Creation of A Neoaortoiliac System (Nais Procedure) for the Treatment of Infected Aortic Grafts
G. Patrick Clagett
Introduction
In treating infected aortic grafts, the major goals are to save life and limb. These goals are best accomplished by eradicating infection and maintaining adequate circulation to portions of the body perfused by the infected aortic graft. Secondary goals include minimizing morbidity, restoration of normal function, and maintenance of long-term function without the need for reintervention and risk of amputation.
Before definitive reconstruction, all infected graft materials must be excised and grossly infected vascular tissues and surrounding soft tissues should be debrided aggressively. Once debridement is complete, there are several options for reconstruction, including (a) extra-anatomic bypass (axillofemoral bypass), (b) use of an arterial allograft, (c) placement of vascular prostheses treated with or soaked in antibiotic solutions, and (d) in situ replacement with a femoropopliteal vein (FPV) graft. For the sake of brevity, the latter procedure has been referred to as “creation of a neoaortoiliac system” or NAIS procedure.
All of these reconstructive approaches are valid and are appropriate depending upon patient-specific characteristics, extent and virulence of infection, and severity of vascular disease. It is a mistake to think that a single surgical approach is applicable to all patients with this condition. These are extraordinarily complex patients with varying levels of illness severity and they require individualized attention.
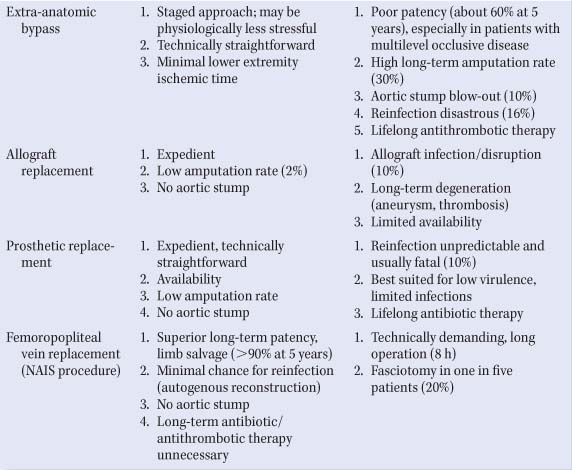
The pros and cons of each approach are presented in Table 1. From analysis of these considerations, the following features help to determine the choice of reconstructive procedure. Extra-anatomic bypass is a good option for the treatment of an infected aortic graft when groin infection is absent and lower extremity runoff is good. For example, extra-anatomic bypass would be an excellent choice in a patient with an infected aortoiliac graft. The disadvantages of this approach are that long-term patency is poor and that there is a significant risk of reinfection of the extra-anatomic bypass. In addition, if groin infection is present, the bypass is compromised even further by the need to use vessels such as the profunda femoris artery or the popliteal artery for distal targets. Because of these factors,
durability is limited despite aggressive antithrombotic therapy.
durability is limited despite aggressive antithrombotic therapy.
Table 1 Treatment Options for Aortic Graft Infections | |
|---|---|
|
Extra-anatomic bypasses are plagued by sudden thrombotic occlusion and amputation rates are high. Reinfection is also a major concern, which occurs in 10% to 20% of such patients, and often proves fatal. A final concern in patients undergoing extra-anatomic bypass is the possibility of lethal aortic stump blowout, which occurs in approximately 10% of these patients.
In situ aortic allograft and antibiotic-treated prosthetic graft replacement have the advantages of being expedient and technically straightforward with low amputation rates. These reconstructions are a good choice in patients who are unstable, for example, patients with actively bleeding aortoenteric fistulas. A major drawback of using allografts and antibiotic-treated prosthetic grafts is that reinfection may occur and often proves fatal. For this reason, these approaches should probably be reserved for graft infections of low virulence and limited anatomic extent. Aortic allografts are also subject to long-term complications, such as aneurysm dilation, late allograft rupture, and thrombosis.
The NAIS reconstruction using FPV grafts was developed because of the limitations of the other approaches. FPV grafts have excellent long-term patency and are resistant to reinfection. In addition, they are ideal conduits for patients with extensive multilevel occlusive disease, in whom venous grafts theoretically would have better patency than prosthetic grafts. Individuals with extensive occlusive vascular disease are the most commonly encountered patients with infected aortic grafts in our practice. They frequently have infected aortobifemoral bypass grafts and septic groins. The superior durability of the NAIS reconstruction translates into correspondingly low long-term amputation rates. In addition, these patients do not require treatment with lifelong anticoagulant and antibiotic therapy.
The main disadvantage of the NAIS reconstruction is that the procedure is time-consuming and technically demanding. The mean operating time is 8 hours, and the lower extremity ischemic time is longer than that of patients undergoing the other reconstructive approaches. An additional disadvantage of using FPV grafts is the associated short-term venous morbidity. Approximately 20% of patients who undergo FPV harvesting will require leg fasciotomy. The fasciotomy rate is highest in patients who undergo concurrent greater saphenous vein harvesting, and in those who have severe, preexisting lower extremity ischemia (ankle/brachial index of <0.4). Despite this, long-term venous morbidity is gratifyingly low with no known cases of venous ulceration or venous claudication.
The preoperative workup should assess the extent of infection and anatomic location of concomitant occlusive disease (indicating a possible need for additional infrainguinal reconstruction), and determine whether there are associated infectious complications that must be treated (e.g., a psoas abscess or duodenal erosion necessitating duodenal repair). In patients who have previously undergone prosthetic aortobifemoral bypass, infection may be limited to one limb of the graft, and it may be treated by replacing only that limb. In patients who have previously undergone prosthetic infrainguinal bypass, the bypass graft, if infected, will have to be removed and replaced with an autogenous graft.
In the past, the mainstay of the preoperative workup was arteriography complemented by computed tomography (CT), but currently, the workup is increasingly being performed with a CT angiography alone. CT angiography is often capable of evaluating the extent of infection, visualizing the sites of previous prosthetic anastomoses, and delineating the arterial anatomy. Magnetic resonance angiography can also be a helpful adjunct, particularly in patients with renal insufficiency.
Noninvasive vascular laboratory workup consists of ankle/brachial indices, toe systolic blood pressures, aortic and femoral duplex ultrasonography, and venous duplex ultrasonography. Low ankle/brachial indices (<0.4) and toe pressures (<40 mm Hg) may indicate the need for additional infrainguinal bypass and may also portend the need for leg fasciotomy. Aortic and femoral duplex ultrasonography helps to determine the extent of infection. We have found that a hypoechoic rim around the femoral limbs of aortic grafts (“halo sign”) is pathognomonic for infectious involvement. Likewise, absence of a halo sign may indicate that the femoral limb is not infected.
Venous duplex ultrasonography is essential in planning an NAIS reconstruction. Examination of the lower extremity venous system establishes the diameter and available length of the deep veins. In addition, duplex ultrasonography can evaluate acute or chronic thrombosis, recanalization changes, the congenital absence, or duplication of venous segments and unusually small deep veins. When the FPV is small
(<5 mm), absent, or incomplete, a dominant profunda femoris vein is usually present. This vein is located posteriorly in the thigh and connects with the popliteal vein. This can also be used as a venous autograft. Duplex vein mapping of the greater saphenous system is also routinely performed and may provide useful information in the event that concomitant infrainguinal reconstruction is planned or may have to be performed unexpectedly.
(<5 mm), absent, or incomplete, a dominant profunda femoris vein is usually present. This vein is located posteriorly in the thigh and connects with the popliteal vein. This can also be used as a venous autograft. Duplex vein mapping of the greater saphenous system is also routinely performed and may provide useful information in the event that concomitant infrainguinal reconstruction is planned or may have to be performed unexpectedly.
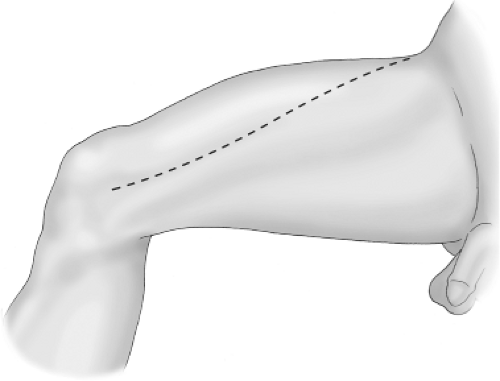 Fig. 1. The thigh incision is lateral to the border of the sartorius muscle extending from the anterior superior iliac spine to the medial femoral condyle. |
Anesthetic Considerations
Removal of an infected aortic graft and autogenous reconstruction requires prolonged exposure of large portions of the body with extensive incisions and dissections in the trunk and lower extremities. Significant drops in core body temperature are frequent and when combined with blood loss and resuscitation, may potentiate metabolic acidosis, cardiac arrhythmia, coagulopathy, and immune compromise. Aggressive maintenance of core body temperature above 36ºC is facilitated by applying heated-air warming blankets to the upper body, using warmed fluids for resuscitation, and maintaining a warm ambient temperature in the operating room.
Fluid management should be judicious to maintain adequate urinary output. Overzealous crystalloid infusions have been identified as an independent predictor of the need for fasciotomy (most likely due to potentiating muscle edema) and the development of postoperative congestive heart failure. The threshold for blood and colloid replacement should be low, since virtually all of these patients will require transfusion. In addition, fresh frozen plasma and platelets should be available in the event that coagulopathy develops.
The NAIS procedure is sequenced in major steps designed to minimize lower extremity ischemia time and the time that the abdomen is opened when temperature and insensible fluid losses are significant. The sequence is as follows: (a) dissection of FPVs, which are left in situ until needed; (b) isolation and control of the femoral vessels; (c) entry into the abdomen and dissection and control of the aorta above the anastomotic site (may involve suprarenal dissection); (d) removal and preparation of measured lengths of FPVs that will be required for the reconstruction; (e) application of aortic and femoral cross-clamps with removal of the infected prosthesis; and (f) reconstruction with FPV grafts.
Thigh Incision and Exposure of Femoral Vessels
The patient is placed in the supine position with the legs “frog legged” and supported under the thighs. An incision is made on the thigh along the lateral border of the sartorius muscle (Fig. 1). This incision extends from the anterior superior iliac spine to the medial femoral condyle. The lateral incision not only facilitates vein harvesting, but also allows exposure of the femoral vessels while avoiding the infected femoral wound located more medially.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree