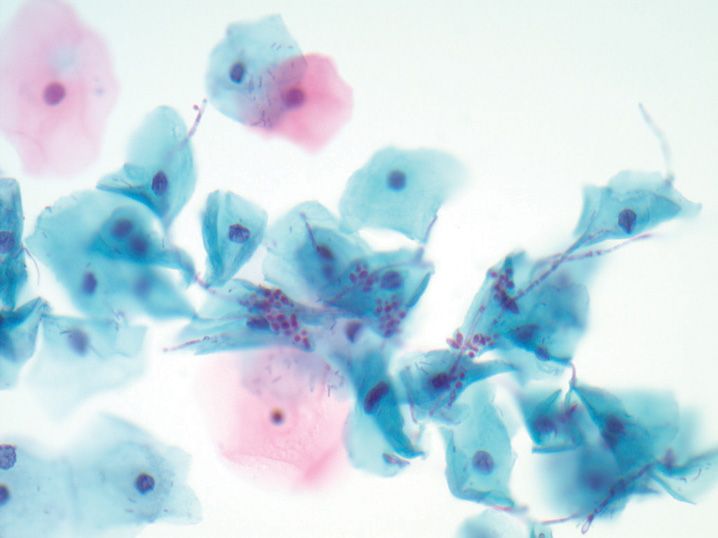
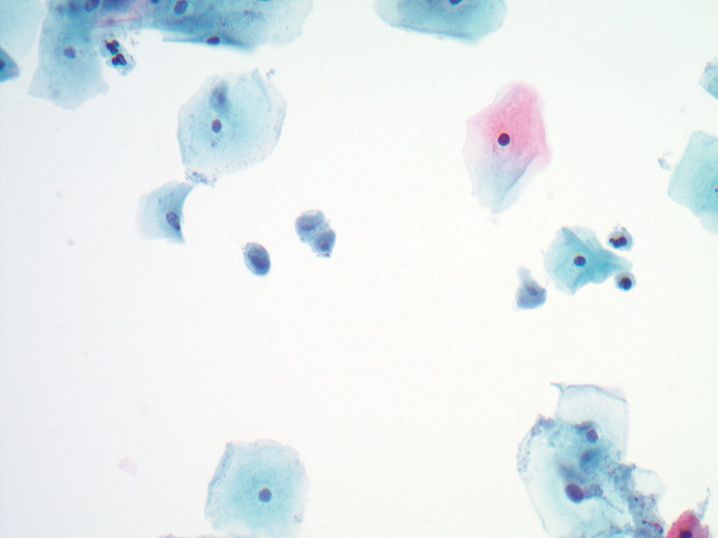
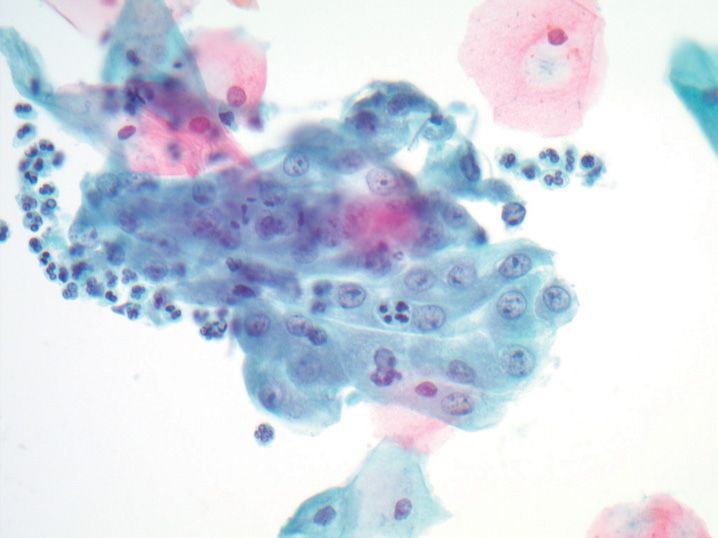
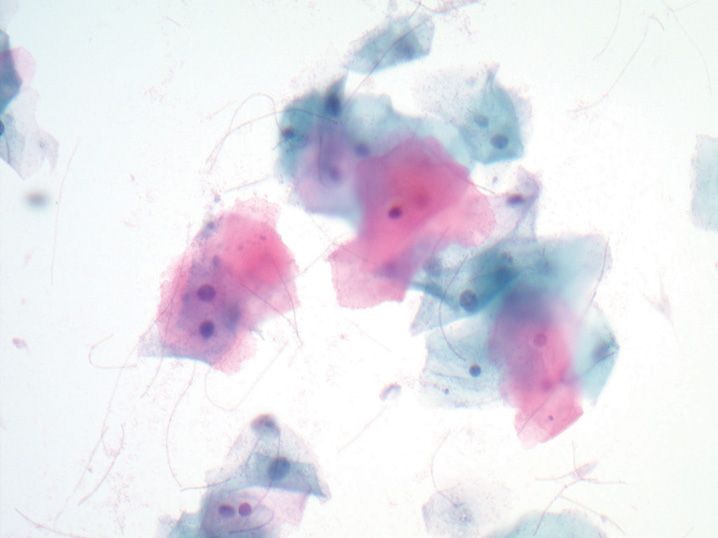
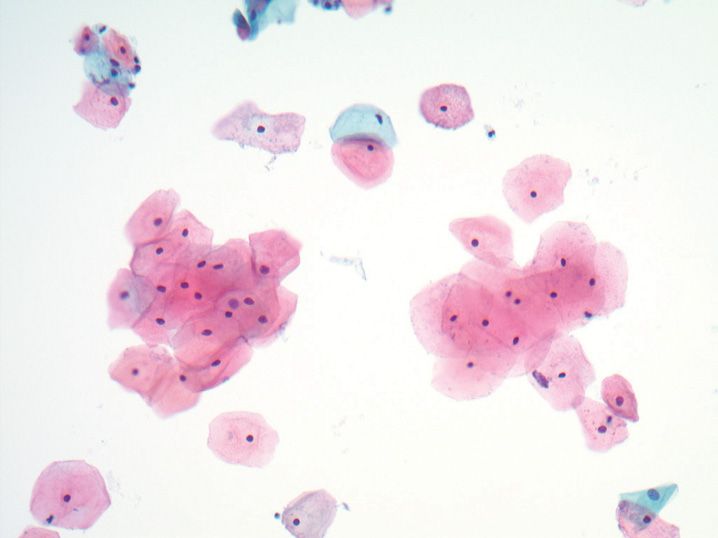
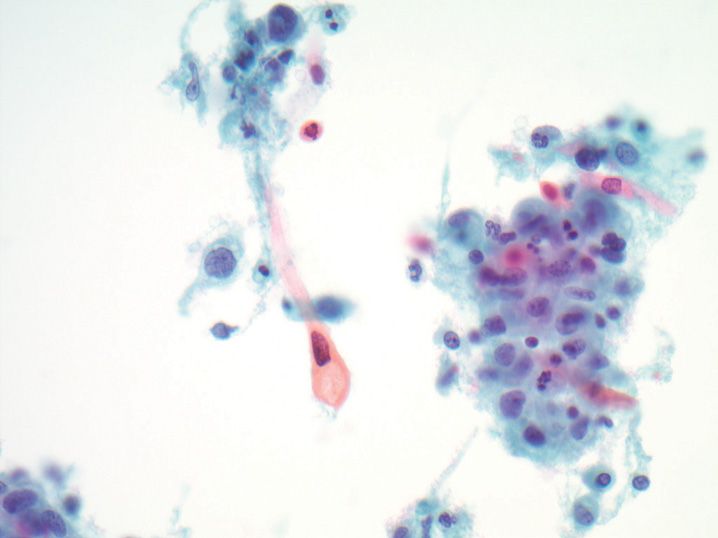
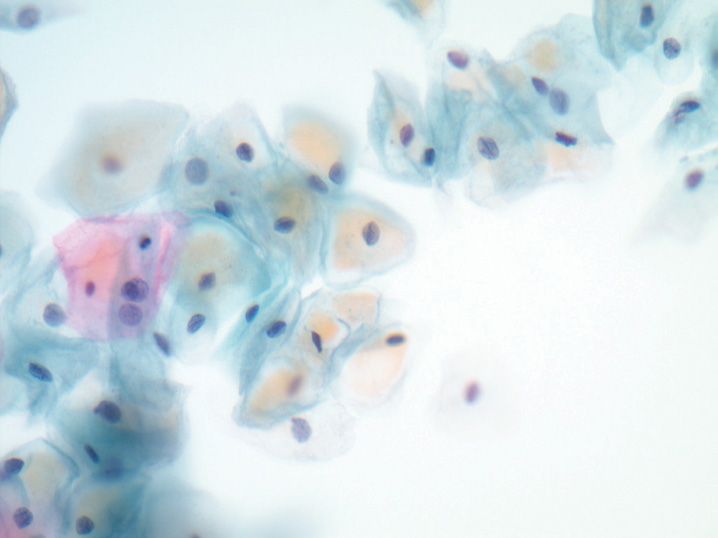
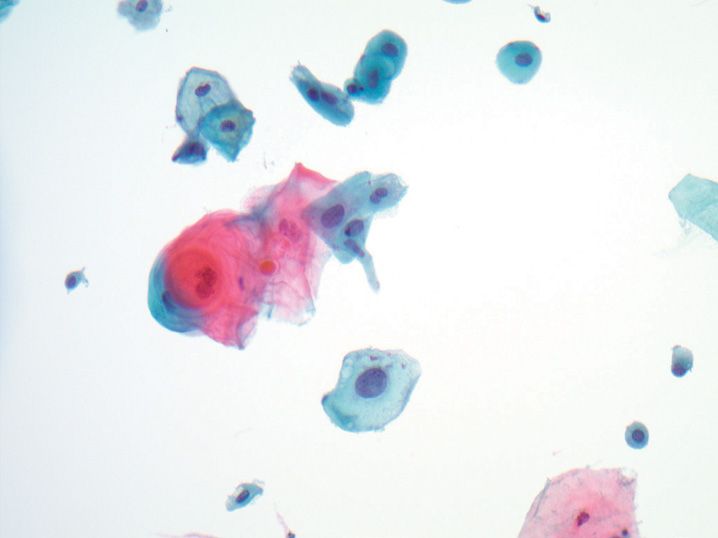
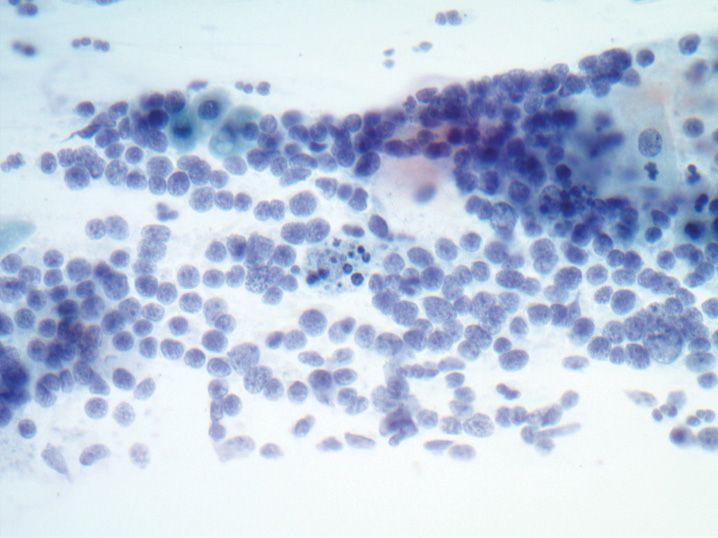
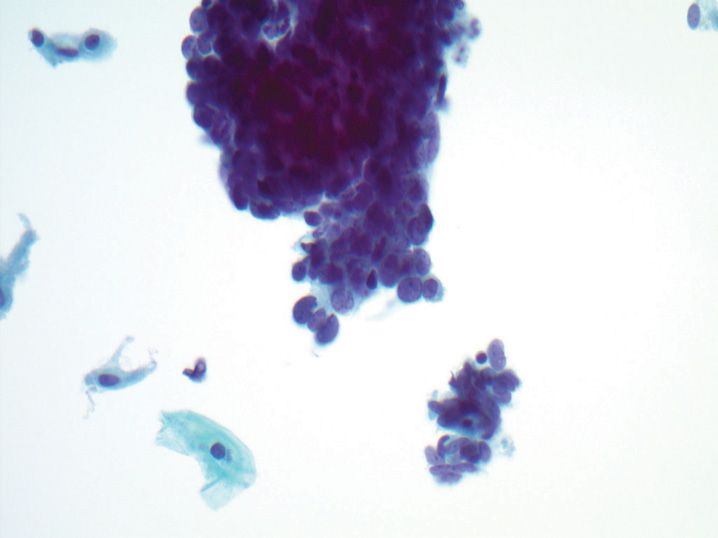
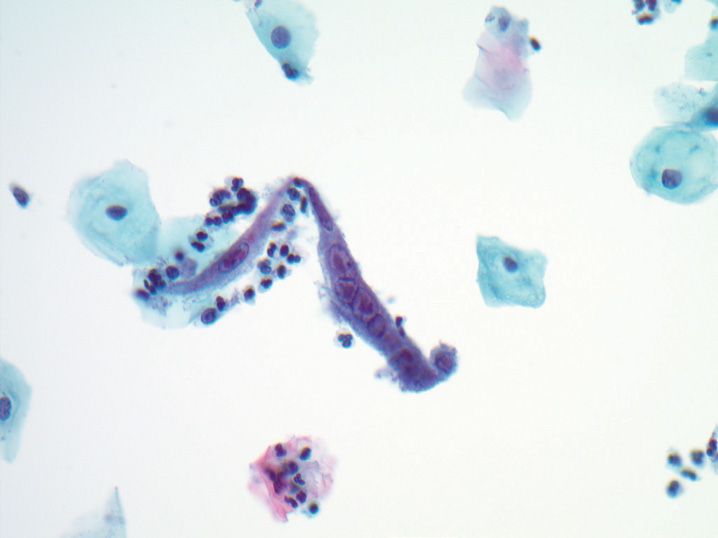
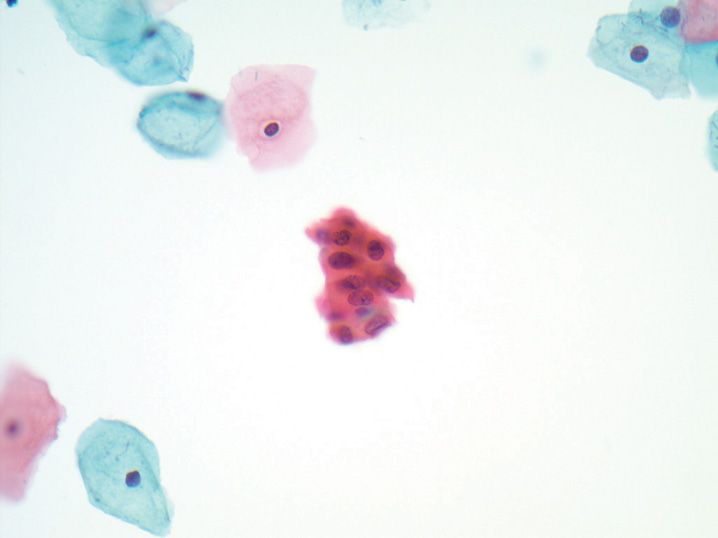
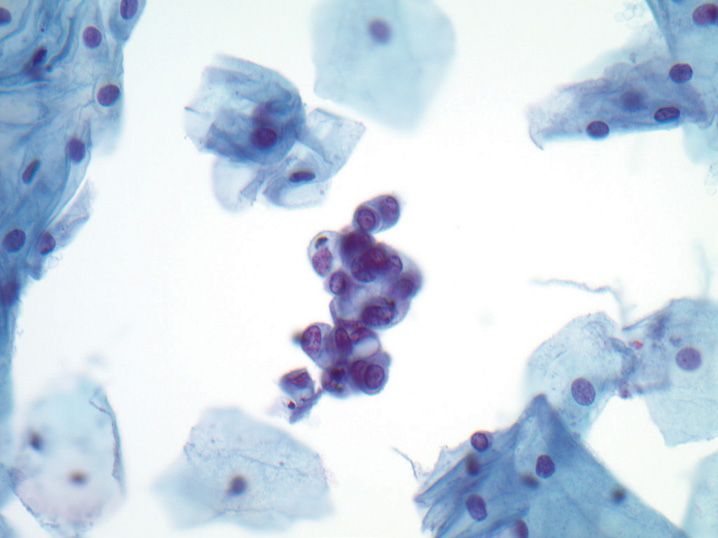
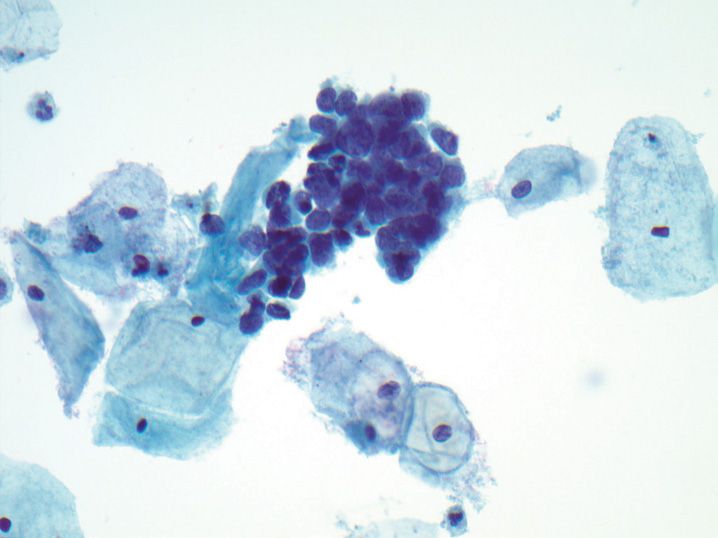
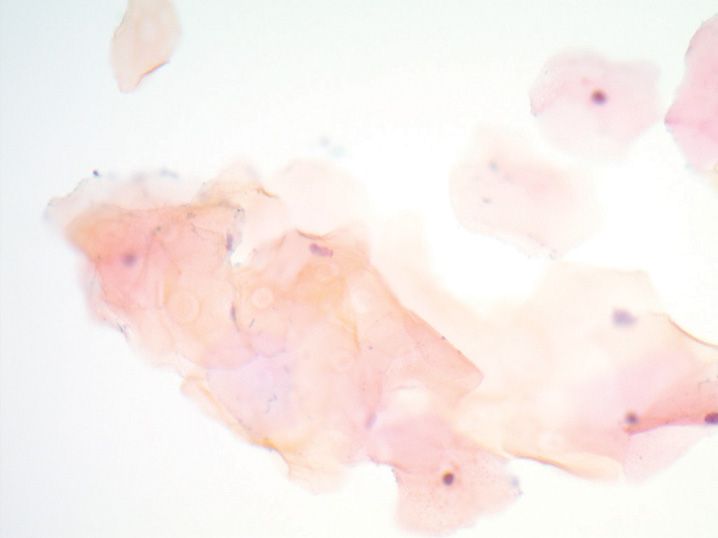
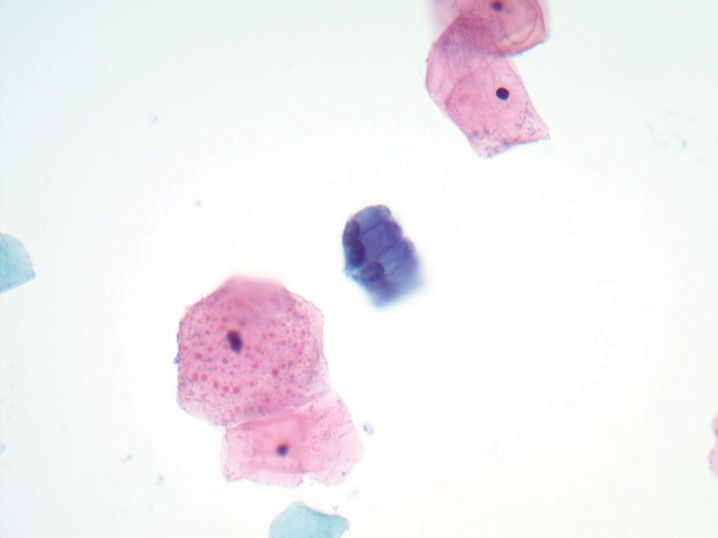
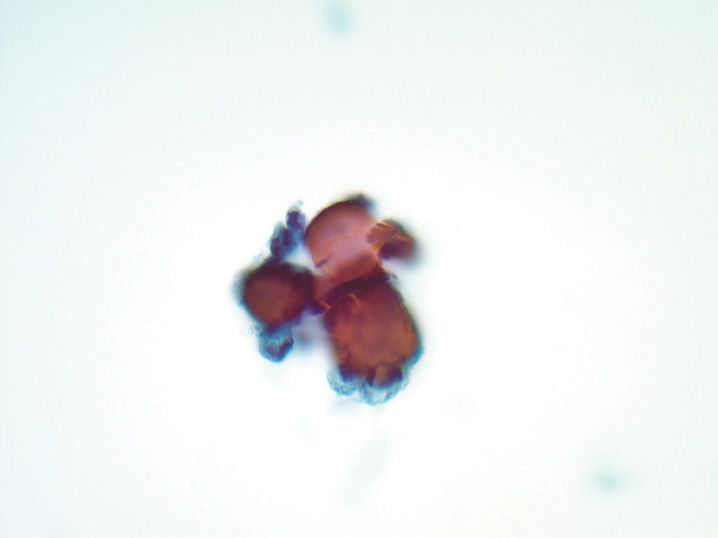
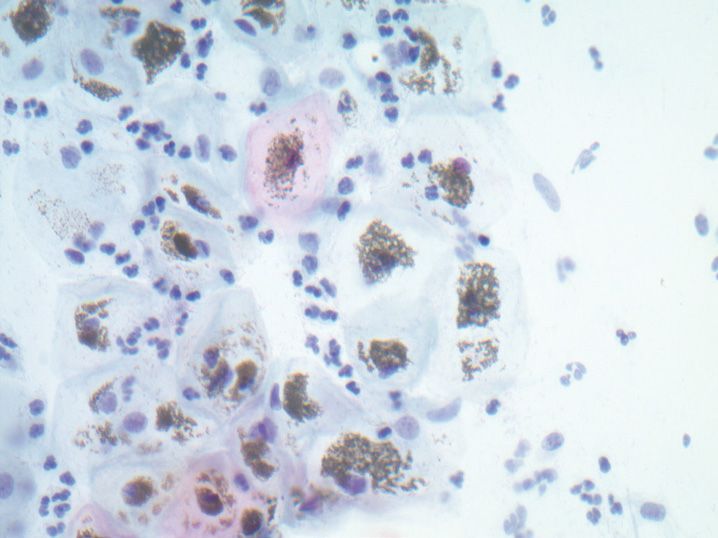
FIGURE 8-1
(A) Atrophy, negative for intraepithelial lesion or malignancy
(B) Low-grade squamous intraepithelial lesion (LSIL)
(C) High-grade squamous intraepithelial lesion (HSIL)
(D) Repair, negative for intraepithelial lesion or malignancy
(E) Squamous cell carcinoma (SCC)
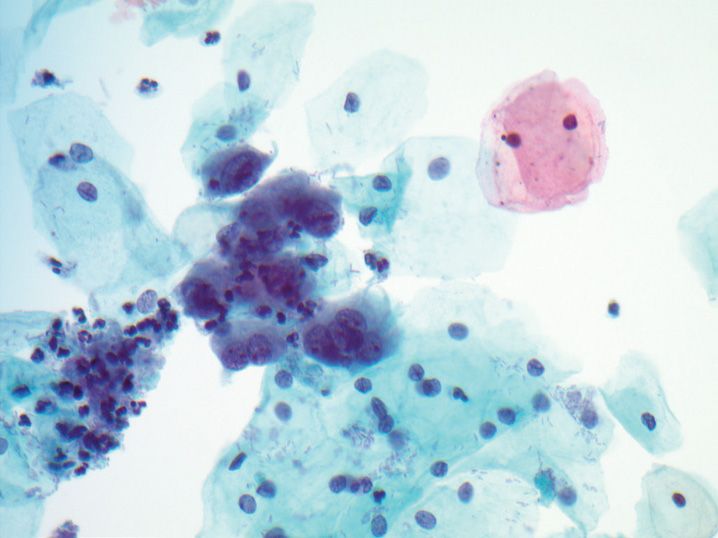
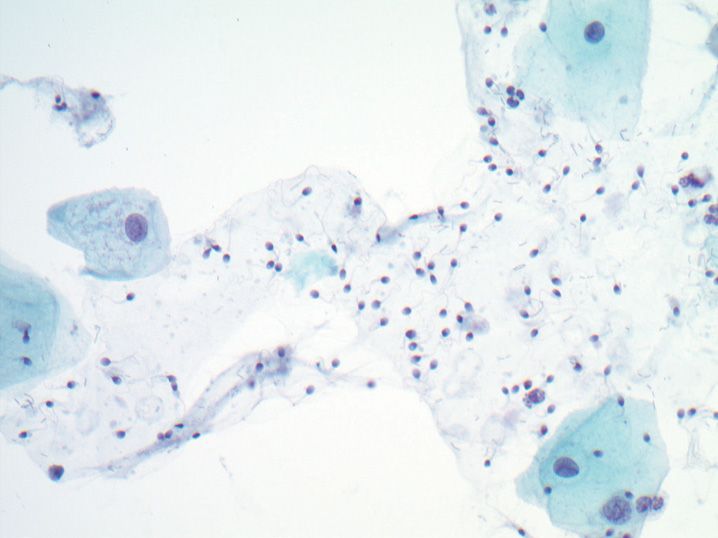
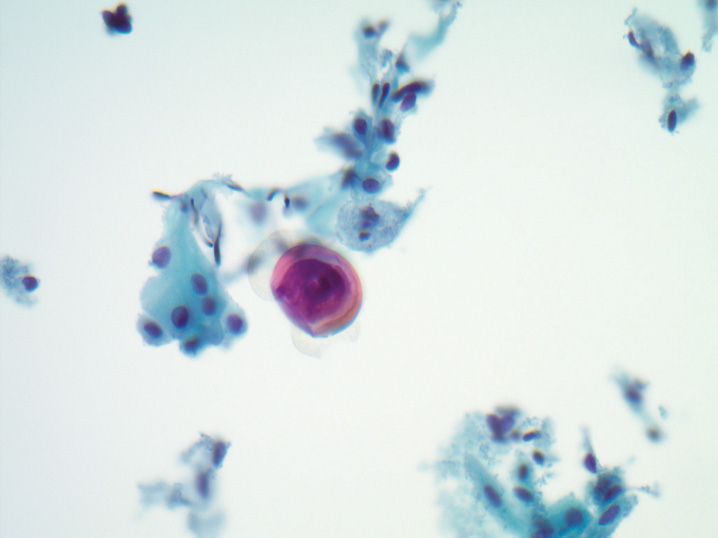
2. Which of the following statements is true regarding the microorganism present in this Pap test (see Figure 8-2)?
(A) Candida glabrata is the most common organism
(B) Classically shows both yeast and hyphae from cervical samples
(C) Considered a sexually transmitted disease
(D) Most common cause of abnormal vaginal discharge
(E) Presence on Pap test does not always correlate with symptomatic infection
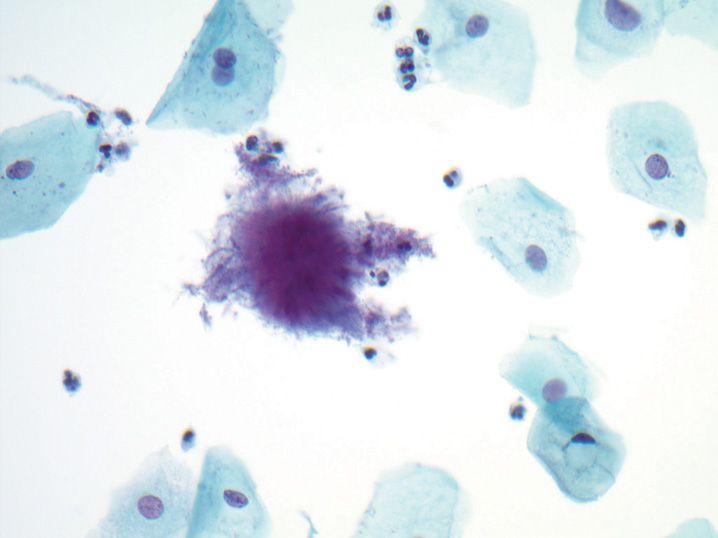
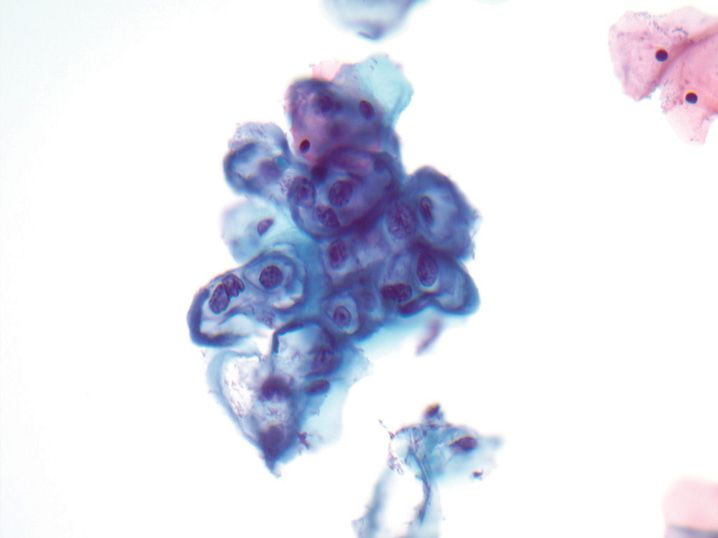
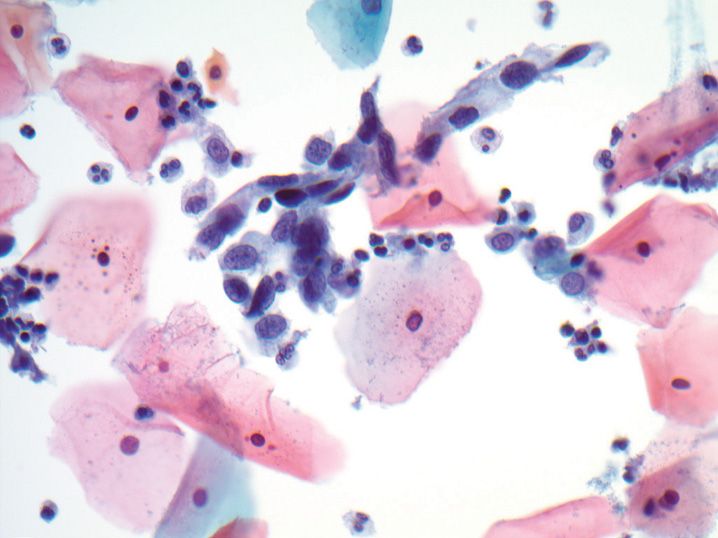
3. A Pap test was performed on a 31-year-old woman and demonstrates the following cytologic findings (see Figure 8-3). What is the next best/acceptable step in the management of this woman?
(A) Cervical colposcopy with endocervical sampling
(B) Colposcopy, endocervical sampling, and endometrial sampling
(C) Reflex human papilloma virus testing, and colposcopy if positive
(D) Repeat Pap in 6–12 months
(E) Routine screening in 3 years
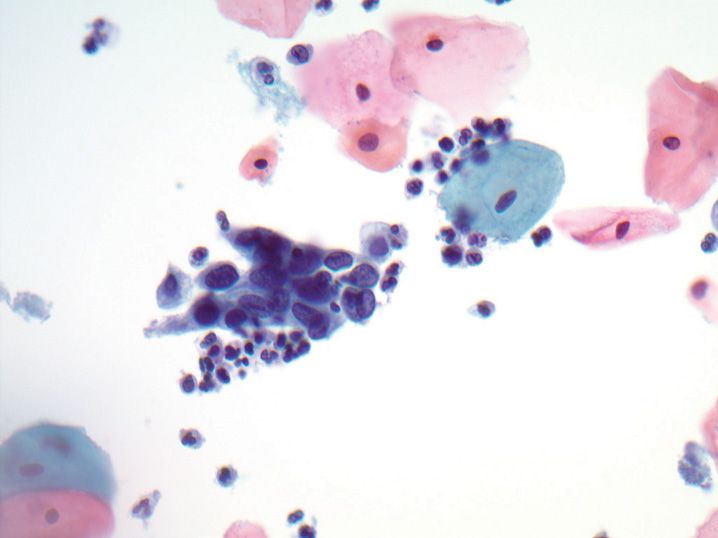
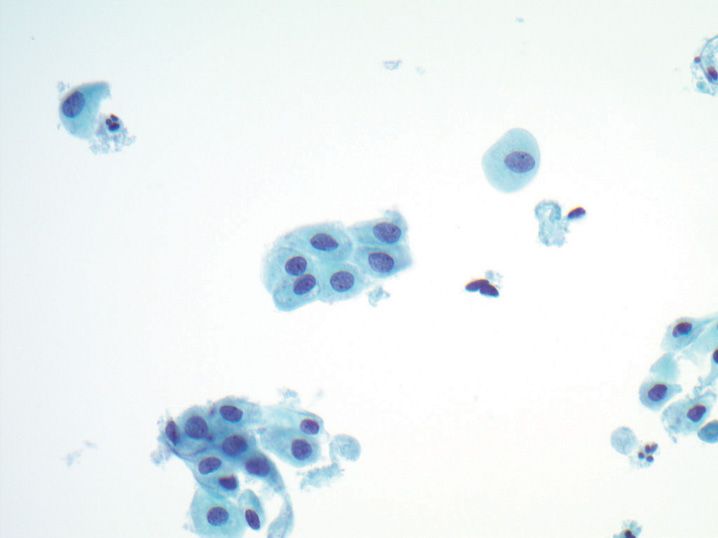
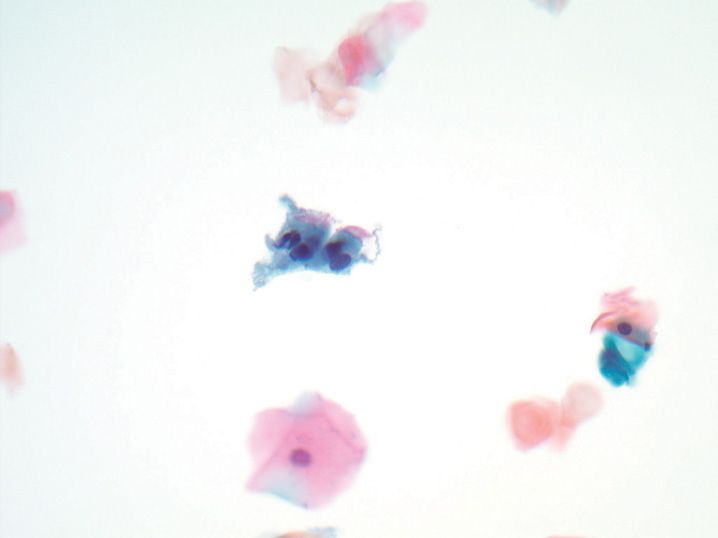
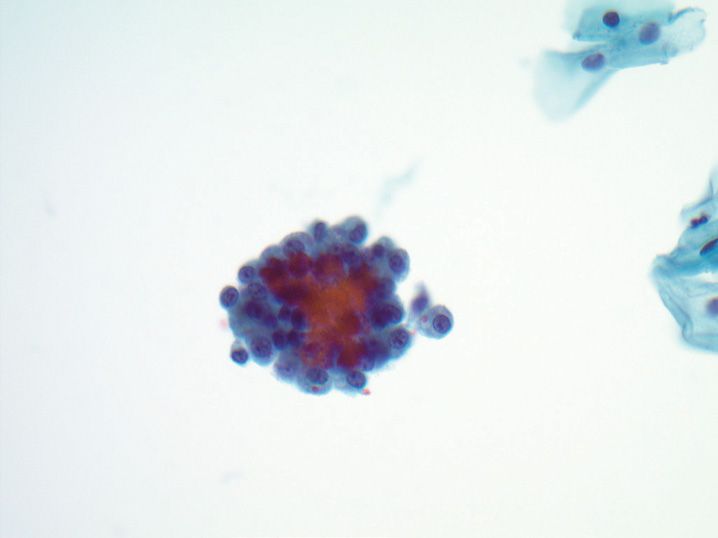
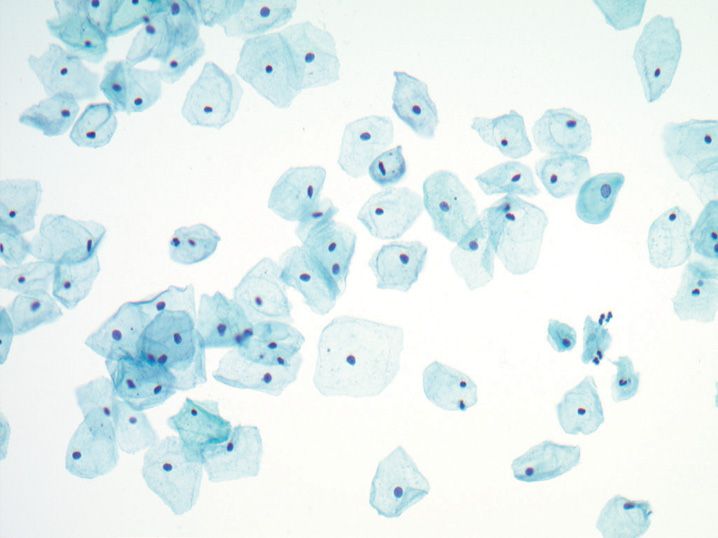
4. A 42-year-old woman presents for annual exam. A representative field from her Pap test is shown (see Figure 8-4). What clinical history is important to correlate with this finding?
(A) Body mass index (BMI)
(B) Diethylstilbestrol (DES) exposure
(C) History of squamous dysplasia
(D) Last menstrual period
(E) Prior loop electrosurgical excision procedure (LEEP) conization
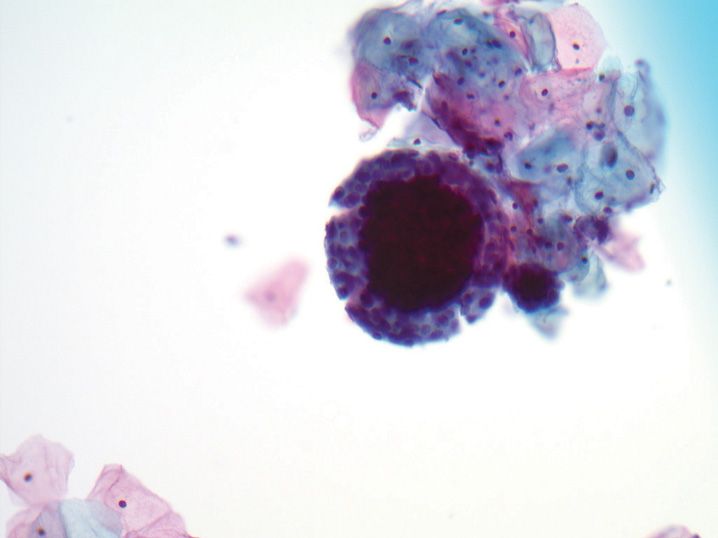
5. A 22-year-old woman presents for her annual Pap test (see Figure 8-5). The best interpretation of this is
(A) Adenocarcinoma in situ
(B) Endocervical adenocarcinoma
(C) Exfoliated endometrial cells
(D) Normal endocervical cells
(E) Tubal metaplasia
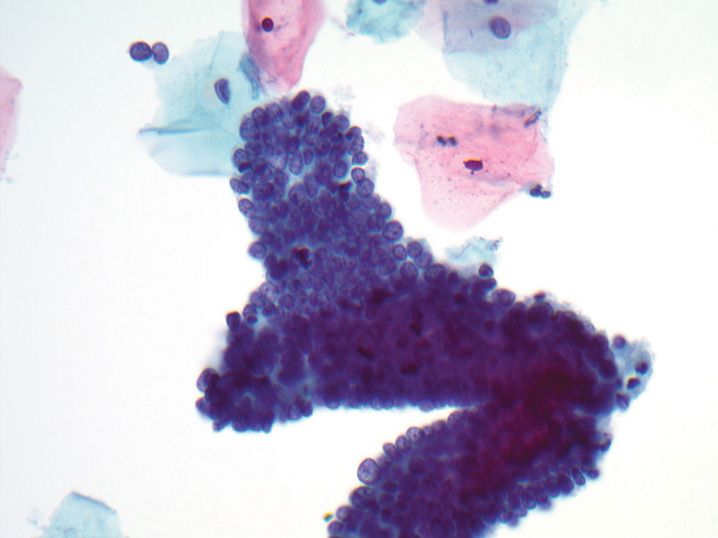
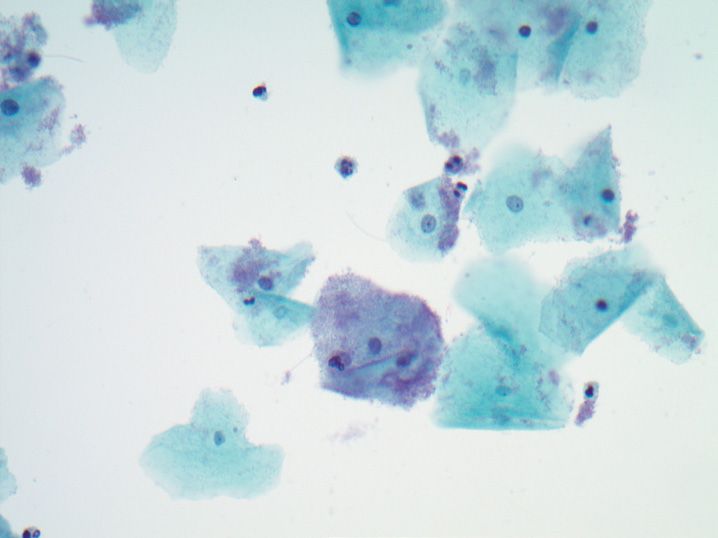
6. A 23-year-old woman presents for routine follow-up. Her Pap test shows the following changes (see Figure 8-6). The best interpretation for this Pap test is
(A) Atypical squamous cells of undetermined significance (ASC-US)
(B) Low-grade squamous intraepithelial lesion (LSIL)
(C) Negative for intraepithelial lesion or malignancy; fungal organisms consistent with Candida species present
(D) Negative for intraepithelial lesion or malignancy; reactive cellular changes present
(E) Negative for intraepithelial lesion or malignancy; Trichomonas vaginalis present
7. A 29-year-old woman presents for follow-up and a Pap test is performed (see Figure 8-7). The most likely clinical history that would correlate with this cervical cytology would be
(A) Follow-up for polycystic ovarian disease
(B) Human papilloma virus positive at last Pap
(C) Postpartum follow-up
(D) Pregnancy week 30 exam
(E) Radiation therapy for Hodgkin disease
8. A 27-year-old woman presents for her annual physical and a Pap test is performed (see Figure 8-8). The most likely clinical finding at exam is
(A) Ammonia or “fishy” odor to vaginal discharge
(B) Blisters on the cervix or vulva
(C) Intrauterine device present
(D) Strawberry cervix (microhemorrhages)
(E) White, thick discharge
9. The most important criterion to determine if the cells present in this Pap test (see Figure 8-9) are atypical is
(A) Feathering
(B) High nuclear-to-cytoplasmic ratio
(C) Increase in nuclear size
(D) Presence of small nucleoli
(E) Three-dimensional arrangement
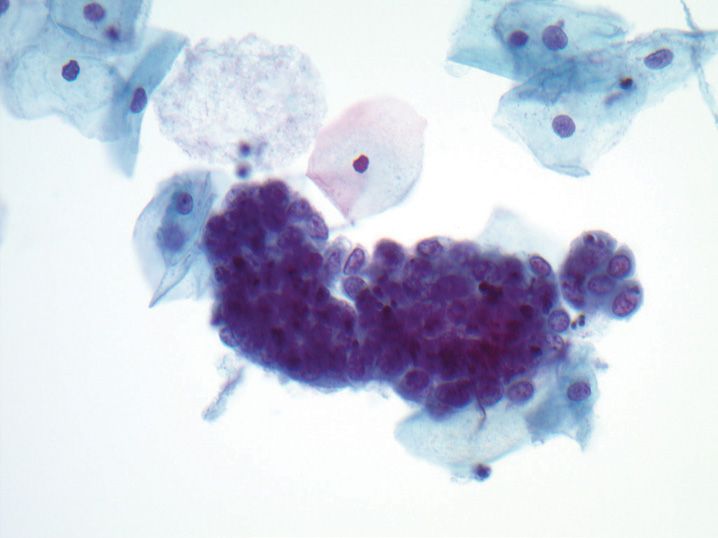
10. A Pap test was performed on a 37-year-old woman, and demonstrates the following cytologic findings (see Figure 8-10). The best interpretation for this is
(A) Low-grade squamous intraepithelial lesion (LSIL)
(B) High-grade squamous intraepithelial lesion (HSIL)
(C) Negative for intraepithelial lesion or malignancy, atrophy
(D) Negative for intraepithelial lesion or malignancy, repair
(E) Squamous cell carcinoma (SCC)
11. The organism present in this Pap test (see Figure 8-11) is classically seen in association with what other infectious organism?
(A) Candida
(B) Gardnerella
(C) Herpes
(D) Lactobacillus
(E) Trichomonas
12. A 32-year-old woman with infertility problems has the following vaginal smear appearance (see Figure 8-12). This appearance is associated with which of the following states?
(A) Granulosa cell tumor of ovary
(B) Newborn girl
(C) Postmenopausal
(D) Pregnancy
(E) Second half of menstrual cycle
13. A 38-year-old woman has the following Pap test appearance (see Figure 8-13). What is the most likely clinical finding in this patient?
(B) Ovarian mass
(C) Pregnancy
(D) Uterine enlargement and bleeding
(E) Vaginal atrophy
14. A 22-year-old woman has a Pap test performed (see Figure 8-14). Features that favor a benign interpretation over an atypical interpretation of the central group of cells include all of the following except
(A) Abundant tall columnar cytoplasm
(B) Flat strips and sheets
(C) High nuclear-to-cytoplasmic (N:C) ratio
(D) Honeycomb arrangement
(E) Nuclear enlargement up to 4 times normal cells
15. A 21-year-old woman with no prior history comes in for an annual examination. A Pap test is performed (see Figure 8-15). The changes in this figure most likely represent
(A) Bacterial vaginosis
(B) Coverslipping artifact
(C) Glycogen deposition
(D) Keratohyaline granules
(E) Koilocytic change
16. A 52-year-old woman presents for annual screening. The changes on her Pap test (see Figure 8-16) are most likely secondary to
(A) Herpes simplex infection
(B) History of radiation therapy
(C) Human papilloma virus-related cervical dysplasia
(D) Intrauterine device (IUD)
(E) Invasive squamous cell carcinoma
17. A 31-year-old woman presents for her annual Pap test (see Figure 8-17). This finding is most commonly associated with which of the following processes in women under 50?
(A) Candida
(B) Chlamydia
(C) Lymphoma
(D) Small cell carcinoma
(E) Trichomonas
18. A 38-year-old woman presents for her annual Pap test, which shows the following findings (see Figure 8-18). Which of the following statements is true regarding this process?
(A) Likely represents metastasis from an occult lung primary
(B) May be associated with a background of low-grade squamous intraepithelial lesion (LSIL)
(C) Most commonly associated with human papilloma virus type 16
(D) Rapid development can occur in the interval between screening Pap tests
(E) Treated similar to conventional squamous cell carcinoma
19. A 28-year-old woman who is 34 weeks pregnant has a Pap test (see Figure 8-19). Based on the findings present, which of the following changes in clinical management is indicated?
(A) Cesarean section instead of vaginal delivery
(B) Colposcopy immediately, with biopsy
(C) Deferred colposcopy until 6 weeks postpartum
(D) Therapy with antifungal cream
(E) Therapy with metronidazole (Flagyl)
20. A 25-year-old pregnant woman presents for her first prenatal visit, and has a Pap test performed. Rare cells are seen (see Figure 8-20), which most likely represent?
(A) Aria–Stella reaction
(B) Clear cell carcinoma
(C) Decidual cells
(D) Endometrial adenocarcinoma
(E) Intrauterine device (IUD) effect
21. A 29-year-old woman presents for her annual Pap test. The following changes are seen (see Figure 8-21). The most likely clinical finding at exam is
(A) Ammonia or “fishy” odor to vaginal discharge
(B) Blisters on the cervix or vulva
(C) Intrauterine device present
(D) Strawberry cervix (microhemorrhages)
(E) White, thick discharge
22. A 27-year-old woman has a Pap test performed (see Figure 8-22). Which of the following cytomorpho-logic changes is not a feature of this cell type?
(A) Coarse chromatin
(B) Crowded clusters
(C) Increased nuclear-to-cytoplasmic ratio
(D) Pseudostratified nuclei
(E) Vacuolated cytoplasm
23. A 43-year-old woman undergoes a Pap test (see Figure 8-23). The best interpretation for this finding is
(A) Atypical squamous cells of undetermined significance (ASC-US)
(B) High-grade squamous intraepithelial lesion (HSIL)
(C) Negative for intraepithelial lesion or malignancy (NILM), hyperkeratosis present
(D) NILM, parakeratosis present
(E) NILM, reactive cellular changes present
24. A 22-year-old woman presents for her annual Pap test (see Figure 8-24). The structures present at the center of the figure are
(A) Candida albicans hyphae
(B) Leptothrix
(C) Psammoma bodies
(D) Spermatozoa
(E) Trichomonas vaginalis
25. A 25-year-old woman presents for Pap test screening. The following changes are seen (see Figure 8-25). What is the most appropriate next clinical step?
(A) Cervical colposcopy
(B) Endometrial sampling
(C) Reflex human papilloma virus testing, and colposcopy if positive
(D) Repeat Pap in 6–12 months
(E) Routine screening in 3 years
26. A 35-year-old woman undergoes Pap test screening. Her Pap test demonstrates an unusual finding (see Figure 8-26 photomicrograph). This finding is most commonly associated with which of the following conditions?
(A) Abnormal bleeding
(B) High-grade intraepithelial lesion (HSIL)
(C) Intrauterine device (IUD)
(D) Pregnancy
(E) Trichomonas infection
27. A 37-year-old woman presents for Pap test screening. The following cells are seen (see Figure 8-27). What type of contraception is she most likely using?
(A) Birth control pill (estrogen/progestin)
(B) Condoms
(C) Depo-Provera (progestin injections)
(D) Intrauterine device (IUD)
(E) None
28. A 49-year-old woman with a history of invasive ductal carcinoma of the breast presents for annual Pap test screening. Her cervix exam is normal, and her Pap test shows rare atypical cells (see Figure 8-28) in an otherwise normal-appearing background. The most likely source of the malignant cells is
(A) Endocervical adenocarcinoma
(B) Endometrial adenocarcinoma
(C) Invasive squamous cell carcinoma
(D) Large cell lymphoma
(E) Metastatic breast carcinoma
29. A 31-year-old woman presents for a screening Pap test. The presence of abundant cells with the following features (see Figure 8-29) can be associated with all of the following conditions except
(A) Cervical condyloma
(B) Invasive well-differentiated squamous cell carcinoma
(C) Pregnancy
(D) Uterine prolapse
(E) Vulvar contamination
30. A 35-year-old woman with a history of a hysterectomy in the past due to fibroids has a Pap test performed, with the following finding (see Figure 8-30). Which of the following is the most likely reason for this finding in this patient?
(A) Atrophy
(B) Diethylstilbestrol (DES) exposure as a child
(C) Endocervical adenocarcinoma
(D) Endometrial adenocarcinoma
(E) Fallopian tube prolapse
31. A 43-year-old woman presents for Pap test screening which shows the following changes (see Figure 8-31). This finding has been found in association with all of the following conditions except
(A) Atrophy
(B) Cervical polyp
(C) Endometrial carcinoma
(D) Endometriosis
(E) Ovarian carcinoma
32. A 31-year-old woman presents for Pap test screening. This structure (see Figure 8-32) is most likely
(A) Actinomyces
(B) Cocklebur
(C) Herpes simplex changes
(D) Pollen
(E) Psammoma body
33. A 27-year-old woman has a Pap test performed at her 22-week prenatal checkup. The following changes are seen (see Figure 8-33). What is the next best step in clinical management of this woman?
(A) Cervical colposcopy with endocervical sampling
(B) Cervical colposcopy without endocervical sampling
(C) Reflex human papilloma virus testing, and colposcopy if positive
(D) Repeat Pap at 6 weeks postpartum
(E) Routine screening in 3 years
34. A 32-year-old woman undergoes conventional Pap test screening, and the clinician notices significant ferning of the mucus on the slide. This most commonly corresponds with
(A) High levels of estrogen immediately before ovulation
(B) High levels of estrogen postovulation
(C) High levels of progesterone immediately before ovulation
(D) High levels of progesterone postovulation
(E) Pregnancy
35. In the past, vaginal smears have been used to evaluate women for infertility using the maturation index (MI). Which of the following hormonal states is correctly paired with the MI expected (parabasal: intermediate:superficial cells)?
(A) Newborn 0:90:10
(B) Premenstrual child 0:80:20
(C) Preovulatory 0:60:40
(D) Postmenopausal 20:80:0
(E) Postovulatory 0:40:60
36. A 34-year-old woman has a Pap test that contains clusters of hyperchromatic crowded groups. All of the following findings can cause hyperchromatic crowded groups except
(A) Atrophy
(B) Benign endometrial cells
(C) Endocervical adenocarcinoma in situ
(D) High-grade squamous intraepithelial lesion (HSIL)
(E) Low-grade squamous intraepithelial lesion (LSIL)
37. The peak age range for women with a diagnosis of invasive squamous cell carcinoma is
(A) 25–30 years old
(B) 30–35 years old
(C) 35–40 years old
(D) 40–45 years old
(E) 45–50 years old
38. What percentage of LSIL lesions will regress without further management within 2 years?
(A) <5%
(B) 20%
(C) 50%
(D) 80%
(E) >95%
39. Which of the following human papilloma virus (HPV) subtypes is considered high risk?
(A) 6
(B) 11
(C) 31
(D) 40
(E) 42
40. A woman has a vaginal smear with a maturation index (MI) of 0:80:20. Which of the following conditions could be associated with this MI?
(A) Granulosa cell tumor of the ovary
(B) Pregnancy
(C) Preovulation
(D) Polycystic ovarian disease
(E) Postmenopause
41. During a human papilloma virus (HPV) infection of the cervical squamous epithelium, which of the following changes is associated with integration of the HPV genome into the host cell genome?
(A) Disruption of the E1-E2 region of the virus genome
(B) Irreversible infection by human immunodeficiency virus (HIV)
(C) Morphologic change from high-grade squamous intraepithelial lesion (HSIL) to invasive squamous cell carcinoma
(D) Overexpression of E6, which binds to retinoblastoma (Rb) protein
(E) Overexpression of E7, which binds to p53 protein
42. What is the single most important risk factor in the development of cervical squamous cell carcinoma?
(A) Altered immune status (e.g., human immunodeficiency virus (HIV), leukemia)
(B) HLA variation
(C) Persistent human papilloma virus (HPV) infection
(D) Microtrauma
(E) Smoking
43. A 38-year-old woman has a Pap test, which is interpreted as high-grade squamous intraepithelial lesion (HSIL). A satisfactory colposcopy was performed, and the biopsy and endocervical curettage are negative for dysplasia. According to the 2012 ASCCP management guidelines, what is the next best step in the management of this woman?
(A) Human papilloma virus testing alone at 6 months
(B) Repeat colposcopy at 2 years
(C) Repeat Pap test alone at 12 months
(D) Repeat Pap test with human papilloma virus (HPV) cotesting at 12 months
(E) Routine screening in 3 years
44. A 41-year-old woman presents for a screening Pap test, and benign-appearing exfoliated endometrial cells are present without other changes. Her last menstrual period is provided, and she is in day 9 of her cycle. The 2001 Bethesda System for Reporting Cervical Cytology recommends which of the following interpretations?
(A) Atypical endometrial cells
(B) Epithelial cell abnormality. Other: Endometrial cells present in a woman ≥40 years of age
(C) Negative for intraepithelial lesion or malignancy (changes consistent with menstrual smear)
(D) Negative for intraepithelial lesion or malignancy (no comment regarding endometrial cells)
(E) Negative for intraepithelial lesion. Other: Endometrial cells present in a woman ≥40 years of age.
45. A 28-year-old woman presents for a screening Pap test, and an interpretation of “atypical squamous cells of undetermined significance (ASC-US)” is made. Assuming reflex human papilloma virus (HPV) testing is performed on this sample, what is the 2012 ASCCP recommended management of this woman?
(A) If HPV negative: endocervical and endometrial sampling
(B) If HPV negative: cervical colposcopy
(C) If HPV negative: repeat Pap at 12 months
(D) If HPV positive: cervical colposcopy
(E) If HPV positive: repeat Pap at 12 months
46. A cell on a Pap test has a high nuclear to cytoplasmic ratio (close to 1:1). All of the other features listed below would be compatible with an interpretation of high-grade squamous intraepithelial lesion (HSIL) according to the 2001 Bethesda System for Reporting Cervical Cytology except
(A) Densely keratinized cytoplasm
(B) Irregular nuclear membrane
(C) Nuclear hyperchromasia
(D) Small cell size
(E) Vesicular chromatin
47. A 36-year-old woman has a Pap test, which is interpreted as atypical glandular cells, not otherwise specified (AGC, NOS). According to the 2012 ASCCP management guidelines, what is the next best clinical management step?
(A) Cervical colposcopy with endocervical sampling
(B) Colposcopy, endocervical sampling, and endometrial sampling
(C) Reflex human papilloma virus (HPV) testing, and colposcopy if positive
(D) Repeat Pap in 6–12 months
(E) Routine screening in 3 years
48. A 21-year-old woman presents for her initial Pap test. An interpretation of low-grade squamous intraepithelial lesion (LSIL) is made. According to the 2012 ASCCP management guidelines, what is the next best step in management of this process?
(A) Cervical colposcopy with endocervical sampling
(B) Colposcopy, endocervical sampling, and endometrial sampling
(C) Reflex human papilloma virus testing, and colposcopy if positive
(D) Repeat Pap in 12 months
(E) Routine screening in 3 years
49. A 32-year-old woman has a negative Pap test, but human papilloma virus (HPV) testing is positive. According to the 2012 ASCCP management guidelines, what next step in the clinical management of this woman is most appropriate?
(A) Diagnostic excisional procedure
(B) HPV genotyping
(C) Immediate colposcopy
(D) Repeat HPV testing
(E) Repeat Pap test and HPV testing in 24 months
50. A 57-year-old postmenopausal asymptomatic woman presents for a Pap test. An interpretation of “negative for squamous intraepithelial lesion, endometrial cells present in a woman over 40”, is made. The endometrial cells are not atypical. According to the 2012 ASCCP management guidelines, what is the next best clinical management step for this woman?
(A) Colposcopy with endocervical sampling and endometrial sampling
(B) Endometrial sampling
(C) Reflex human papilloma virus testing and colposcopy if positive
(D) Repeat Pap test in 12 months
(E) Routine screening in 3 years
51. Two vaccines have recently been developed against high-risk human papilloma virus subtypes 16 and 18. Both of these vaccines are manufactured using what process?
(A) Killed virus particles
(B) Live attenuated virus
(C) Recombinant DNA vectors
(D) Virus-like particles
(E) Virus particles conjugated to a hapten
52. A 37-year-old woman has a Pap test performed, and an interpretation of “atypical squamous cells, cannot exclude a high-grade squamous intraepithelial lesion (ASC-H)”, is made. According to the 2012 ASCCP management guidelines, what is the next best step in the clinical management of this woman?
(A) Cervical colposcopy
(B) Cervical colposcopy and endometrial sampling
(C) Reflex human papilloma virus testing, and colposcopy only if positive
(D) Repeat Pap in 12 months
(E) Routine screening in 3 years
53. A 41-year-old woman has a Pap test performed, and it is interpreted as “atypical squamous cells, cannot exclude high-grade squamous intraepithelial lesion (ASC-H)”. Why is aggressive management recommended for this result?
(A) The risk of cervical intraepithelial neoplasia 1 (CIN1) on biopsy is 40–50%
(B) The risk of CIN1 on biopsy is >80%
(C) The risk of CIN2 or worse on biopsy is 10–15%
(D) The risk of CIN2 or worse on biopsy is 40–50%
(E) The risk of CIN2 or worse on biopsy is >80%
54. During human papilloma virus (HPV)-related carcinogenesis, which of the following HPV-derived genes is responsible for an increase in p16 protein?
(A) E5
(B) E6
(C) E7
(D) L1
(E) L2
55. A 19-year-old woman presents to her primary care physician and requests the human papilloma virus vaccine Gardasil. She asks what percentage of cervical cancers this vaccine can prevent, and if she will also be protected from cervical warts. She also asks if she will need to continue to have Pap tests after finishing the vaccination series. What do you tell her?
(A) 70% of cervical cancers; it covers cervical warts; she does not need further screening
(B) 70% of cervical cancers; it covers cervical warts; she does need further screening
(C) 70% of cervical cancers; it does not cover cervical warts; she does need further screening
(D) 95% of cervical cancers; it covers cervical warts; she does not need further screening
(E) 95% of cervical cancers; it does not cover cervical warts; she does need further screening
56. Liquid-based Pap tests (e.g., ThinPrep and SurePath) were developed to overcome many limitations of conventional Pap tests, such as obscuring elements and poor fixation. What is another advantage of liquid-based Pap tests over conventional Pap tests?
(A) Ancillary testing on residual specimen
(B) Clustering of atypical cells for easier identification
(C) Easier evaluation of glandular clusters
(D) Less intense nuclear staining
(E) Reduced number of cells evaluated
57. Which of the following workloads can a cytopathologist perform and be within acceptable limits (without using automated screening)?
(A) Primary screening of 30 Pap tests and secondary review of 50 Pap tests in 3 hours of work
(B) Primary screening of 50 Pap tests and secondary review of 30 Pap tests in 3 hours of work
(C) Primary screening of 80 Pap tests in 6 hours of work
(D) Primary screening of 100 conventional Pap tests in 6 hours of work
(E) Primary screening of 200 liquid-based Pap tests in 8 hours of work
58. Which of the following quality control methods is required by a cytology laboratory that screens Pap tests, according to the Clinical Laboratory Improvement Amendments (CLIA) 1988 regulations?
(A) Correlation of all concurrently performed cervical biopsies with Pap test prior to final sign-out
(B) Correlation of all follow-up biopsies for all Pap tests after sign-out
(C) Rescreening of all negative high-risk Pap tests prior to final sign-out
(D) Rereview of all Pap tests in the last 5 years prior to the first interpretation of high-grade squamous intraepithelial lesion (HSIL)
(E) Random rescreening of at least 10% of negative Pap tests prior to final sign-out
59. Which of the following scenarios is an appropriate use of high-risk human papilloma virus (HPV) testing for the detection of cervical neoplasia?
(A) Follow-up of a 32-year-old woman with cervical intraepithelial neoplasia 1 (CIN1) 6 months ago and negative colposcopy
(B) Initial triage of a 19-year-old woman with atypical squamous cells of undetermined significance (ASC-US)
(C) Initial triage of a 31-year-old woman with atypical squamous cells, cannot exclude high-grade intraepithelial lesion (ASC-H)
(D) Initial triage of a postmenopausal woman with low-grade squamous intraepithelial lesion (LSIL)
(E) Primary HPV testing in a 29-year-old woman
60. The ThinPrep Imaging System (TIS) is the most widely used imaging system for cytology specimens, and is FDA approved for primary screening of cervical cytology. Which of the following statements is accurate regarding the TIS?
(A) Full manual review is required for all cases with an abnormality in at least one field of view
(B) There is no difference in sensitivity for the detection of atypical squamous cells of undetermined significance (ASC-US) or worse compared with manual review
(C) Slides can be filed without examination by a cytotechnologist if no abnormalities are identified by the imager
(D) The imager identifies 20 fields of view, which a cytotechnologist must review
(E) There is no difference in cytotechnologist productivity using this system, only increased detection of dysplasia
61. A 26-year-old woman has a Pap test interpretation of atypical squamous cells of undetermined significance (ASC-US), and reflex human papilloma virus testing is positive. At colposcopy, no lesions are identified, but the examination is considered unsatisfactory, as the transition zone cannot be visualized. Why is visualization of the transitional zone important for a satisfactory colposcopy?
(A) Glandular epithelium is more susceptible to human papilloma virus infection
(B) Most squamous lesions cannot be visualized in the ectocervix
(C) Most squamous lesions involve the endocervix
(D) Squamous metaplasia is more likely to involve the endocervix
(E) The squamocolumnar junction is the site of most initial human papilloma virus infections
62. Pap test screening can be discontinued for which of the following women?
(A) A 58-year-old woman who underwent hysterectomy for severe squamous dysplasia 10 years ago and has had 2 negative vaginal Pap tests
(B) A 63-year-old woman with no prior abnormal paps and three consecutive negative Pap tests in the last 10 years
(C) A 70-year-old woman with a history of diethylstilbestrol (DES) exposure and three consecutive negative Pap tests within the last 10 years
(D) A 71-year-old woman with a history of atypical squamous cells of undetermined significance (ASC-US) at age 66 and three consecutive negative Pap tests since that time
(E) A 79-year-old woman with a previous high-grade squamous intraepithelial lesion (HSIL) at age 34 and 3 consecutive negative Pap tests in the last 10 years
63. A 27-year-old woman is in the second half of her menstrual cycle, and a vaginal test performed has the following appearance (see Figure 8-34). Which of the following is true regarding the maturation index (MI) and appropriateness for her menstrual cycle?
(A) Appropriate for phase, MI: 0/20/80
(B) Appropriate for phase, MI: 0/80/20
(C) Inappropriate for phase, MI: 0/20/80
(D) Inappropriate for phase, MI: 0/80/20
(E) Inappropriate for phase, MI: 60/40/0
64. A 25-year-old woman had a Pap test performed. The changes seen (see Figure 8-35) represent
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree