(1)
Department of Pathology, Radboud University Nijmegen Medical Center, Nijmegen, The Netherlands
Keywords
Jaw CystsOdontogenic CystsPseudocysts2.1 Introduction
Cysts of the jaws are classified in distinct categories depending on histogenesis and etiology. Those that arise from odontogenic epithelium are called odontogenic, those that have their source in other epithelial structures are known as non-odontogenic. Within the odontogenic cysts and based on etiology, one discerns between inflammatory and developmental [1]. By definition, cysts are lined by epithelium but there are also cavities in the jaws that lack such an epithelial investment; they are included in this Chapter as well for differential diagnostic considerations.
2.2 Odontogenic Cysts – Inflammatory
2.2.1 Radicular Cyst
Radicular cysts are cystic lesions located at the root tips of teeth (Figs. 2.1 and 2.2) [2] and they arise from the rests of Malassez, remnants of dental epithelium involved in root formation that lie in the fibrous tissue that connects the tooth with its jaw socket, the so-called periodontal ligament. When triggered by inflammation, usually due to tooth decay, these epithelial nests increase in size whereafter they turn into a cyst due to subsequent liquefaction necrosis of the central part (Figs. 2.3 and 2.4). It is the most frequently encountered odontogenic cyst [3, 4].
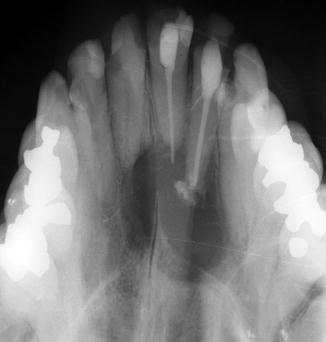

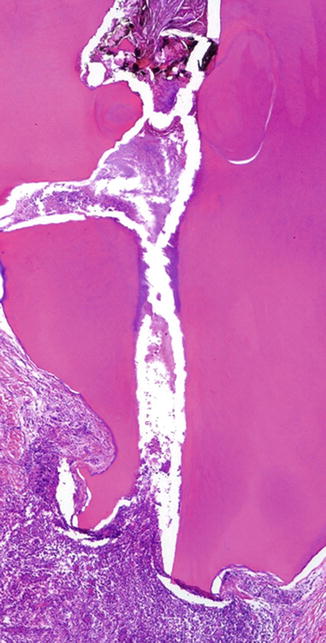
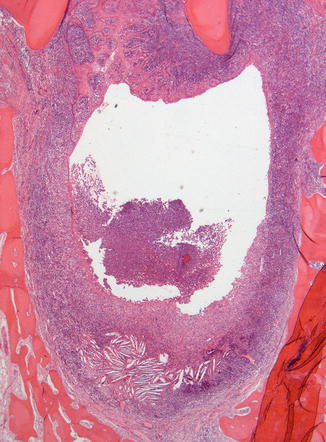
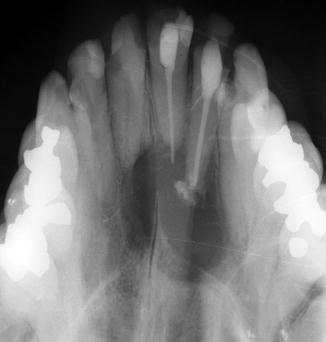
Fig. 2.1
Radiograph showing radicular cyst. A large radiolucent lesion surrounds the apices of 2 anterior incisor teeth that have their roots filled to treat pulpal inflammation. Before treatment, this pulpal disease has spread through the apical root foramen into the adjacent jaw bone with as outcome cyst formation resulting in local loss of bone

Fig. 2.2
Bisected molar tooth with attached radicular cyst. Occasionally, a radicular cyst remains attached to the roots during tooth extraction (Reproduced from Slootweg [2])
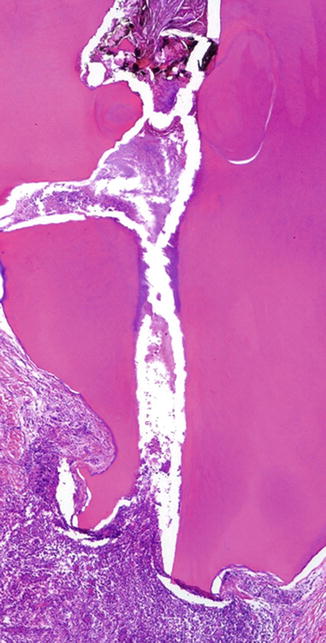
Fig. 2.3
Low power view showing inflammatory infiltrate at the root tip of a decayed tooth. Radicular cyst development may be a sequel of this condition due to reactive proliferation of odontogenic epithelial remnants located in the periodontal ligament
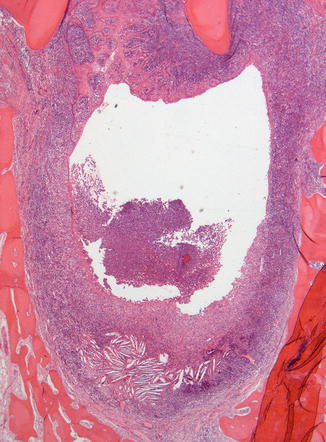
Fig. 2.4
In areas of inflammation at the root apex, odontogenic epithelial remnants increase in size. Central liquefaction in these epithelial clusters transforms them into a cyst lined with epithelium, usually of the squamous type
Histologically, these cysts are lined by nonkeratinizing stratified squamous epithelium that may show elongated rete processes that may form arches (Fig. 2.5) or are thin and atrophic (Fig. 2.6). Also, pronounced intercellular edema may be shown (Fig. 2.7). In many cysts, cholesterol clefts with adjacent giant cells occur. Within the cyst epithelium, hyaline bodies (Rushton bodies) of various size and shape may be present (Fig. 2.8), the specific nature of which remains unclear [5]. Occasionally, the lining squamous cells are admixed with mucous cells or ciliated cells (Fig. 2.9). In maxillary cysts, this finding could be explained by the vicinity of the lesion to respiratory mucoa lining the maxillary sinus or nasal cavity but as these cells also occur in the lining of cysts in the mandible, it represents genuine aberrant differentiation of odontogenic epithelium. Sometimes, the histologic pattern of the radicular cyst is complicated by extensive intramural proliferation of squamous epithelial nests of varying size, thus mimicking a squamous odontogenic tumor (Fig. 2.10) [6]. A similar histology may be shown by other jaw cysts, in particular when there are extensive inflammatory changes that obscure the more specific histological details of these latter ones. When differentiating between a genuine radicular cyst and one of these other jaw cysts, one should realize that radicular cysts usually are small and located at the root tip of a decayed tooth. If cysts histologically resembling a radicular cyst are not in the periapical tooth area, not related to a decayed tooth and have a big size thus involving large areas of the mandible, one should be suspicious that one is dealing with a dentigerous cyst, an odontogenic keratocyst, or a unicystic ameloblastoma in which the specific diagnostic features have disappeared due to secondary inflammatory changes. In those cases, it is the best approach to make a note that possibly, the submitted specimen is not representative for the lesion. Another item of diagnostic confusion may arise when the Rushton bodies are mistaken for ghost cells, a feature in a lot of odontogenic lesions that will be dealt with later on in more detail.
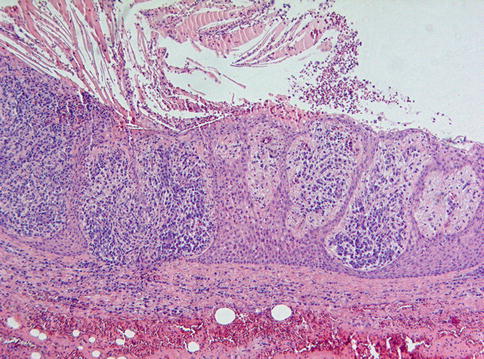
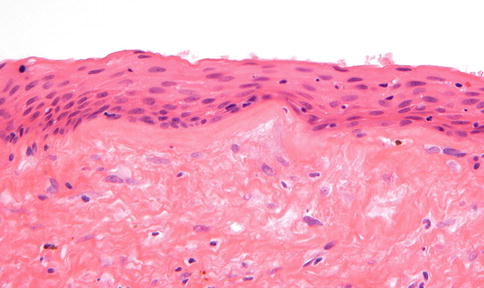
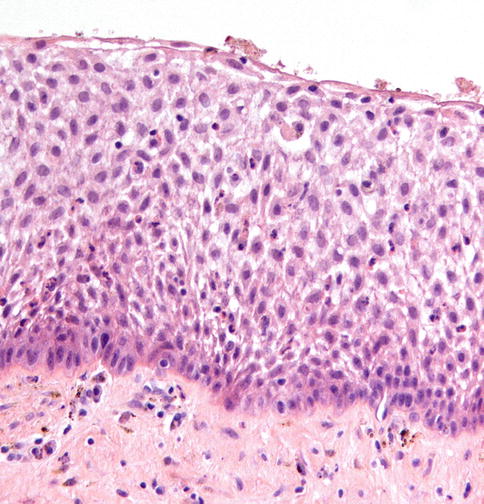
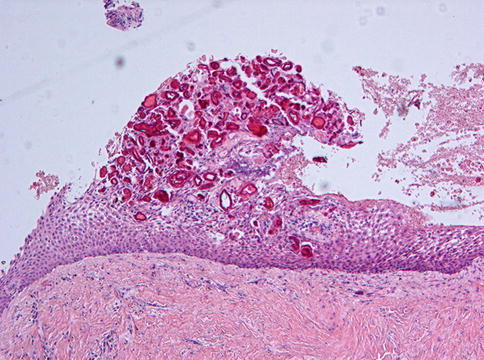
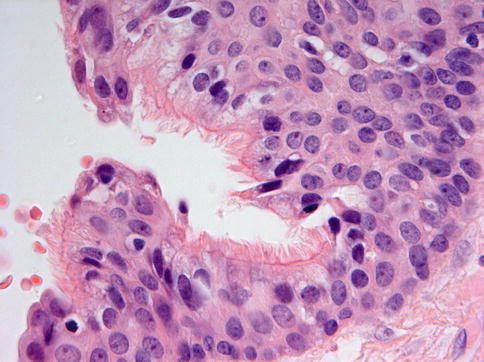

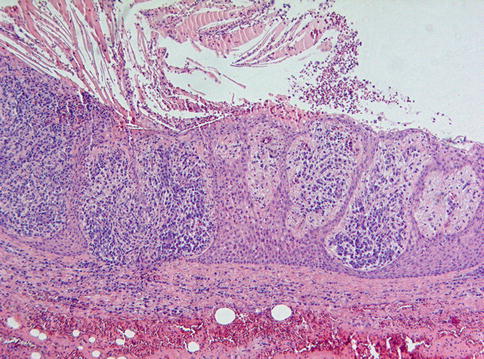
Fig. 2.5
Radicular cysts are lined by non-keratinizing squamous epithelium that may show elongated rete ridges sometimes forming roman arches
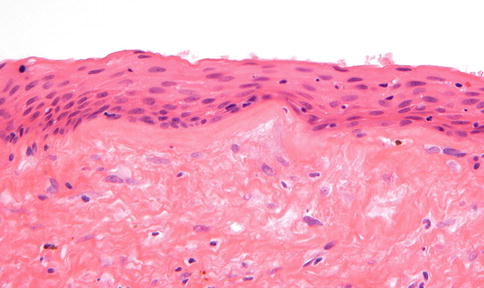
Fig. 2.6
Detail of the lining of a radicular cyst, in this case composed of a thin layer of squamous epithelium
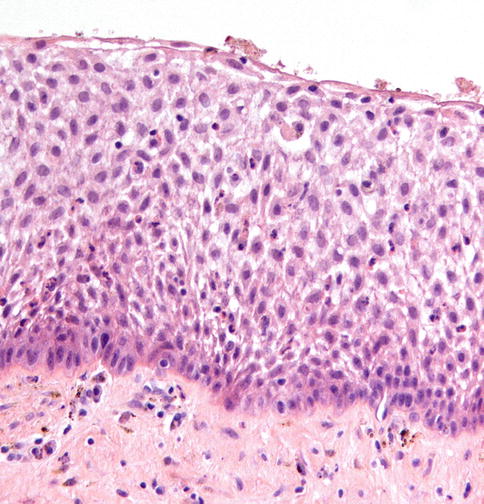
Fig. 2.7
In case of inflammation, the epithelial lining may show spongiotic changes that should not be confused with the stellate reticulum present in ameloblastoma
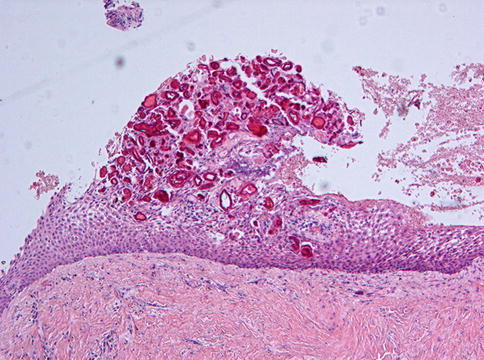
Fig. 2.8
Intraepithelial acellular deposits known as Rushton bodies are a common feature in a variety of odontogenic cysts. They should not be confused with ghost cells
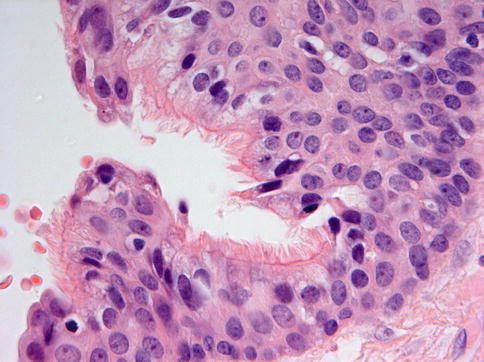
Fig. 2.9
Mucous cells and ciliated cells may be present in the lining of radicular cysts. This is an incidental finding without any diagnostic significance. In this picture, ciliated cells are shown

Fig. 2.10
Large intramural nests of odontogenic epithelium can be found in radicular cysts. This may mimic squamous odontogenic tumor
When a radicular cyst is retained in the jaws after removal of the associated tooth, the lesion is called residual cyst.
2.2.2 Paradental Cyst
The paradental cyst is a cystic lesion located at the lateral side of the tooth at the border between tooth crown and root surface. The cyst is secondary to an inflammatory process in the adjacent periodontal tissues that induces proliferation of neighboring odontogenic epithelial rests, similar to the pathogenesis of the radicular cyst [7, 8] and its histological features are the same. Only the site is different, radicular cysts lying at the root tip and the paradental cysts located at the root surface close to the tooth crown. Moreover, radicular cysts are the results of tooth decay and paradental cysts are associated with inflammation of the soft tissues that surround the neck of the tooth, the tooth itself being without any pathology. When keeping this in mind, the distinction between radicular and paradental cyst is relatively easy provided the relevant clinical data are provided.
2.3 Odontogenic Cysts – Developmental
2.3.1 Dentigerous Cyst
The dentigerous (follicular) cyst is a very common lesion. Its radiologic and gross appearance is highly characteristic, a cyst lumen in which the tooth crown protrudes and a cyst wall that is attached to this tooth at the junction between crown and root (Figs. 2.11 and 2.12) [9]. Probably, this cyst arises from fluid accumulation between the tooth’s enamel surface and the remnants of the epithelial enamel organ that invests the tooth crown as long as the tooth has not erupted in the oral cavity.



Fig. 2.11
Radiograph of dentigerous cyst. The crown of the right mandibular 3rd molar tooth is surrounded by a radiolucent lesion partly extending into the mandibular ramus

Fig. 2.12
Gross view of dentigerous cyst. The cyst wall is attached to the neck of the involved tooth which is a typical feature for this odontogenic developmental cyst (Reproduced from Flucke and Slootweg [9])
Microscopical examination shows a cyst wall that is connected to the tooth at the cement-enamel junction (Fig. 2.13) and usually with a thin epithelial lining that may be only two to three cells thick (Fig. 2.14). In case of inflammation, the epithelium becomes thicker and may resemble that of a radicular cyst. Also, mucous producing cells as well as ciliated cells may be observed (Fig. 2.15). The connective tissue component of the cyst wall may be fibrous or fibromyxomatous and may also contain varying amounts of epithelial nests representing remnants of the dental lamina and should not be mistaken for some type of odontogenic neoplasm (Fig. 2.16). Occasionally, the cyst wall may show aggregates of tiny amorphous calcifications, usually associated with odontogenic epithelial nests (Figs. 2.17 and 2.18). This close association between odontogenic epithelium and calcified deposits is however not unique for dentigerous cysts but is a general feature of odontogenic epithelial remnants.
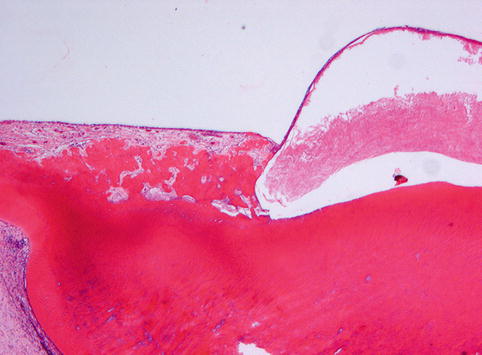
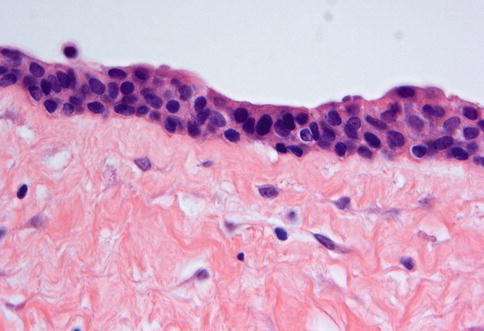
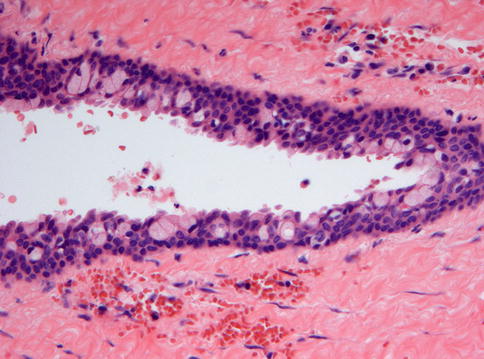
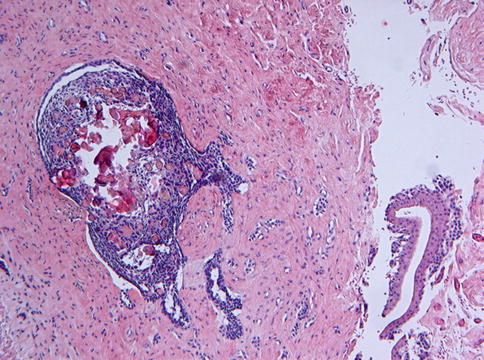
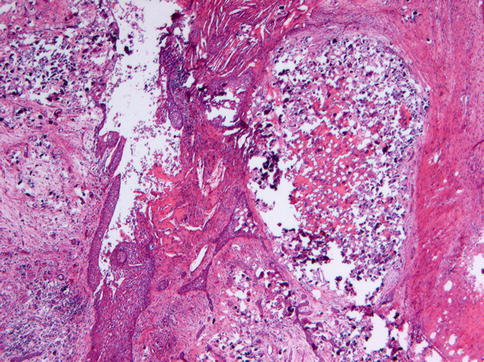
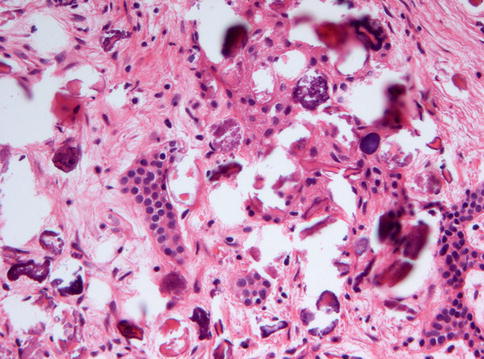
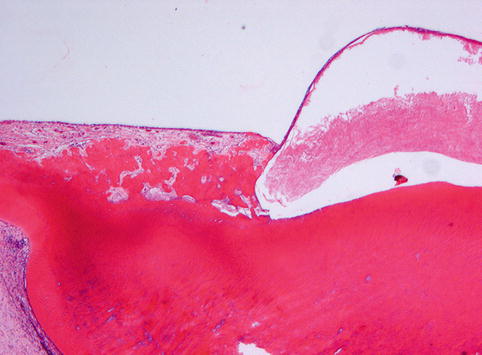
Fig. 2.13
Low power view of a dentigerous cyst. The attachment of the cyst wall to the neck of a tooth is the diagnostic hallmark of this lesion but can only be visualized when tooth and cyst wall are processed for histology as a single block
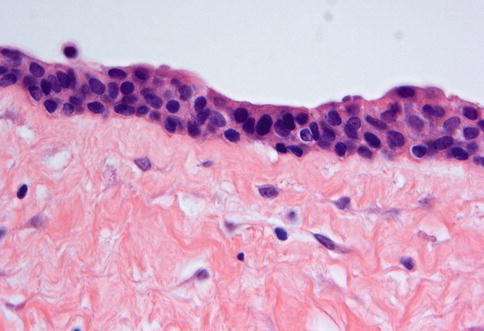
Fig. 2.14
A thin multilayered cuboidal epithelium is the most simple lining of a dentigerous cyst
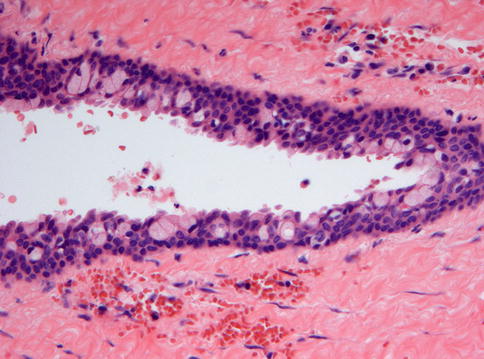
Fig. 2.15
Mucous cells and ciliated cells may form part of the lining of dentigerous cysts. In this Figure, mucous cells are shown
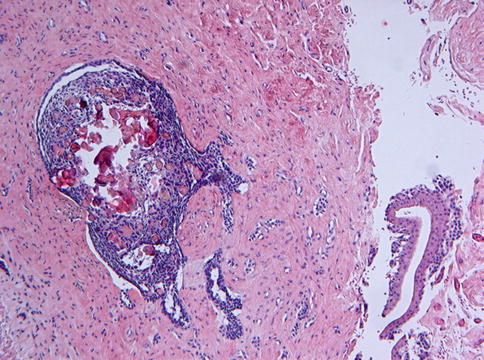
Fig. 2.16
Wall of dentigerous cyst showing a large nest of odontogenic epithelium composed of ameloblastoma-like cells and ghost cells. This should be considered a tiny hamartomatous lesion without clinical significance. Similar aggregates can be found in hyperplastic dental follicles
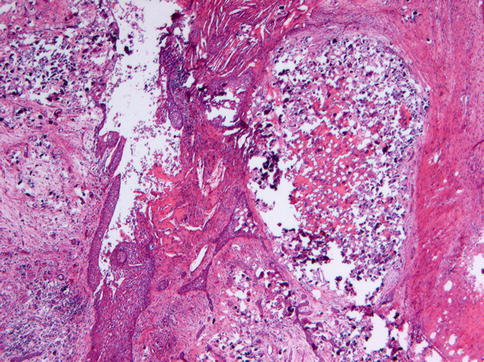
Fig. 2.17
Large areas of calcification in the wall of a dentigerous cyst
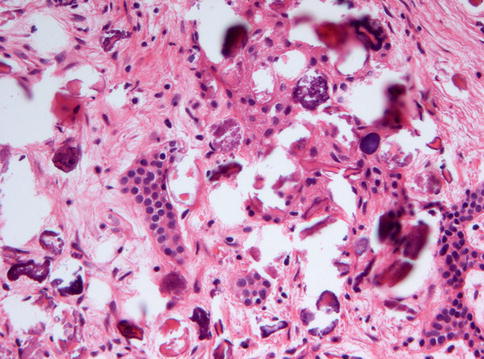
Fig. 2.18
Higher magnification of Figure 2.17 showing the close relationship between epithelium and calcified material
These fibromyxomatous areas in the connective tissue wall of a dentigerous cyst may resemble odontogenic myxoma and the presence of odontogenic epithelial rests may lead to the erroneous diagnosis of one or another type of epithelial odontogenic tumor [10]. However, identification of the epithelial cyst lining will rule out these alternatives.
The eruption cyst is a specific type of dentigerous cyst located in the gingival soft tissues overlying the crown of an erupting tooth. Mostly, these cysts are short-lived, rupturing with progressive eruption of the associated tooth. They are lined by squamous epithelium that is thickened due to inflammatory changes in the underlying connective tissue and thus similar to the lining of a radicular cyst.
Removal of the cyst wall and the involved tooth will yield a permanent cure.
2.3.2 Lateral Periodontal Cyst
Lateral periodontal cysts are rare lesions, derived from odontogenic epithelial remnants, and occurring on the lateral aspect or between the roots of vital teeth, this latter feature similar as for the paradental cyst [11]. Usually they are asymptomatic and fortuitous findings on radiographs, where they present as well-demarcated radiolucencies on the lateral surface of a tooth root (Fig. 2.19).
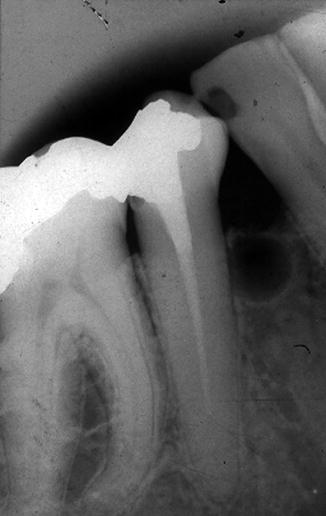
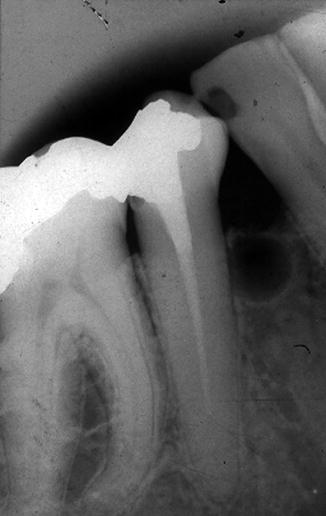
Fig. 2.19
Radiograph of lateral periodontal cyst showing a small radiolucent lesion in the interdental bony septum
These cysts are lined by thin, non-keratinizing squamous or cuboidal epithelium with focal, plaque-like thickenings consisting of clear cells that may contain glycogen (Figs. 2.20 and 2.21) [12].
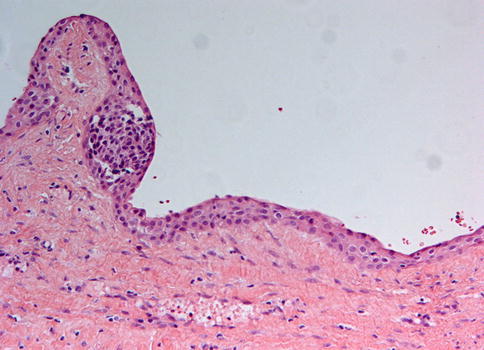
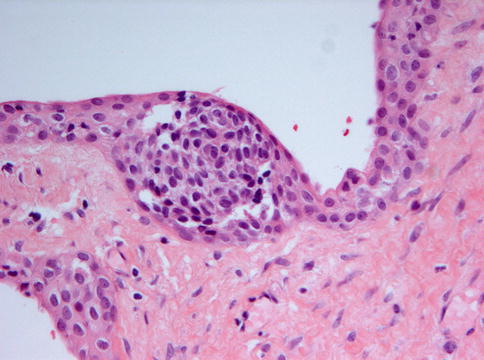
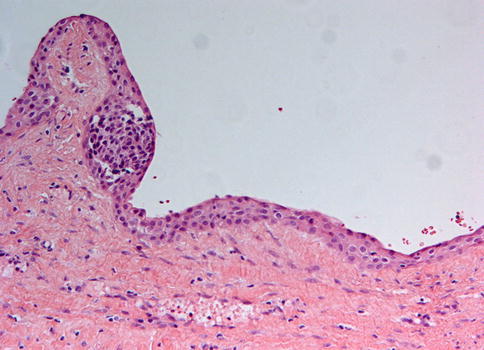
Fig. 2.20
Lateral periodontal cysts have a lining composed of non-diagnostic thin, non-keratinizing squamous or cuboidal epithelium. Local thickenings, the so-called plaques are the defining diagnostic feature
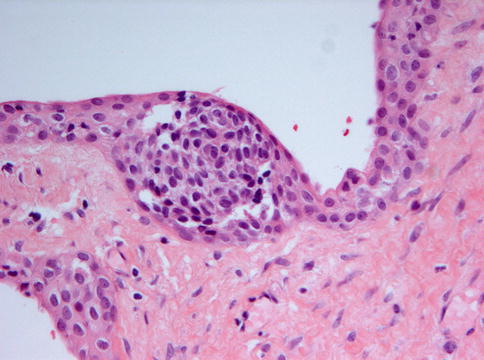
Fig. 2.21
Higher magnification of the plaques, diagnostic for both the lateral periodontal cyst as well as the botryoid odontogenic cyst
The botryoid odontogenic cyst represents a multilocular form of the lateral periodontal cyst [13]. Histologically, the same epithelial lining including presence of plaques is observed.
2.3.3 Glandular Odontogenic Cyst
The glandular odontogenic cyst, also called sialo-odontogenic cyst is a cystic lesion characterized by an epithelial lining with cuboidal or columnar cells both at the surface and lining crypts or cyst-like spaces within the thickness of the epithelium [1, 3]. The lesion is rare.
This cyst most commonly affects the body of the mandible, particularly the anterior part, and the most prominent symptom is painless swelling.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


