-generation antihistamines (diphenhydramine, hydroxyzine) are particularly useful in the evening due to their sedative effect. Second-generation antihistamines (cetirizine, loratadine) may be easier to tolerate during the day as they are nonsedating.4
- Gabapentin and other neuroleptic medications have shown efficacy in neuropathic pruritus as well as idiopathic itch.5
PROTECTION
- Cotton and rubber gloves can be used to avoid excessive contact with water or chemical irritants. Cotton absorbs palmar sweat and should be cleaned or changed frequently.
- Barrier creams and ointments may prevent contact with irritating chemicals but are not substitutes for mechanical barriers.
TOPICAL STEROIDS
- Topical steroids are first-line therapy for many dermatologic conditions (Table 41-3). Topical steroids are effective, but can have significant side effects including skin atrophy, striae, acne, infection, and even suppression of the pituitary-adrenal axis.6 Side effects tend to occur with repeated application or application to the face, thin-skinned areas (neck, antecubital/popliteal fossae), or occluded areas (axillae, groin, inframammary folds). Patients should be reminded that a topical steroid should not be used as if it were a moisturizer. Topical steroids should be used on the affected areas of skin and never on normal skin.
- Several factors are important in determining the optimal steroid for a particular condition. Accurate diagnosis obviates the need for combination agents such as a weak azole antifungal and a high-strength topical steroid.
- Base or vehicle:
- Ointments are more lubricating as well as more occlusive, making them more potent. A lubricating ointment is best for dry dermatitis.
- Creams are less lubricating than ointments, but more so than gels, lotions, and solutions. A cream would be more appropriate for a weeping dermatitis. Creams are more likely than ointments to have additives that may irritate skin. If a patient complains of burning or stinging with a cream, it may be appropriate to switch to a comparable ointment.
- Lotions, gels, foams, and solutions are easier to use in hair-bearing areas and are most often used in dermatitis of the scalp. Gels may also be appropriate for the oropharynx.
- Ointments are more lubricating as well as more occlusive, making them more potent. A lubricating ointment is best for dry dermatitis.
- Strength:
- Higher-strength (classes 1 and 2) topical steroids are used for palmar/plantar areas or for severe or resistant lesions. They should never be used on the face.
- Midstrength (classes 3 through 5) topical steroids may be used on most parts of the body, but should generally be avoided on the face, genital areas, or skin folds.
- Lower-strength (classes 6 and 7) topical steroids may be safely used intermittently on the face.
- Higher-strength (classes 1 and 2) topical steroids are used for palmar/plantar areas or for severe or resistant lesions. They should never be used on the face.
- Dosage: Applications should generally be performed twice daily. When a cream or ointment is used, 1 g covers the face and 30 g covers the body of an adult (for 1 day).
- Occlusion: Occlusion with plastic wrap or gloves increases the potency of the steroid but should be reserved for severe, resistant lesions. A limited time course for occlusion should be specified. Occlusion increases both potency and risk of side effects.
TABLE 41-3 Topical Steroids
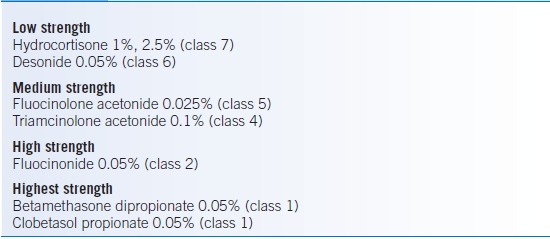
Note: Classes 6 and 7 are indicated for intermittent facial use. Classes 1 and 2 are indicated for palmar/plantar areas or severe/resistant lesions.
SKIN NEOPLASMS
Basal cell carcinoma (BCC) and squamous cell carcinoma (SCC) of the skin, which are sometimes grouped together as nonmelanoma skin cancer (NMSC), are the most common types of cancer diagnosed in the United States.7 Melanoma is much less common than NMSC, but the incidence of melanoma has been on the rise for several decades, especially among younger patients.8
SKIN CANCER PREVENTION
- Patients should be advised to avoid sun exposure between 10 am and 3 pm.
- Clothing (including hats and swimwear) with sun protection factor (SPF) can be purchased online and in many activewear stores.
- Sunscreens are useful adjuncts to long sleeves and wide-brimmed hats for fair-skinned people or patients with dermatoses induced by ultraviolet light. A daily moisturizer with broad-spectrum (ultraviolet A [UVA] and ultraviolet B [UVB]) coverage, preferably with at least SPF 30, is appropriate for most fair-skinned individuals.
- For certain light-sensitive disorders (e.g., systemic lupus erythematosus [SLE]) and photosensitizing drugs (e.g., tetracycline, sulfonamides, thiazides, quinolones), broad-spectrum sunscreens are necessary.
- All sunscreens should be applied 30 minutes before exposure and should be reapplied at least every 90 minutes and after bathing, swimming, or excessive sweating.
- Allergic and photosensitivity reactions occur to paraaminobenzoic acid, especially in patients who are sensitive to benzocaine, procaine, thiazides, and sulfonamides.
- Titanium dioxide and zinc oxide are opaque sunscreens that shield against UVA and UVB by providing a physical block. They are particularly useful on the nose and lips.
- For certain light-sensitive disorders (e.g., systemic lupus erythematosus [SLE]) and photosensitizing drugs (e.g., tetracycline, sulfonamides, thiazides, quinolones), broad-spectrum sunscreens are necessary.
- Patients should perform skin self-examinations monthly. Encourage patients to use the ABCDEs when examining their own skin. Lesions with the following traits are more likely to be malignant and should be evaluated by a physician.9
- Asymmetry: If a line is drawn through the lesion, the two sides do not match.
- Border: Irregular, notched, or scalloped borders are worrisome for melanoma.
- Colors: Melanoma may have different shades of brown, tan, or black within one lesion. Red, blue, and white areas may also be present.
- Diameter: A diameter of >6 mm is concerning for melanoma.
- Evolution: Any change in size, shape, color, or other characteristic is more likely to be present in a malignant lesion, and this factor is often the most significant of the five when considering the likelihood of malignancy. Development of pain, pruritus, or bleeding of the lesion is also concerning for skin cancer.
- Asymmetry: If a line is drawn through the lesion, the two sides do not match.
SEBORRHEIC KERATOSIS
- Seborrheic keratoses are hyperkeratotic epidermal papules commonly found in middle-aged and elderly patients.
- Seborrheic keratoses are benign skin neoplasms that can be confused with skin cancer. They have no malignant potential.
- On exam, they have a waxy, stuck-on appearance and may be tan, yellow, dark brown, or black in color. White horn cysts may be visible on close inspection. There is always a well-defined border. They usually appear on the face, chest, and back.
- Stucco keratoses are a variant consisting of small white papules on the lower legs.
- Dermatosis papulosa nigra is a form of seborrheic keratosis that appears as multiple small, darkly pigmented, possibly pedunculated papules on the cheeks and periorbital areas of Black, Hispanic, and Asian patients.
- If symptomatic, seborrheic keratoses may be removed using laser, cryosurgery (liquid nitrogen), curettage, or excision. Most seborrheic keratoses, however, do not require treatment or are treated for cosmetic reasons. If a clinician is not certain of the diagnosis, manipulation must be avoided as the differential of pigmented lesions includes melanoma.
ACROCHORDON
Also called acrochordons, skin tags are pedunculated skin-colored to brown papules commonly occurring on skin experiencing friction, specifically the neck, axillae, and groin. Treatment options for irritated or cosmetically troubling lesions include snipping with scissors and, less commonly, electrodessication or cryosurgery.
KERATINOUS CYST
Cysts on the skin present as firm subcutaneous nodules often with a central black punctum. They are freely mobile. Pilar cysts frequently occur on the scalp. Inflamed cysts may be treated with corticosteroid injection or, if necessary, incision and drainage. Once inflammation has subsided, definitive treatment consists of excision. The entire epithelial lining surrounding the cyst must be removed to prevent recurrence.
LIPOMA
Lipomas present as rubbery subcutaneous tumors. They are freely mobile. Lipomas are benign lesions. Treatment consists of excision, but is generally reserved for changing, symptomatic, or cosmetically undesirable lesions.
MELANOCYTIC NEVUS
- By definition, a melanocytic nevus is a benign skin neoplasm. Nevi are common growths and usually appear from birth through ages 35 to 40.
- Melanocytic nevi present as circumscribed papules or macules and may be flesh colored or darkly pigmented. They present on any area of the skin but often are concentrated in sun-exposed areas.
- Unlike melanoma, nevi are symmetric with well-defined borders and uniform color. They are usually <6 mm in diameter.
- Dysplastic nevi may have many of the characteristics of melanoma. Dysplastic nevi are controversial, but it is generally agreed that patients with a large number of nevi, particularly irregular or dysplastic nevi, are at higher risk for developing melanoma and should be examined more frequently.
SOLAR LENTIGO
Solar lentigines are benign pigmented lesions caused by chronic sun exposure. On examination, they appear as tan to dark brown macules often on the face and dorsal hands. Special attention should be paid to lesions that violate the ABCDEs as the differential includes lentiginous-type melanoma. Biopsy of the entire clinical lesion is preferred to avoid sampling bias.
CHERRY ANGIOMA
Cherry angiomas are benign collections of blood vessels appearing as round, red papules. No treatment is necessary unless lesions become irritated or bleed.
ACTINIC KERATOSIS
- Actinic keratosis (AK) is a premalignant lesion caused by chronic sun exposure. If left untreated, a small percentage of AKs may develop into SCC.10
- On examination, AKs appear as erythematous, raised papules with a firm scaly texture. On palpation, they have a sandpaper feel and are often easier to palpate than see.
- Typically, actinic keratoses are treated with cryosurgery. Other therapeutic options for patients with persistent or widespread lesions include curettage, topical 5-fluorouracil, topical imiquimod, or photodynamic therapy.
Basal Cell Carcinoma
GENERAL PRINCIPLES
- BCC is common and associated with chronic sun exposure. Fair-skinned individuals are at the highest risk.
- Patients with a history of one BCC have a 50% risk of developing a second primary within 5 years.11 There is a very low metastatic potential, but BCCs can cause significant local tissue destruction.
- Patients with a history of BCC should be examined every 6 to 12 months.
DIAGNOSIS
- BCC presents most commonly as a pearly, telangiectatic papule on the face or trunk.
- Superficial BCC may occur on the trunk and extremities and appear as a scaly plaque with raised borders. Ulceration is common.
- Diagnosis is made by shave or punch biopsy.
TREATMENT
- Surgical options include excision, electrodessication and curettage, or Mohs micrographic surgery if the BCC is located in a functionally or cosmetically sensitive area.
- Medical therapies include imiquimod and 5-fluorouracil for superficial BCCs.
- Radiation may be used to treat BCC in some instances when surgery is not an option.
- Vismodegib, a hedgehog inhibitor, has recently been approved by the FDA in the treatment of metastatic or locally advanced BCC.12
Squamous Cell Carcinoma
- SCC is caused by chronic sun exposure. SCC may also arise in chronic ulcers (Marjolin ulcer) or other chronic skin lesions.
- People with fair skin and a history of actinic keratoses are at higher risk of developing SCC. The risk of SCC is significantly increased in patients who are being treated with immunosuppressive medications, including patients with solid organ or allogeneic stem cell transplantation, inflammatory bowel disease, HIV, connective tissue disease, and myelodysplasia.13
- Patients with a history of one SCC are at higher risk of developing a second primary lesion. Metastasis is possible but uncommon, occurring in <5% of cases. Risk factors for metastasis include location (e.g., lips, ears, and genitalia), immunosuppression, and carcinomas arising from non-UV causes (e.g., long-standing discoid lupus or burns).14
- Patients with a history of SCC should be followed closely, and lymph node examination is recommended.
- SCC is characterized by a red scaly papule, plaque, or nodule, more commonly in a sun-exposed area. Lesions may have a verrucous appearance.
- Diagnosis is made by shave or punch biopsy.
- Surgical options include excision with at least 4-mm margins, Mohs micrographic surgery, or possibly electrodessication and curettage if histology is not aggressive.
Melanoma
GENERAL PRINCIPLES
- Melanoma can develop anywhere on the body. In Caucasian men, the back is the most common location, whereas in Caucasian women, the legs are most common.15 Melanomas occur more often on the palms, soles, and nail beds in Asians, Hispanics, and African Americans.
- People with a family history of melanoma are at increased risk for developing melanoma; however, most melanomas are diagnosed in patients with no family history of melanoma.
- Unlike BCC and SCC, melanoma has a high potential for metastasis.
- Patients with melanoma should be examined for lymphadenopathy. Sentinel node biopsy may also be performed for cancer staging.
DIAGNOSIS
- On examination, asymmetry, irregular borders, multiple colors, and a diameter >6 mm are worrisome signs for a malignant lesion.
- Excisional biopsy should be performed on any concerning or changing lesion. It is preferable not to sample a portion of the lesion but to provide the entire clinical lesion for pathologic examination, as the melanoma may be present in only a portion of the clinical lesion. Additionally, the tumor thickness (Breslow thickness), which provides important prognostic information, may be lost if only a portion of a lesion is removed.
TREATMENT
- Wide local excision is the definitive treatment for melanoma. Excisional margins and need for sentinel lymph node biopsy are based on the Breslow thickness of the lesion.
- The role of complete lymphadenectomy in the surgical treatment of patients with positive sentinel nodes remains controversial.
- Metastatic melanoma may be treated with immunotherapy (interferon, IL-2, ipilimumab, vaccine therapy), chemotherapy, and the recently introduced targeted agent, vemurafenib, but prognosis remains generally poor.16
DERMATITIDES
Contact Dermatitis
GENERAL PRINCIPLES
- Irritant contact dermatitis is a nonallergic reaction of the skin to chemical or physical agents. Mild irritants require repeated or prolonged contact to cause dermatitis (e.g., soaps, detergents, and solvents). Strong irritants can cause dermatitis following a single exposure (e.g., strong acids or alkali).
- Allergic contact dermatitis is a form of delayed hypersensitivity (type IV reaction) that develops only in previously sensitized individuals. The distribution and pattern of the dermatitis may suggest a specific allergen. Patch testing may be necessary to identify the offending allergen. Common allergens include the following:
- Plants (e.g., Rhus dermatitis, otherwise known as poison ivy, oak, and sumac): characterized by linear, vesicular lesions
- Metals (e.g., nickel, chrome): commonly diagnosed on skin that touches jewelry and fasteners, especially the earlobes and the periumbilical area
- Rubber/latex: affects skin in contact with gloves, condoms, and elastic
- Topical medications: specifically neomycin, benzocaine, additives in creams, and other vehicles
- Cosmetics: preservatives in makeup, perfume, and hair dye
- Plants (e.g., Rhus dermatitis, otherwise known as poison ivy, oak, and sumac): characterized by linear, vesicular lesions
DIAGNOSIS
- Acute dermatitis is characterized by erythema, weeping/oozing, crusting, and vesiculation. Poison ivy often produces linear vesicles. Severe lesions may demonstrate edema, ulceration, and large bullae.
- Chronic dermatitis is characterized by scale, dryness, and eventually thickening and hyperlinearity (lichenification) of the skin.
- The diagnosis is made largely by history of exposure to irritants or allergens.
- Skin examination may reveal a particular pattern associated with a type of dermatitis.
TREATMENT
- Mild dermatitis is treated with topical steroids, topical or systemic antipruritics, and avoidance of the offending agent.
- Severe blistering reactions are treated with oral prednisone, 0.5 to 1 mg/kg tapered over 14 to 21 days; antipruritics; and drying agents.
Atopic Dermatitis (Eczema)
- In contrast to contact dermatitis, atopic dermatitis is not caused by a specific irritant or allergen, although irritants and allergens can exacerbate eczema.
- Atopic dermatitis presents as erythematous, scaly plaques that may demonstrate lichenification and pigment alteration (hyper- or hypopigmentation).
- Dyshidrotic eczema is characterized by vesiculation. Scratching or rubbing worsens the condition.
- Commonly affected areas include skin flexures, hands, and feet.
- Effective therapy includes emollients, dry skin care, topical steroids, and antihistamines for reduction of pruritus. Choice of topical steroid depends on the location and severity of the lesion as well as the age of the patient.
- Recalcitrant cases may be treated with UV light therapy or immunosuppressants.
- Superinfection is common and should be treated with antibiotics targeting staph and strep.
Stasis Dermatitis
Stasis dermatitis is characterized by bilateral erythema, hyperpigmentation, and scaling that is most prominent on the lower legs. It may be mistaken for cellulitis, which is almost always unilateral. Successful treatment of stasis dermatitis requires reduction of lower extremity edema with compression stockings. Triamcinolone 0.1% ointment applied bid is an appropriate topical steroid.
Keratosis Pilaris
Keratosis pilaris is a common chronic papular eruption that occurs on the proximal extensor surfaces of the extremities and cheeks throughout life. The rash is characterized by scaly follicular papules and is usually asymptomatic. Treatment is often unsatisfactory and includes emollients, keratolytics, and topical retinoids.
Seborrheic Dermatitis
- Seborrheic dermatitis is a very common, usually mild dermatitis in adults. However, it can be quite severe in patients with HIV or Parkinson disease.17
- In adults, erythema with fine white or greasy scale is seen on the scalp (dandruff), eyebrows, eyelids, nasolabial folds, ears, sternal area, axillae, inframammary folds, and perineum.
- Antiseborrheic shampoos, such as selenium sulfide, zinc pyrithione, tar, or 2% ketoconazole are used at least every other day for 10 to 15 minutes. For the face or trunk, ketoconazole cream or 1% to 2.5% hydrocortisone cream bid is used.
Psoriasis
GENERAL PRINCIPLES
- Psoriasis is a chronic recurring condition with varying degrees of severity. While some patients suffer from widespread disease, others may have only a few small patches of involvement. Psoriatic arthritis involves the joints and may cause significant disfigurement and disability. Ten to twenty percent of patients with psoriasis will develop psoriatic arthritis.
- Psoriasis has been associated with high rates of cardiovascular disease.18
- Psoriasis is frequently associated with significant emotional distress and depression.19
- Stress, smoking, alcohol consumption, and certain medications (e.g., lithium, beta-blockers) can aggravate the disease. There may also be severe worsening of psoriasis after treatment with systemic steroids, and for this reason, systemic steroids should not be used to treat psoriasis.
DIAGNOSIS
- Examination reveals erythematous plaques with silvery scale on the elbows, knees, scalp, and trunk. Nail changes including pitting and “oil spots” may also be present. Psoriasis can progress to generalized erythroderma (psoriasis involving >90% body surface area [BSA]).
- Guttate (“drop-like”) psoriasis is characterized by small, erythematous papules on the trunk and may be associated with streptococcal pharyngitis.
TREATMENT
- Mild-to-moderate psoriasis is treated topically with topical steroids, vitamin D3 analogs (calcipotriene), retinoids (tazarotene), tar derivatives, natural sunlight, or narrow-band UVB radiation. Calcipotriene and tazarotene are more expensive than topical steroids but less likely to cause skin atrophy. Calcipotriene can cause hypercalcemia if it is used on >10% of the body. Tazarotene can cause burning, erythema, and desquamation. Sunlight and UVB radiation can cause burning and increase the long-term risk of skin cancer.
- Severe psoriasis (>30% BSA) may require phototherapy or systemic agents (e.g., methotrexate, acitretin, cyclosporine, etanercept, adalimumab, infliximab, ustekinumab). These therapies must be closely monitored. Some biologic agents increase the risk of infection, especially reactivation of tuberculosis. Tuberculosis tests (purified protein derivative [PPD] or interferon-gamma release assay) must be checked yearly. Systemic therapies are for patients who are incapacitated by their disease and resistant to less toxic forms of treatment. They are the only therapies effective for psoriatic arthritis.
- Scalp psoriasis is treated topically with tar shampoo and steroid solutions. Prominent scale must be removed before topical treatments will work.
- Guttate psoriasis may respond to penicillin or amoxicillin if there is an underlying streptococcal infection. Phototherapy is also particularly effective for guttate psoriasis.
- Inverse psoriasis affects the axillae, inframammary folds, and groin. Topical steroids, often in combination with topical antifungals, are appropriate for these locations.
Pityriasis Rosea
- Pityriasis rosea is characterized by pink, oval papules with minimal peripheral scale. The papules align parallel to lines of skin cleavage, often resulting in a Christmas tree distribution on the trunk. The herald patch is a larger pink plaque that precedes the more diffuse rash.
- Pityriasis rosea may be mildly pruritic and is self-limiting, usually resolving in 6 to 12 weeks.
- Treatment is often frustrating, but sunlight, phototherapy, topical steroids, erythromycin, and antipruritics have all been reported to be effective.
- The rash of secondary syphilis can closely mimic pityriasis rosea. If there is any clinical suspicion, serologic testing for syphilis should be pursued.
Lichen Planus
- Lichen planus is characterized by pruritic, purple, polygonal papules that favor the volar wrists, ankles, and genitals. Lesions have lacy white scale (Wickham striae). Oral lesions are common and appear as lacy white plaques or erosions, often on the buccal mucosa.
- Lichen planus has been associated with chronic hepatitis, particularly in populations with a high incidence of hepatitis C.20 Lichen planus may also be induced by systemic medications, most commonly ACE inhibitors and thiazide diuretics.
- Treatment is with topical steroids, emolliation, and antipruritics. Severe, generalized cases may require oral prednisone or phototherapy.
Thermal Burns
- Dermatitis of varying intensity may be caused by excessive heat on the skin.
- First-degree burns congest superficial blood vessels, causing erythema that may be followed by desquamation (e.g., sunburn). Treatment includes prompt cold application and emolliation.
- Second-degree burns cause edema, vesicles, and severe pain. Treatment includes prompt cold application and emolliation. Vesicles should not be opened unless they are tense and painful. When required, drainage under aseptic technique is recommended.
- Third-degree burns cause full-thickness necrosis of the skin and anesthesia. Severe second- and third-degree burns benefit from specialized teams of physicians.
ACNE
Acne Vulgaris
GENERAL PRINCIPLES
- Acne vulgaris often develops around puberty and persists long into adulthood.
- Acne is an inflammatory condition with an infectious component and is characterized by open comedones (blackheads) and closed comedones (whiteheads).
- Treatments require at least 2 months of regular use to show significant improvement. Therapies should be continued for at least this long before changing treatment course.
- Acne may be improved by the use of oral contraceptives (OCPs) but is often worsened by medroxyprogesterone (Depo-Provera).
- Inflammatory acne is characterized by erythematous papules and pustules.
- Nodulocystic acne is characterized by larger nodules and results in scarring and should be treated aggressively.
TREATMENT
- Comedolytics are the first-line therapy for acne.
- Benzoyl peroxide, 2.5%, 5%, or 10%, is available as a wash or gel. Higher concentrations and gels may be used in patients with oily skin. Unlike topical antibiotics, benzoyl peroxide does not promote antibiotic resistance. Patients should be warned that benzoyl peroxide bleaches clothes.
- Topical retinoids (tretinoin, adapalene, tazarotene) are available in creams and gels. They should be used in small quantities (a pea-sized amount covers the entire face) on clean, dry skin. Higher-concentration creams and gels can be drying and can predispose to photosensitivity. Less frequent application may be necessary if irritation is significant.
- Benzoyl peroxide, 2.5%, 5%, or 10%, is available as a wash or gel. Higher concentrations and gels may be used in patients with oily skin. Unlike topical antibiotics, benzoyl peroxide does not promote antibiotic resistance. Patients should be warned that benzoyl peroxide bleaches clothes.
- Topical antibiotics can be used in inflammatory acne and are most helpful when used in combination with benzoyl peroxide or a topical retinoid.
- Clindamycin solution, lotion, or pledget one to two times daily
- Erythromycin solution or pledget one to two times daily
- Clindamycin solution, lotion, or pledget one to two times daily
- Systemic antibiotics

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


