Table 21-1. Selected Drug Therapy Based on Guidelines for Use in ICU Patients
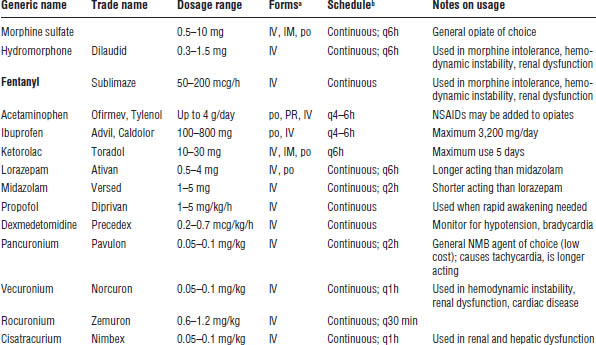
Boldface indicates one of top 100 drugs for 2012 by units sold at retail outlets, www.drugs.com/stats/top100/2012/units.
a. Long-acting drugs and dosage forms generally are not used in ICU (e.g., fentanyl patch, controlled-release morphine, doxacurium).
b. Continuous analgesia and sedation with frequent titration (patient-controlled analgesia pump, IV infusion, or scheduled) are preferred to prn therapy alone. NMB agents used prn are preferred.
Patient instructions
When patient-controlled analgesia pumps are used, make sure the patient understands how to activate the device.
Adverse drug events
■ Opiates, NSAIDs: See Chapter 27 on pain management.
■ Benzodiazepines, antipsychotics: See Chapter 29 on psychiatric disease.
■ Propofol (Diprivan): Adverse events include respiratory depression, hypotension, and hypertriglyceridemia. Propofol infusion syndrome (e.g., metabolic acidosis, rhabdomyolysis, and cardiac dysfunction) may occur at high doses (> 5 mg/kg/h for > 48 h). Thus, the maximum dose is 5 mg/kg/h.
■ Dexmedetomidine (Precedex): The most common adverse events are hypotension and bradycardia; however, respiratory depression is less likely than with other agents.
■ NMB agents: Adverse events include respiratory depression, prolonged weakness or paralysis after discontinuation, and tachycardia with pancuronium.
Drug interactions
■ Opiates, NSAIDs: See Chapter 27 on pain management.
■ Benzodiazepines, antipsychotics: See Chapter 29 on psychiatric disease.
■ Propofol (Diprivan), dexmedetomidine (Precedex): Actions are potentiated by other sedatives.
■ NMB agents: Actions are potentiated by corticosteroids, aminoglycosides, clindamycin, calcium channel blockers, and anesthetics; actions are inhibited by anticholinesterase inhibitors (e.g., neostigmine).
Parameters to monitor
■ Opiates, NSAIDs: Use self-reporting if possible, or BPS or CPOT if unable to communicate. Monitor vital signs, but do not use alone for assessment. Also see Chapter 27 on pain management.
■ Sedative agents: Use RASS or SAS. Monitor vital signs. Also see Chapter 29 on psychiatric disease. For propofol (Diprivan), also monitor serum triglycerides at baseline and one to two times per week during long-term use.
■ Antipsychotics: Use CAM-ICU or ICDSC. Also see Chapter 29 on psychiatric disease.
■ NMB agents: Monitor movement and breathing. Also monitor blood pressure (BP), heart rate (HR), and intracranial pressure (ICP) (acute increases may indicate suboptimal sedation or analgesia). Use peripheral nerve stimulation (“train of four” monitoring).
■ Note: In patients with continuous sedation, a daily awakening and assessment period results in decreased sedative use and a shorter length of stay in the ICU.
Kinetics
■ Opiates, NSAIDs: See Chapter 27 on pain management.
■ Benzodiazepines, antipsychotics: See Chapter 29 on psychiatric disease.
■ Propofol (Diprivan): Propofol is highly lipophilic (may accumulate over the long term), has a rapid onset (1 minute), and has a short duration (about 10 minutes). It is hepatically cleared.
■ Dexmedetomidine (Precedex): Dexmedetomidine is hepatically cleared and has a short onset (minutes) and half-life (about 2 hours).
■ NMB agents: Onset for all NMB agents is < 5 minutes. Duration is 60–90 minutes for pancuronium and 30–60 minutes for vecuronium and cisatracurium. Excretion of pancuronium is mostly renal; for vecuronium, it is about 50:50 (hepatic:renal). Excretion of cisatracurium is not organ dependent.
Other aspects
Propofol (Diprivan) is in a lipid vehicle that provides 1 kcal/mL. Avoid overfeeding. It should be used with caution in patients with egg allergy. It is a potential growth medium for bacteria; the maximum hang time for a bottle is 12 hours.
New IV formulations
Intravenous (IV) formulations of acetaminophen and ibuprofen are now available.
21-4. Traumatic Brain Injury
Definition
Traumatic brain injury (TBI) is defined as neurologic deficit secondary to brain trauma.
Classifications
■ Severe
■ Mild or moderate
Clinical Presentation
■ Use the Glasgow Coma Scale (GCS) for assessment: sum of eye, motor, and verbal scores (range 3 to 15).
■ TBI has a wide range of presentation from mild confusion to totally nonresponsive coma.
Pathophysiology
■ TBI results from motor vehicle accidents (most common), falls and accidents, assaults, and gunshot wounds. It is most common in the 15- to 24-year-old age group. Every year in the United States, there are 375,000 TBI cases and 75,000 deaths.
■ TBI consists of direct neuronal damage ± edema ± secondary ischemia-related neuronal death.
Diagnostic Criteria
■ The following are used for diagnosis: (1) computed tomography (CT) scan, (2) GCS, and (3) ICP monitoring in severe patients (GCS score 3–8).
Treatment Goals
■ Treatment goals include keeping ICP < 20 mm Hg and cerebral perfusion pressure (CPP) > 50 mm Hg (CPP = mean arterial pressure − ICP) and preventing seizures.
Strategies to decrease ICP
■ Osmotic agents and diuretics
• Mannitol 0.25–1 g/kg IV q4–6h
• Hypertonic NaCl IV (e.g., 3%, 7.5%) IV q4–6h
• Loop diuretics IV (e.g., furosemide)
• Short-acting agents are preferred to allow frequent patient assessment (e.g., propofol, fentanyl).
• Pentobarbital (1–3 mg/kg/h IV) is a long-acting agent for refractory intracranial hypertension.
■ NMB agents: A short-acting agent is preferred and is used only for refractory intracranial hypertension.
Nondrug interventions
■ Raising of the head of the bed (30 degrees)
■ Ventricular drainage of cerebrospinal fluid via ventriculostomy
■ Mild or moderate hyperventilation (pCO2 30–35 mm Hg)
■ Surgery
Strategies to increase mean arterial pressure
■ Maximize fluid status. The overall goal is euvolemia.
■ Vasopressors and inotropes may be used in shock after fluid status is optimized.
Seizure prevention
■ Seizure prevention may be started on the basis of severity and type of injury.
■ Phenytoin (Dilantin, generic) can be used: 20 mg/kg IV loading dose plus 4–8 mg/kg/day for 7 days.
• Continue beyond 7 days if the patient has a seizure after the immediate postinjury period.
• Alternative agents include levetiracetam (Keppra) or carbamazepine (limited data for both).
■ See Chapter 28 on seizure disorders for the mechanism of action, adverse drug events, drug interactions, and kinetics.
Parameters to monitor
The overall goal is CPP > 50 mm Hg and ICP < 20 mm Hg. Drug classes are covered elsewhere.
Other Aspects
Nimodipine (Nimotop) is a calcium channel blocker given for 21 days. It is indicated for treating aneurysmal subarachnoid hemorrhage. It may also provide some benefit in traumatic subarachnoid hemorrhage.
21-5. Acute Spinal Cord Injury
Note: High-dose methylprednisolone is no longer recommended for acute spinal cord injury.
21-6. Venous Thromboembolism Prophylaxis
Note: See Chapter 41 on thromboembolic disease.
21-7. Stress Ulcer Prophylaxis
Definition
Stress ulcer prophylaxis refers to gastrointestinal (GI) mucosal damage related to metabolic stress in the ICU.
Clinical Presentation
Presentation is similar to that of peptic ulcer disease (see Chapter 25 on gastrointestinal diseases).
Pathophysiology
Shunting of blood from the GI tract to vital organs during critical illness results in breakdown of gastric mucosal defenses (e.g., bicarbonate and mucus production, epithelial cell turnover).
Risk Factors
■ The primary risk factors are mechanical ventilation > 48 hours and coagulopathy.
■ Other risk factors include disease states or organ dysfunction where GI perfusion may be compromised (e.g., sepsis, burns, TBI, renal failure).
Diagnostic Criteria
Diagnosis is based on signs and symptoms and can be confirmed with endoscopy.
Treatment Goals
The goal is to prevent stress ulcers.
Drug Therapy
■ See Chapter 25 on gastrointestinal diseases for full drug information and treatment of ulcers that develop (stress ulcers are treated similarly to peptic ulcers). Patients in the ICU should be given stress ulcer prophylaxis if they have a risk factor listed above.
■ Proton pump inhibitors (PPIs) are a primary option. Most studies of stress ulcer prophylaxis have shown PPIs and histamine 2–receptor antagonists (H2RAs) to be equivalent; however, a recent meta-analysis suggests that PPIs are more effective. Thus, PPIs may be preferred, but this is still controversial. Another unresolved issue is concern about the association between outpatient use of PPIs with increased rates of community-acquired pneumonia and Clostridium difficile–associated diarrhea.
■ H2RAs are still widely considered to be a primary option. They are more effective than sucralfate for this indication and may have fewer epidemiological concerns than PPIs (see previous item).
■ Sucralfate is a secondary option that has fallen out of favor. It is less effective than H2RAs, is not available in IV form, and has significant drug-binding interactions.
■ Antacids are not recommended. They are less effective, have higher aspiration risk, and require frequent dosing.
■ Optimal duration of therapy is unknown. A reasonable approach is to discontinue prophylaxis when risk factors have resolved or upon transfer from the ICU.
21-8. Severe Sepsis and Septic Shock
Definition and Classifications
Severe sepsis is sepsis (see Chapter 33 on infectious disease) plus dysfunction of one or more major organs (e.g., hypotension responsive to fluids, oliguria, acute mental status change, lactic acidosis, respiratory insufficiency, coagulopathy).
Septic shock is severe sepsis plus hypotension that is not fully responsive to fluids (i.e., requires vasopressor therapy).
Clinical Presentation
See sepsis criteria (in Chapter 33) and the definitions of severe sepsis and septic shock.
Pathophysiology
Progression is seen in the systemic manifestations of sepsis. Imbalances in the inflammatory, immune, and coagulation systems lead to organ hypoperfusion and organ dysfunction with or without refractory hypotension. See Chapter 33 on infectious disease for typical causative organisms by site of infection.
Diagnostic Criteria
See sepsis criteria (in Chapter 33) and the definitions of severe sepsis and septic shock.
Treatment Goals
■ A primary treatment goal is to use “goal-directed therapy” to rapidly stabilize hemodynamic parameters (mean arterial pressure [MAP] > 65 mm Hg, urine output > 0.5 ml/kg/h) and reverse organ dysfunction and elevated serum lactate within 6 hours.
■ Concurrently, collect appropriate cultures based on the suspected site of infection, start appropriate antimicrobial therapy within 1 hour, and eliminate the source of infection if applicable (e.g., vascular or urinary catheter, abscess). The duration of antimicrobial therapy is typically 7–10 days depending on the site of infection and type of organism.
■ Modulate inflammatory, coagulation, and hormonal derangements if applicable.
Drug and Nondrug Therapy
See Chapter 33 on infectious disease for antimicrobial information (mechanism of action, dosing, adverse effects, etc.) and empiric antimicrobial selection. Definitive therapy should be streamlined to a narrower spectrum agent, if possible, on the basis of the final culture and sensitivity reports.
See Section 21-9 for details on fluid therapy. Initial fluid therapy for severe sepsis and septic shock should be 30 ml/kg of isotonic crystalloids (0.9% NaCl or lactated Ringer’s [LR] solution). Albumin can be given as a secondary fluid in patients requiring high doses of crystalloids. Other colloids (e.g., hetastarches) are no longer recommended because of the risk of acute kidney insufficiency. Vasopressors should be used only after appropriate fluid therapy fails to adequately normalize BP (Table 21-2). Inotropes can be used if cardiac index is poor following adequate fluid resuscitation.
Table 21-2. Vasopressorsa and Inotropes Used in Severe Sepsis and Septic Shock
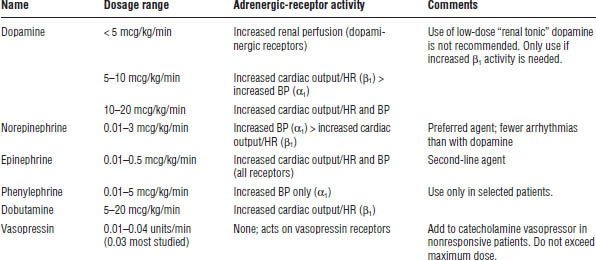
a. All catecholamine vasopressors are given as continuous IV infusions and are titrated to effect.
Mechanism of action
■ Vasopressors and inotropes are adrenergic-receptor agonists.
Adverse drug events
■ Vasopressors and inotropes: Adverse events include tachycardia, arrhythmias, organ and extremity ischemia, and hypertension. Norepinephrine causes fewer arrhythmias than dopamine. Thus, norepinephrine is now the preferred first-line vasopressor for most patients.
Drug–drug interactions
■ Vasopressors and inotropes: None
Parameters to monitor
■ Vasopressors and inotropes: Monitor BP, HR, cardiac output, urine output, and extremity perfusion on physical exam.
Other aspects
Hydrocortisone
Low-dose hydrocortisone (200 mg/day IV infusion × 7 days) is recommended for patients with septic shock who are not responsive to fluids and vasopressors. Patients with a poor response to cosyntropin stimulation testing (serum cortisol increase of < 9 mcg/dL) may respond better to corticosteroid supplementation. Hydrocortisone may be tapered sooner than day 7 of treatment if vasopressors are discontinued.
Vasopressin
Vasopressin infusion (0.03 units/min) may be used to increase BP in patients refractory to high doses of traditional vasopressors. Doses > 0.04 units/min are associated with severe adverse events (e.g., cardiac arrest). Patients receiving lower doses of catecholamine vasopressors (i.e., < 15 mcg/min of norepinephrine) may benefit more from vasopressin than do patients on higher doses of norepinephrine.
Prevention of ventilator-associated pneumonia
Oral chlorhexidine is suggested to reduce the risk of ventilator-associated pneumonia (VAP) in critically ill patients with severe sepsis or septic shock.
Miscellaneous therapies
The following therapies are not recommended in severe sepsis or critical illness: (1) treatment with selenium, immunoglobulins, or sodium bicarbonate (unless pH < 7.15), and (2) erythropoietin (unless already used for another indication).
21-9. Fluid and Electrolyte Abnormalities in Critically Ill Patients
See also Chapter 20 on kidney disorders (for hyperphosphatemia), Chapter 22 on nutrition, and Chapter 23 on oncology (for hypercalcemia).
Definition
Fluid and electrolyte abnormalities are pathologic alterations in fluid and electrolyte homeostasis.
Classifications
Fluid and electrolyte abnormalities are classified by electrolyte (see the discussion on clinical presentation).
Clinical Presentation
In all cases, mild to moderate abnormalities are usually asymptomatic.
Sodium (normal range: 135–145 mEq/L)
In cases of hyponatremia or hypernatremia, conditions including lethargy, nausea, headache, dry mucous membranes, poor skin turgor (depends on hydration status), and confusion may occur.
Coma, seizures, or central pontine myelinolysis may occur in severe hyponatremia or if sodium increases or decreases rapidly (> 12 mEq/L/day).
Chloride (normal range: 96–106 mEq/L)
Symptoms are related to acid–base or fluid abnormalities, not chloride itself.
Water (moves osmotically with sodium)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


