Cutaneous and Systemic Mastocytosis
Jeremy C. Wallentine, MD
Key Facts
Terminology
Heterogeneous group of clonal neoplastic proliferations of mast cells in ≥ 1 organ system
Cutaneous mastocytosis: Confined to skin
Systemic mastocytosis: Involvement of at least 1 organ ± skin lesions
Etiology/Pathogenesis
Frequently associated with somatic activating point mutations within c-KIT protooncogene
About 30% of SM cases associated with TET2 mutations
Clinical Issues
2/3 of cases occur in children
Prognosis depends on disease category
Pediatric onset CM has favorable outcome
Approximately 80% of patients with mastocytosis have evidence of skin involvement
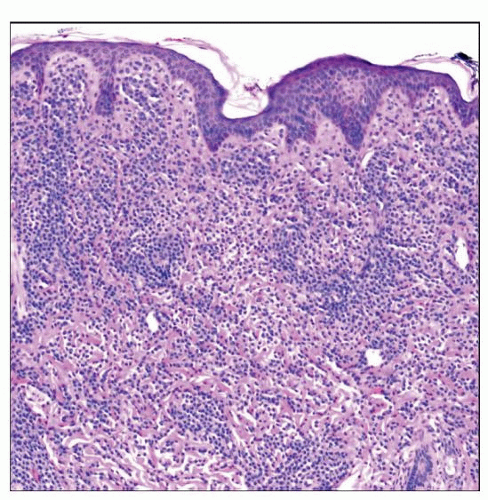
Microscopic Pathology
Multifocal compact or diffuse compact mast cell infiltrates
Diffuse interstitial infiltration pattern
Cytology varies, but abnormal features are almost always detected, including spindling and hypogranularity
Frequent bi- or multilobated nuclei usually indicate aggressive disease
Top Differential Diagnoses
Reactive mast cell hyperplasia
Cutaneous lymphoma
Myeloid and lymphoid neoplasms with eosinophilia
 This mastocytoma of the skin was present at birth on the right neck of this newborn. Mastocytomas of the skin occur almost exclusively in infants. (Courtesy S. Vanderhooft, MD.) |
TERMINOLOGY
Abbreviations
Cutaneous mastocytosis (CM)
Systemic mastocytosis (SM)
Synonyms
Mast cell disease
Definitions
Heterogeneous group of clonal, neoplastic mast cell proliferations that accumulate in 1 or more organ systems
Subtypes based mainly on distribution of disease and clinical manifestations
Cutaneous mastocytosis (CM): Mast cell infiltrates confined to skin
Urticaria pigmentosa (UP)/maculopapular cutaneous mastocytosis (MPCM)
Diffuse cutaneous mastocytosis
Mastocytoma of skin
Systemic mastocytosis (SM): Involvement of at least 1 extracutaneous organ ± skin lesions
Indolent systemic mastocytosis (ISM)
Systemic mastocytosis with associated clonal hematological non-mast cell lineage disease (SMAHNMD)
Aggressive systemic mastocytosis (ASM)
Mast cell leukemia (MCL)
Mast cell sarcoma (MCS)
Extracutaneous mastocytoma
ETIOLOGY/PATHOGENESIS
Molecular Background
Frequently associated with somatic activating point mutations within c-KIT protooncogene
Encodes tyrosine kinase receptor for stem cell factor (SCF)
Various mutations result in ligand-independent activation of c-KIT tyrosine kinase
Constitutively activated c-KIT leads to clonal proliferation of mast cells
Most common mutation: D816V in exon 17 encoding tyrosine kinase domain
Identified in ≥ 95% of adults with SM when sensitive methods are used
Present in 35% of pediatric CM cases
Provides relative resistance to prototypical tyrosine kinase inhibitor imatinib
Other activating point mutations: D816Y, D816H, D816F, and D816I in exon 17 (rarely seen)
Frequency significantly higher in CM than in SM
Activating point mutations in exons 8, 9, and 11 (mutually exclusive with codon 816 mutations)
44% of pediatric CM cases
Pediatric CM historically regarded as reactive condition with transient dysregulation of local growth factors
Increasing evidence supports neoplastic nature associated with activating c-KIT mutations (as in adults)
Despite high rate of spontaneous regression (mechanism unknown)
Rare familial cases with germline mutations of c-KIT have been reported
In patients with SM-AHNMD, additional genetic defects are detected depending on type of AHNMD
About 30% of SM cases associated with TET2 mutations
TET2 acts as putative tumor suppressor gene
50% of those cases also carry c-KIT D816V mutation
CLINICAL ISSUES
Epidemiology
Incidence
Very rare
Lack exact numbers with regard to frequency
Calculated incidence of 5-10 new cases per 1,000,000 population per year in various studies
CM
UP: Most common CM variant
Mastocytoma of skin (10-15% of pediatric CM cases)
Diffuse CM (rare)
SM
ISM: Most common SM variant (46% of SM cases)
SM-AHNMD (40% of SM cases)
ASM (12% of SM cases)
MCL, MCS, and extracutaneous mastocytoma are extremely rare
Age
Occurs at any age
2/3 occur in children in 1st 2 years of life
CM most common in children, less frequent in adults
50% of affected children develop typical skin lesions before 6 months of age
May present at birth
SM generally diagnosed after 2nd decade of life, rare in pediatric population
Gender
Slight male predominance in CM
M:F = 1:1-1:3 in SM
Site
Approximately 80% of patients with mastocytosis have evidence of skin involvement
CM: Mast cell infiltrates confined to skin
SM: Involvement of at least 1 extracutaneous organ ± skin lesions
Bone marrow (BM) almost always involved
Skin lesions occur in ≥ 50% of cases, more often in those with indolent disease
Spleen, lymph nodes, liver, and gastrointestinal tract mucosa
Rarely peripheral blood (PB) shows leukemia
Any tissue may be affected
Presentation
CM
Includes 3 distinct clinicohistopathologic entities
Characterized by 2 main groups of symptoms
Skin lesions due to mast cell infiltrate and release of mediators (flushing, blistering, pruritus)
Lesions can urticate when stroked (“Darier” sign) in 1/2 of cases
Systemic symptoms due to release of mast cell mediators (histamine most significant)
Headache
GI manifestations including acid reflux disease, peptic ulcer disease, and diarrhea
Respiratory symptoms including shortness of breath and asthma exacerbations
Cardiovascular symptoms including tachycardia, hypotension, syncope, or rarely, even shock
UP/MPCM
Widespread distribution of tan macules and occasionally nodules or plaques
In children, lesions tend to be larger and papular
Most lesions show intraepidermal accumulation of melanin pigment
Sparing of palms, soles, face, and scalp
In children, typically involving head and lateral face
Number of lesions varies, but does not predict presence of systemic disease
Rare special forms
Plaque form: Nonpigmented, plaque-forming lesions in young children
Nodular form: Brown nodules
Telangiectasia macularis eruptiva perstans (TMEP): Brown macules and erythema with telangiectasias on trunk and extremities
Blistering variant (“bullous mastocytosis”): Exaggeration of urticaria due to chymase cleaving dermal-epidermal junction
Diffuse CM
Diffusely thickened skin with “orange peel” appearance and yellow-red discoloration
No discernible individual lesions
In more severe variant, blistering may precede mast cell infiltration
Differential diagnosis with congenital bullous diseases
More likely associated with severe systemic symptoms (higher concentrations of mast cells)
GI manifestations (including severe diarrhea), hypotension, or even shock
Mastocytoma of skin
Single indurated red-brown macule, papule, plaque, or tumor measuring ≤ 4 cm in diameter
Multiple mastocytomas in different locations have been reported
Almost exclusively in infants
Slight predilection for trunk, but also occurs on extremities, head and neck
Systemic mastocytosis
Includes 6 distinct clinicohistopathologic entities
Symptoms grouped into few categories
Constitutional symptoms
Fatigue, weight loss, fever, diaphoresis
Skin manifestations
Pruritus, urticaria, dermographism
Mediator-related systemic events (due to release of histamine, eicosanoids, proteases, and heparin)
Same as CM systemic symptoms
Musculoskeletal complaints
Bone pain, osteopenia/osteoporosis, fractures, arthralgias, myalgias
Symptoms related to organ impairment due to mast cell infiltrates (absent in indolent but present in aggressive variants)
Splenomegaly (often minimal)
Lymphadenopathy and hepatomegaly (less frequent)
Hematological abnormalities
Anemia, leukocytosis, eosinophilia (frequent), neutropenia, and thrombocytopenia
BM failure only in aggressive or leukemic variants
Significant numbers of circulating mast cells are suggestive of MCL
30-40% of SM has associated clonal hematological non-mast cell lineage disease (AHNMD) diagnosed before, simultaneously with, or after SM diagnosis
Any defined myeloid or lymphoid malignancy possible, myeloid predominates (chronic myelomonocytic leukemia [CMML] most common)
Laboratory Tests
Serum total tryptase
Persistently elevated (> 20 ng/mL suggestive of SM, used as minor criterion for diagnosis)
Criterion not valid in SM-AHNMD
Normal to slightly elevated in patients with CM
Usually reserved for adult work-up of CM
Histamine
May be very elevated in diffuse CM, but are rarely part of routine work-up for CM
Treatment
CM
Alleviate symptoms with antihistamines and topical steroids
Prevent episodes by avoiding mast cell degranulators
Physical stimuli (temperature changes, rubbing/friction, intense physical exertion)
Foods (spicy foods, citrus fruits, cheese, alcohol)
Medications (antibiotics, aspirin, lidocaine, etc.)
Educate and reassure families
SM
Currently no cure
PKC412 tyrosine kinase inhibitor may be effective in treating SM with mutated KIT
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree