(1)
Department of Histopathology and Cytology, Royal Hallamshire Hospital, Sheffield, UK
Abstract
In this chapter the appearance of neoplasms of the cervix other than glandular neoplasms as seen in cervical cytology preparations will be described.
Keywords
Neuroendocrine tumoursTransitional cell tumoursSoft tissue tumoursCarcinosarcomaLymphomaMalignant melanomaMetastatic tumoursIntroduction
All the neoplasms of the cervix described in this tumour are uncommon and consequently description of their appearances in cervical cytology preparations is limited in the vast majority to individual case reports or small series. In addition in view of the relatively recent introduction of liquid-based cytology in cervical screening programmes the experience of the cytological appearances of these neoplasms is greater with conventional Papanicolaou cervical smears.
Neuroendocrine Neoplasms
As described in Chap. 6, the WHO classification of neuroendocrine neoplasms of the cervix is identical to the classification employed for pulmonary neuroendocrine neoplasms and varies from a well-differentiated tumour composed of small regular cells with a trabecular or solid streaming pattern typical of a carcinoid tumour, to a small cell carcinoma characterised by the presence of a monotonous population of small cells with scanty cytoplasm, ovoid or slightly spindled hyperchromatic nuclei, often exhibiting moulding, abundant mitotic and apoptotic activity, and in some cases, extensive crush artefact, nuclear fragmentation and necrosis [1].
The appearances in cervical cytology samples reflect the range of histological appearances.
In well-differentiated neuroendocrine neoplasms of the cervix (carcinoid tumour), the cells are usually in nests with round to oval mildly pleomorphic nuclei containing small punctate reddish nucleoli and finely granular chromatin. Cytoplasm is scanty and eosinophilic or basophilic and the cytoplasmic borders ill-defined (Fig. 7.1) [2].
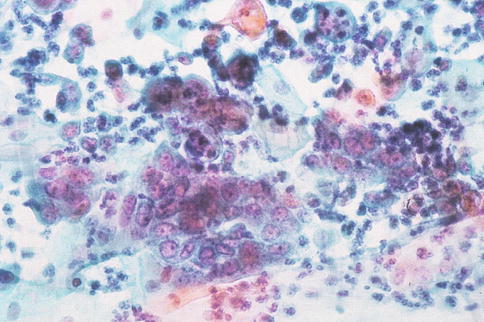
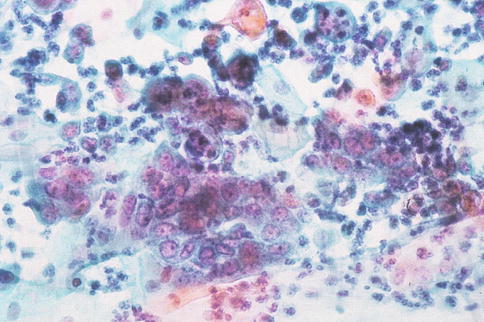
Fig. 7.1
Well differentiated neuroendocrine tumour in a conventional cervical smear showing a cohesive group of crowded cells with hyperchromatic nuclei and well-defined nucleoli (From Smith [55] with permission)
Small cell neuroendocrine carcinoma (poorly differentiated neuroendocrine tumour) is characterised by sheet like clusters or dispersed small cells with finely granular chromatin, scant cytoplasm and absent nucleoli [3–5]. Nuclear moulding is typically present in conventional cervical smears of small cell neuroendocrine carcinoma but may not be conspicuous in liquid based cytology preparations (Fig. 7.2) [5, 6]. Cytological preparations from large cell neuroendocrine carcinoma are composed of large cells with relatively abundant or absent cytoplasm, coarse chromatin and prominent nucleoli. Mitoses may be frequent and smears may show palisading, moulding and abortive rosette formation [4, 7, 8]. A solitary case of neuroendocrine carcinoma of the cervix with psammoma body formation has also been reported [9].
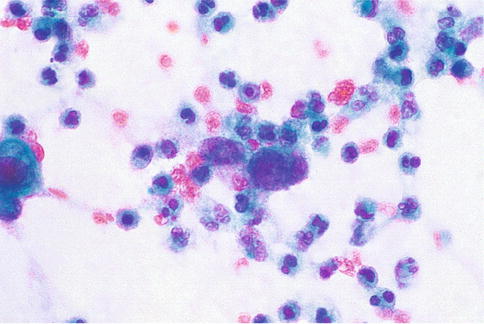
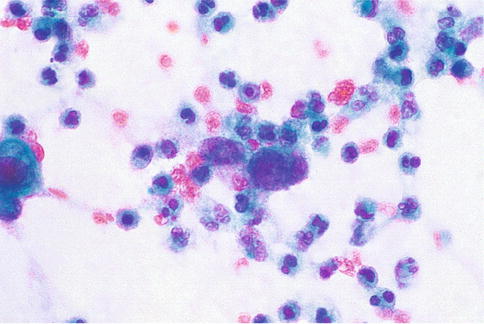
Fig. 7.2
Poorly differentiated neuroendocrine tumour in a conventional cervical smear showing marked tumour diathesis and a few small clusters of malignant cells with scanty cytoplasm and coarse granular hyperchromatic nuclei (From Smith [55] with permission)
The differential diagnosis of neuroendocrine neoplasms in cervical cytology preparations includes poorly-differentiated squamous carcinoma, adenocarcinoma or lymphoma and neuroendocrine neoplasms may coexist with the former epithelial neoplasms. If the sample contains two cell populations, because a squamous or glandular component is present, confusion with an adenosquamous carcinoma can arise or the neuroendocrine component may be completely overlooked. If small carcinoma cells are identified in a cervical cytology preparation, the possibility of metastasis from a pulmonary small cell carcinoma should be considered although metastases to the cervix are usually within the stroma and covered by intact mucosa, at least in the early stages; an appropriate history of lung tumour should be sought. It should also be noted that sparse cells from a small cell neoplasm of the cervix, whether of squamous or neuroendocrine type, are a well recognised cause of false negative cervical cytology reports [10, 11].
Transitional Neoplasms
The cytological features of six cases of papillary transitional cell carcinoma (squamotransitional cell carcinoma) of the cervix in conventional cervical smears, and nine cases in liquid-based cytology preparations have been described [12, 13].
In conventional cervical smears tumour cells with transitional features form cohesive groups in a multilayered fashion and have an oval or spindle shape with tapered ends. The nuclei are hyperchromatic, frequently display a wrinkled membrane, and have coarse and medium-sized granules, small or absent nucleoli, nuclear grooves and rarely pseudoinclusions. In all cases other cells with cytological appearances characteristic of squamous cell carcinoma were present and the background was necrotic or hemorrhagic [12].
Liquid-based cytology preparations of cervical transitional cell carcinoma often display moderate to high cellularity and contain three-dimensional, arborising, papillary clusters of basal or parabasal-like cells in which fibrovascular cores may sometimes be identified and basaloid cells are aligned horizontally at the epithelial surface. At high-power the appearance of the tumour cells ranges from bland-looking to high grade squamous intraepithelial lesions (high-grade dyskaryosis) and occasionally squamous cell carcinoma. Mitotic figures are commonly identified and tumour diathesis and dyskeratotic cells may be observed [13].
Mesenchymal Tumours
Smooth Muscle Neoplasms
Approximately 8 % of uterine leiomyomas (fibroids) occur in the cervix, making these the commonest benign mesenchymal neoplasms at this site. They are usually solitary. Although, if the overlying mucosa is ulcerated benign smooth muscle cells from the lesion may be present in cervical cytology samples, it has not been reported.
Embryonal Rhabdomyosarcoma
The cervix is very rarely the primary site of this aggressive tumour which typically presents in the reproductive years as a polypoid mass developing beneath the cervical surface epithelium associated with vaginal discharge.
The cytological features in a touch smear preparation of a case have been described by Matsuura et al. and consist of loose clusters of short spindle-shaped cells with elongated, scanty cytoplasm, and indistinct cell borders associated with tumour diathesis. The tumour cell nuclei are elongated or oval with a thin nuclear membrane, variable but usually fine chromatin and tend to have macronucleoli which are partly clear. The degree of cellular atypia ranges from mild to severe. Cross striations are rarely identified and without immunocytochemistry to confirm rhabdomyoblastic differentiation, distinction from other malignant mesenchymal neoplasms is difficult [14].
Myofibroblastoma
Other Mesenchymal Neoplasms
Other benign mesenchymal tumours of the cervix, namely haemangioma, schwannoma, neurofibroma, and lipoma are rare and the cytological findings have not to date been documented in conventional or liquid-based cervical cytology preparations.
Primary malignant mesenchymal neoplasms of the cervix are very rare; the most frequently encountered being leiomyosarcoma. Positive cervical cytology is rarely found in association with these tumours and even when abnormal cells are present it may not be possible to give a specific diagnosis. Cytological features suggestive of leiomyosarcoma are the finding of cell clusters or isolated neoplastic cells with oval to elongated, blunt ended nuclei showing fine granular chromatin with small nucleoli and delicate wispy cytoplasm. Stromal sarcoma of the cervix is usually a manifestation of direct spread from an endometrial stromal sarcoma. Features suggestive of endometrial stromal sarcoma are moderate or markedly cellular preparations composed of a mixture of single cells or stromal fragments in which small blood vessels may be identified. The individual tumour cells are spindle-shaped or epithelioid with minimal anisonucleosis and anisocytosis, fine granular chromatin with indistinct nucleoli, and scant to moderate delicate, amphophilic cytoplasm. The background usually includes blood and necrotic debris [18–20].
Mixed Epithelial and Mesenchymal Neoplasms
Carcinosarcoma (Malignant Mixed Mullerian Tumour)
This tumour is now generally accepted to be a metaplastic carcinoma [21]. In the majority of cases, carcinosarcoma of the cervix represents spread of tumour from the endometrium: in a series of 202 patients with cervical involvement by this tumour only one case was shown to be a primary cervical neoplasm [22].
The detection rate of malignant cells in cervical cytology preparations from histologically proven carcinosarcoma varies between 56 and 70 %. Most reports and series relate to tumours arising in the body of the uterus rather than the cervix. The histological blend of variable proportions of malignant neoplastic epithelial and stromal tissue, including in some cases heterologous elements showing rhabdomyoblastic or chondrosarcomatous differentiation, with undifferentiated small cells and spindle cells may be reflected in the cytological appearance in cervical cytology preparations, although the mesenchymal component is less commonly represented even in tumours with a predominant sarcomatous component, possibly because the latter does not readily exfoliate [23–25]. In a recent series of histologically proven uterine carcinosarcoma, 75 % of SurePath liquid-based cervical samples were originally reported as adenocarcinoma of possible endometrial origin. The cellular arrangement of the neoplastic epithelial cells is similar in conventional smears and liquid-based cytology samples and consists of neoplastic glandular cells in three-dimensional ball-like clusters, irregular clusters, and cohesive clusters or as dispersed individual cells. Tiny clusters of atypical glandular cells are easily overlooked in atrophic samples. Spindle-shaped malignant cells represent the sarcomatous component and these may show pleomorphism and multinucleation but more often resemble fibroblasts or fibroconnective tissue. The differential diagnosis of the sarcomatous component includes a spindle cell component of cervical squamous cell carcinoma. Heterologous elements are rare and are difficult to recognize with certainty in cervical cytology preparations (Fig. 7.3) [26].
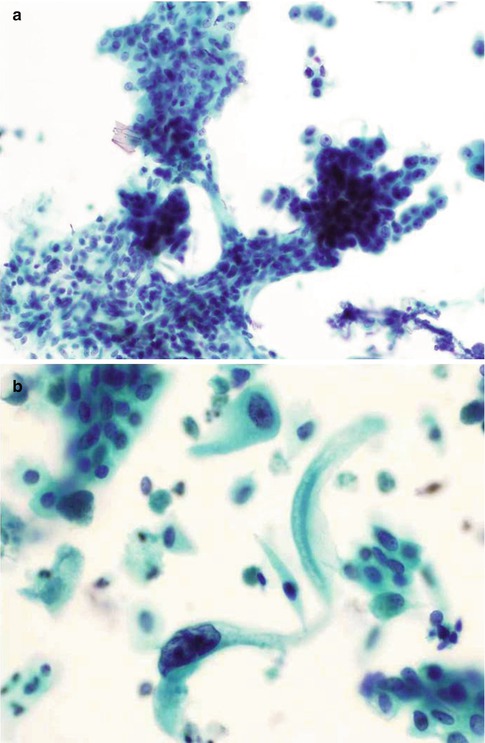
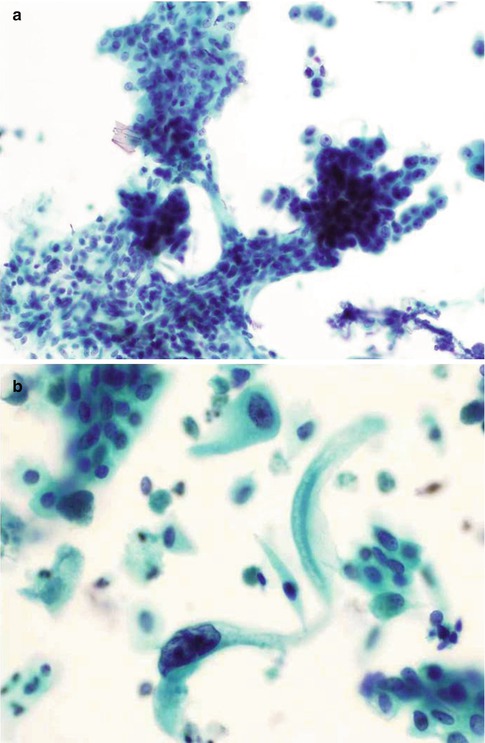
Fig. 7.3
Carcinosarcoma in a SurePath liquid-based cervical cytology sample. Three dimensional clusters of malignant epithelial cells associated with atypical spindle-shaped stromal cells (a) and an elongated malignant stromal cell with a malignant epithelial cell on an atrophic background (b) (From Gupta et al. [26]. With permission of Wiley Periodicals Inc)
Adenofibroma and Adenosarcoma
To date there have been no specific reports of the cytological appearance of adenofibroma or adenosarcoma in cervical cytology preparations.
Adenomyoma and Atypical Adenomyoma
Adenomyomas and polypoid adenomyomas of the cervix are rare. They comprise a mixture of benign endocervical glands and stroma composed predominantly of smooth muscle.
Atypical polypoid adenomyoma also rarely arises in the cervix. The glandular component in this entity is indistinguishable from endometrial intraepithelial neoplasia and there are usually conspicuous squamous morules.
The cytological features of both typical and atypical polypoid adenomyoma have been described in conventional and liquid-based cervical cytology preparations. In both cases cervical smears contained spindle-shaped smooth muscle cells, which in conventional smears may present as cohesive fragments with frayed edges revealing spindle cells with bipolar cytoplasmic processes, but whilst in the case of polypoid adenomyoma there were sheets and strips of reactive endocervical cells in an inflammatory background, in the case of atypical polypoid adenomyoma there were tightly packed, crowded clusters of atypical glandular cells [27–29].
Lymphoma, Leukaemia and Myeloma
Primary non-Hodgkin’s lymphoma of the cervix is a rare but well-documented event with over 60 cases described in the world literature; it is usually of diffuse large B cell type and presents in middle-aged or elderly women with vaginal bleeding and a cervical tumour mass, which is then biopsied [30]. The finding of lymphoma or leukaemia in the cervix is more commonly a manifestation of secondary involvement of the female genital tract and has been observed in up to 40 % of cases with widely disseminated disease [31, 32]. Advanced Hodgkin’s disease also may involve the cervix.
The cytological features of lymphoma of the cervix have largely been limited to single case reports, although a few small series have been reported. It is very rare for a cervical cytology sample to reveal abnormal lymphoid cells and such samples are typically normal or only show non-specific inflammation if the neoplastic cells are covered by intact mucosa; in the few reported cases with abnormal preceding cervical cytology samples, the abnormal cells have usually been interpreted as epithelial [30, 33–35]. There are also solitary case reports of cervical lymphoma in association with CIN 3 [36]. Lymphomatous cells on a cervical cytology sample must be distinguished from chronic inflammatory cells, small cell carcinoma, small cell severe dyskaryosis, endometrial carcinoma, poorly-differentiated adenocarcinoma, and sarcoma. Features favouring the diagnosis of lymphoma include single dissociated cells with prominent nucleoli, nipple-like projections on the nuclei, chromatin clumping at the nuclear borders and scant cytoplasm. Small cell carcinoma cells tend to be irregularly shaped and pleomorphic with indistinct nucleoli. Characteristic nuclear moulding and clustering may be present. Cells of small cell severe dyskaryosis may present in sheets as well as singly and individual cells may show evidence of keratinisation.
Subtyping of lymphomas in conventional cervical smears is not reliable but liquid-based preparations offer the possibility of immunocytochemical evaluation of the abnormal cells for phenotyping and accurate classification.
Reactive inflammatory cells will have a polymorphic appearance, being composed of a mixture of normal mature and immature lymphocytes, sometimes including plasma cells.
Myeloma rarely affects the female genital tract [37]. Atypical plasma cells have been described in the smear from a woman with postmenopausal bleeding in whom the diagnosis of myeloma had yet to be made. Myeloma cells appeared as large single cells with scant or deeply basophilic cytoplasm, hyperchromatic eccentric nuclei, some of which were multinucleate and had prominent large irregular nucleoli [38].
Melanocytic Neoplasms
Both benign and malignant melanocytic neoplasms occur in the cervix, of which blue naevus and malignant melanoma are the most common respectively.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


