Cutaneous Marginal Zone B-cell Lymphoma
Aaron Auerbach, MD, PhD
Key Facts
Terminology
Non-Hodgkin small B-cell lymphoma of centrocytelike marginal zone cells
Malignant B cells expanding marginal zones surrounding reactive follicles and colonizing them
Etiology/Pathogenesis
Borrelia burgdorferi in some cases
Associated with autoimmune disease
Clinical Issues
Excellent prognosis; 5-year survival: 90-100%
Usually treated with excision or radiation
Microscopic Pathology
Small B cells, monocytoid, plasmacytoid
Colonized germinal centers
Lymphoepithelial lesions rare
± Dutcher bodies
Ancillary Tests
B cells positive for CD20, may coexpress CD43 and Bcl-2
Germinal centers Bcl-6(+), CD10(+), Bcl-2(-)
CD21(+) loose follicular dendric cell meshworks
Usually light chain restriction and clonally rearranged immunoglobulin genes
t(11;18) negative
Top Differential Diagnoses
Follicular hyperplasia
Primary cutaneous follicle center lymphoma
Plasmacytoma
Secondary involvement by systemic marginal zone lymphoma
TERMINOLOGY
Abbreviations
Primary cutaneous marginal zone lymphoma (PCMZL)
Synonyms
Primary cutaneous immunocytoma
Definitions
Non-Hodgkin small B-cell lymphoma of centrocyte-like marginal zone cells
Recapitulates architecture of Peyer patches
Usually in sites without significant lymphoid tissue
Malignant B cells expanding marginal zones surrounding reactive follicles and colonizing them
May be difficult to diagnose because of nonspecificity of many of the morphologic features, absence of 1 or more classic features, and nature of the small biopsies
ETIOLOGY/PATHOGENESIS
Infectious Agents
Borrelia burgdorferi DNA found in skin in some European cases, but not in other populations
Other infectious diseases noted in tissue other than skin
Helicobacter pylori implicated in gastric marginal zone lymphoma
Campylobacter jejuni implicated in small intestine marginal zone lymphoma
Chlamydia psittaci implicated in ocular marginal zone lymphoma
Autoimmune Diseases
Marginal zone lymphoma has been associated with patients who have autoimmune diseases
Sjögren syndrome and parotid gland marginal zone lymphoma
Hashimoto thyroiditis and thyroid marginal zone lymphoma
CLINICAL ISSUES
Epidemiology
Age
Usually adults > 40 years old
Gender
No gender predominance
Ethnicity
No ethnic propensity
Site
Mostly upper extremity
Also head and neck and torso
Presentation
1 or more plaques or nodules
Rarely ulcerates
Multiple nodules often seen in systemic marginal zone lymphoma with secondary spread to dermis
Treatment
Excision or radiation therapy
If solitary or only a few lesions
Chemotherapy only considered for widespread disease, metastasis
Antibiotics
Sometimes therapy for Borrelia burgdorferi infection
Prognosis
Excellent
5-year survival: 90-100%
But tendency to recur
Rarely transforms to large B-cell lymphoma
So look for sheets of large B cells for diagnosis of large B-cell lymphoma
Scattered large B cells are often seen in PCMZL
MACROSCOPIC FEATURES
General Features
1 or more firm red nodules on skin
MICROSCOPIC PATHOLOGY
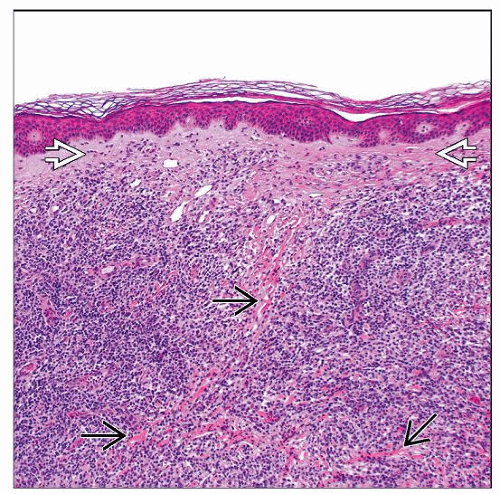
Histologic Features
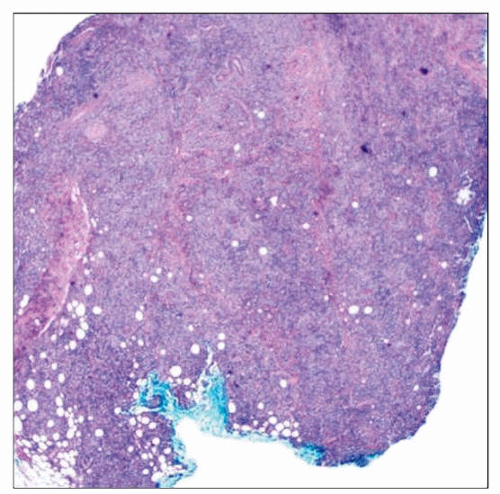
Nodular to diffuse dermal infiltrate
Spares epidermis with grenz zone
Sometimes involves subcutis
Malignant B cells expanding marginal zones surrounding reactive follicles and colonizing them
Lymphoepithelial lesions (very rare in skin)
Neoplastic cells
Sometimes monocytoid with ample pale/clear cytoplasm
Sometimes plasmacytoid with eccentric nucleus and pink cytoplasm
Variable numbers of plasma cells, neutrophils, and eosinophils
Mostly small in size with coarse chromatin and mild atypia
Dutcher bodies (intranuclear inclusions)
Sometimes seen
More often in marginal zone lymphoma than plasmacytoma
Russell bodies are cytoplasmic inclusions that may also be seen, but are less specific
Reactive germinal centers
Colonized by neoplastic marginal zone B cells
Still contain tingible body macrophages
Retain mantle zones
If tissue is small, may not see follicles
Follicular dendric cell meshworks
Often disrupted/loosened in colonized germinal centers
Lymphoepithelial lesions
3 or more lymphocytes entering epithelial structure (usually a gland) and destroying it
Very rarely seen in skin
Cytologic Features
Small to medium-sized B cells with mild atypia, 1 or more inconspicuous nucleoli, and scant pale cytoplasm
ANCILLARY TESTS
Immunohistochemistry
Neoplastic B cells
Express B-cell markers
Positive for CD19, CD20, CD22, CD79a
Shows predominance of B cells
Sheets of B cells with few T cells are concerning for B-cell lymphoma
If there is a mix of B and T cells, then look for other features (IHC, clonality) to diagnose lymphoma
Coexpression of T-cell markers is a feature of malignancy
B cells may coexpress CD43
B cells may coexpress Bcl-2
Bcl-2 is normally expressed on reactive mantle zone cells
Neoplastic B cells do not express
CD5, CD10, Bcl-6, CD21, or CD23
Light chain restriction
Usually in plasma cells &/or lymphoplasmacytic cells
Germinal centers
Positive markers
Bcl-6(+), CD10(+)
Negative markers
Bcl-2(−)
Follicular dendritic cell meshworks
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree