Cystic Nephroma/Mixed Epithelial and Stromal Tumor
Satish K. Tickoo, MD
Victor E. Reuter, MD
Key Facts
Terminology
Cystic nephroma (CN), mixed epithelial and stromal tumor (MEST)
Multicystic to solid and cystic biphasic renal tumors that likely represent morphologic spectrum of same entity
Clinical Issues
CN: F:M = approximately 8:1; MEST: Mostly in females with only rare reported cases in males
Incidentally detected kidney mass is most common clinical presentation
All reported cases of typical CN and MEST have behaved in benign fashion following surgical excision
Macroscopic Features
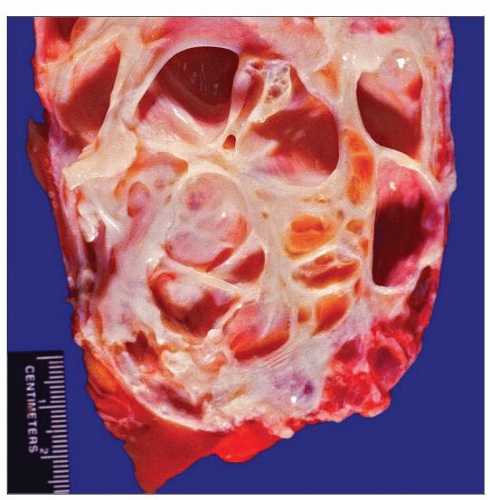
CN: All tumors entirely cystic with no solid areas or expansile nodules
MEST: Variably solid and cystic, sometimes with predominant solid component
Microscopic Pathology
Stroma in both CN and MEST with varied histologic features
Epithelial components in both CN and MEST with varied but similar features
Top Differential Diagnoses
Multilocular cystic RCC, tubulocystic carcinoma, CPDN, mesoblastic nephroma (classical type), metanephric adenofibroma
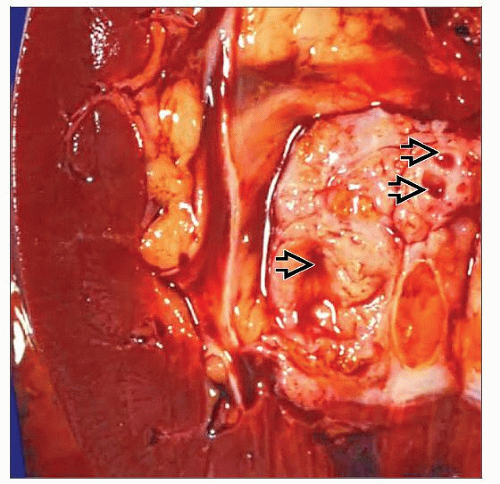
 Gross photograph of a cystic nephroma shows an exclusively cystic, well-circumscribed tumor with no solid areas. Gross distinction from multilocular cystic RCC is not possible in such cases. |
TERMINOLOGY
Abbreviations
Cystic nephroma (CN), mixed epithelial and stromal tumor (MEST)
Synonyms
Renal epithelial and stromal tumor (REST)
For MEST: Adult mesoblastic nephroma, cystic hamartoma of renal pelvis, leiomyomatous renal hamartoma, or solid and cystic biphasic tumor
Definitions
Multicystic to solid and cystic, mostly benign, biphasic renal tumors that likely represent morphologic spectrum of same entity
CN: Tumor composed entirely of cysts and cyst septae without any solid expansile areas or mural nodules
Septations with arbitrarily chosen thickness of less than 5 mm
MEST: Tumors with variable amounts of solid components
ETIOLOGY/PATHOGENESIS
Role of Hormones
Features that suggest role of steroid hormones in genesis and evolution of these tumors include
Marked female preponderance
Common history of long-term estrogen replacement in female patients
Long-term sex steroid exposure in male patients
Frequent expression of ER and PR in tumor mesenchymal component
Genetic Alterations
Gene expression profiles of mRNA demonstrate that both CN and MEST share similar expression profiles
Highest differentially expressed gene, relative to other tumors and nonneoplastic parenchyma, is insulin-like growth factor 2
Lowest differential expression is of carbonic anhydrase 2 gene
Single case of translocation t(1;19) in MEST also reported
CLINICAL ISSUES
Epidemiology
Age
Mean age similar for both CN and MEST: Approximately 53 years (range: 34-78 years)
CN in pediatric age group considered to be fully differentiated nephroblastoma
Not related to tumors seen in adults
Gender
CN: F:M approximately 8:1
MEST: Mostly in females with only rare reported cases in males
Presentation
Incidentally detected kidney mass is most common clinical presentation
Other described symptoms
Abdominal pain
Hematuria
Urinary tract infections
Prognosis
All reported cases of typical CN and MEST have behaved in benign fashion following surgical excision
1 reported case of MEST recurred locally 21 years after resection
A few cases of malignant MEST reported in literature
Malignant phenotype observed in either epithelial or mesenchymal components
Morphologic features of malignancy include increased cellularity, cytologic atypia, prominent nucleoli, and high mitotic rate
Spindle cell NOS, synovial sarcoma, rhabdoid, rhabdomyosarcoma, and chondrosarcoma differentiation in malignant stromal components
MACROSCOPIC FEATURES
General Features
Cystic nephroma
Tumors usually solitary; very rare bilateral cases reported
Most tumors well circumscribed and confined to kidney
Located mostly close to renal hilum but may involve cortex, particularly in larger tumors
All tumors entirely cystic with no solid areas or expansile nodules
Majority of cysts contain clear serous fluid, rarely hemorrhagic or purulent material
Mixed epithelial and stromal tumor
Mostly solitary and unilateral, with rare bilateral cases
Most tumors well circumscribed and confined to kidney
Very few tumors with ill-defined, infiltrative borders
Located mostly close to renal hilum and renal pelvis but may involve cortex, particularly in larger tumors
Variably solid and cystic, sometimes with predominant solid component
Size
Size range similar for both CN and MEST: 1.7-21 cm (mean: 6.5 cm)
MICROSCOPIC PATHOLOGY
Histologic Features
Stroma in both CN and MEST show varied histologic features, including
Loose fibrous and edematous
Dense fibrous and sclerotic
Hypercellular spindled, NOS
Ovarian stroma-like
Smooth muscle type
Prominent vasculature more common in MEST
Calcifications and foamy histiocytes present in both CN and MEST
Cells in epithelial components in both CN and MEST show varied features, including
Flat
Hobnailed
Cuboidal
Columnar
Urothelial-like
Clear cell
However, clear cell or urothelial-like cyst lining relatively uncommon in CN
Prominent ovarian stroma, smaller cysts, complex branching glands, phyllodes gland pattern, and stromal luteinization more common in MEST than CN
Predominant Pattern/Injury Type
Neoplastic
Predominant Cell/Compartment Type
Epithelial, biphasic or mixed
ANCILLARY TESTS
Immunohistochemistry
Stromal cells often positive for ER, PR, and less commonly for inhibin and calretinin, in both (but more often in MEST)
DIFFERENTIAL DIAGNOSIS
Multilocular Cystic Renal Cell Carcinoma
Differentiation is required from CN and predominantly cystic MEST
Multilocular cystic RCC with cysts showing variable flattened lining or almost entirely larger cells with clear cytoplasm
Clusters or nests of clear cells are always present in septae
No cellular or ovarian-type stroma
Lining cells with a CA9, CD10, and often CK7 positive immunophenotype
No stromal immunoreactivity for ER and PR
Tubulocystic Carcinoma
Tubulocystic carcinoma needs to be differentiated from CN and predominantly cystic MEST
Cells lining tubules and cysts in tubulocystic carcinoma have high-grade nuclei and abundant eosinophilic cytoplasm
Stroma usually dense fibrotic and desmoplastic
Septae often incomplete and free floating
No ER and PR positivity
Cystic Partially Differentiated Nephroblastoma (CPDN)
CPDN needs to be differentiated from CN and predominantly cystic MEST
CPDN shows at least focal nephroblastematous tissue, such as blastema, immature stromal cells, and primitive epithelium in septae
Almost all patients < 24 months old
Mesoblastic Nephroma (Classical Type)
Differential is with solid MEST
Classical mesoblastic nephroma shows finger-like extensions into surrounding renal parenchyma
Entrapped native tubules and glomeruli are often seen in mesoblastic nephroma
However, these are seen almost entirely in periphery of tumor
Mesoblastic nephroma shows no ER or PR positivity
Metanephric Adenofibroma
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree