Chapter 12 Cranial Nerve Innervation of Ocular Structures
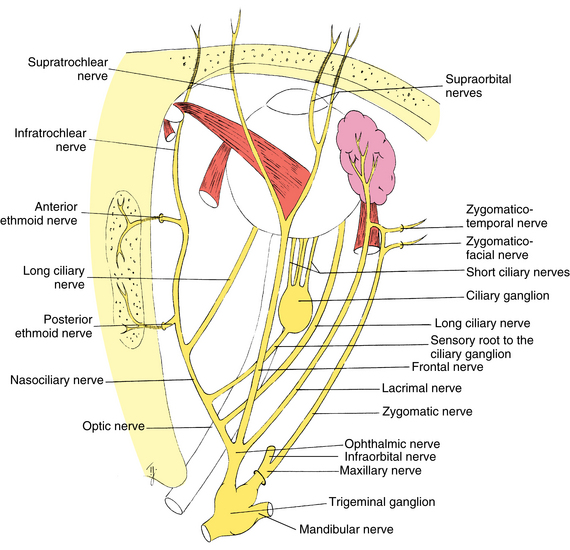
The orbital structures are innervated by cranial nerves (CNs) II, III, IV, V, VI, and VII (Table 12-1). Motor functions of the striated muscles are controlled by CN III, the oculomotor nerve; CN IV, the trochlear nerve; CN VI, the abducens nerve; and CN VII, the facial nerve. CN V, the trigeminal nerve, carries the sensory supply from the orbital structures. CN II, the optic nerve, carries visual information and is discussed in Chapter 13. This chapter discusses sensory and motor innervation of the orbit, including pathways, functions, and presenting signs of dysfunction.
The Nervous System
Efferent fibers, either somatic or autonomic, carry information from the CNS to the target structures: muscles, organs, or glands. The efferent pathway in the somatic system generally consists of a fiber that runs the distance from the CNS to the target muscle. The autonomic pathway generally has a synapse within its efferent pathway (see Chapter 14).
Afferent Pathway: Orbital Sensory Innervation
The eye is richly supplied with sensory nerves that carry sensations of touch, pressure, warmth, cold, and pain. Sensations from the cornea, iris, conjunctiva, and sclera consist primarily of pain; even light touching of the cornea is registered as irritation or pain.1
Trigeminal Nerve
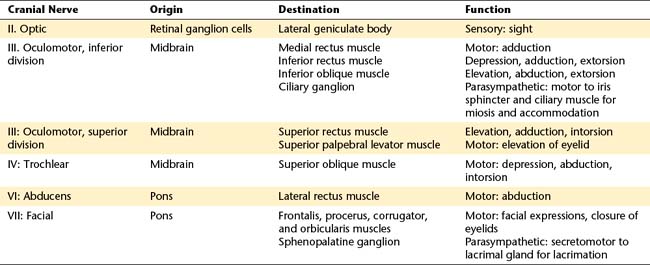
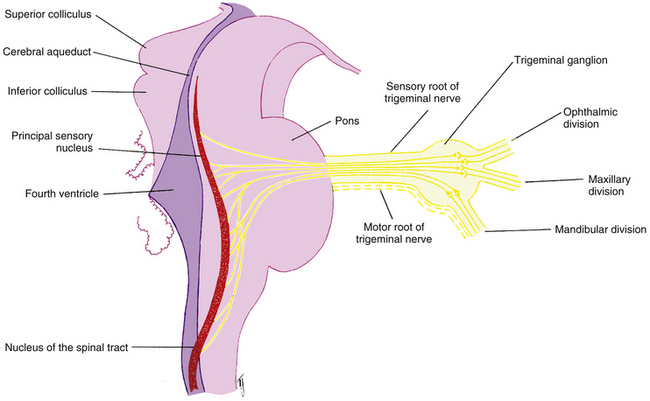
The fibers of the trigeminal nerve (CN V) serving ocular structures are sensory and originate in the innervated structures. The description of the pathways of these nerves begins at the involved structures and follows the nerves as they join to become larger nerves, come together in the ganglion of the fifth cranial nerve, and then exit the ganglion and enter the pons. It is hoped that this presentation, although unconventional, will enable the reader to keep in mind the actual direction of the action potential, and thus the information flow, in these fibers. Figure 12-1 shows the major branches and paths of the trigeminal nerve within the orbit.
Ophthalmic Division of Trigeminal Nerve
Nasociliary Nerve
Sensory fibers from the structures of the medial canthal area—caruncle, canaliculi, lacrimal sac, medial aspect of the eyelids, and skin at the side of the nose —join to form the infratrochlear nerve. This nerve penetrates the orbital septum, enters the orbit below the trochlea, and runs along the upper border of the medial rectus muscle, becoming the nasociliary nerve as other branches join it (see Figure 12-1).
Sensory fibers from the skin along the center of the nose, the nasal mucosa, and the ethmoid sinuses form the anterior ethmoid nerve; fibers from the ethmoid sinuses and the sphenoid sinus form the posterior ethmoid nerve. The ethmoid nerves enter the orbit with their companion arteries through foramina within the frontoethmoid suture.2 Both nerves join the nasociliary nerve as it runs along the medial aspect of the orbit (see Figure 12-1).
Corneal sensory innervation is dense, estimated to be 400 times as dense as other epithelial tissue innervation.3 Three networks of nerves are formed. One is located in the corneal epithelium, another (the subepithelial plexus) is in the anterior stroma, and the third, the stromal plexus, is in the middle of the stroma4 (Figure 12-2). No nerves are found in posterior stroma, Descemet’s membrane, or endothelium. The fibers from these plexus come together in peripheral stroma and radiate out into the limbus as 70 to 80 branches; they become myelinated in the last 2 mm of the cornea.5–7
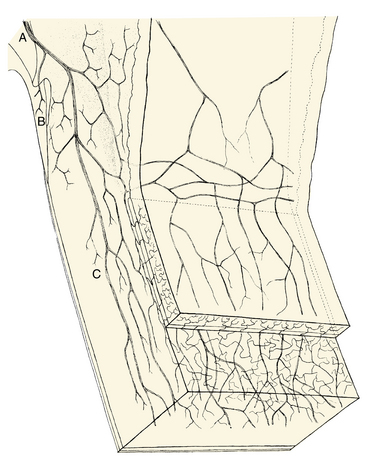
FIGURE 12-2 Innervation of limbus and cornea.
(From Hogan MJ, Alvarado JA, Weddell JE, editors: Histology of the human eye, Philadelphia, 1971, Saunders.)
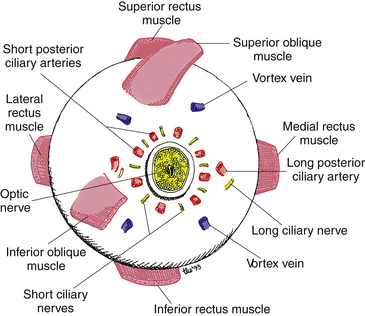
Some of these branches join with nerves from other anterior segment structures to form two long ciliary nerves. These long ciliary nerves, one on the lateral side and one on the medial side of the globe, course between the choroid and sclera to the back of the eye, where they leave the globe at points approximately 3 mm on each side of the optic nerve (Figure 12-3). (In addition to afferent fibers, the long ciliary nerves transmit sympathetic fibers to the dilator muscle of the iris.) The two long ciliary nerves then join the nasociliary nerve.
Clinical Comment: (Scleral) Nerve Loops (of Axenfeld)
A slight variation can occur in the pathway of the long ciliary nerve in which the fibers loop into the sclera from the suprachoroidal space, forming a dome-shaped elevation about 2 mm from the limbus on either the nasal or the temporal side. Often this raised area is pigmented, usually blue or black, and should be differentiated from a melanoma.8 The nerve loop may be painful when touched, a characteristic that should aid in its diagnosis.5
The other branches radiating from the cornea into the limbus join other sensory nerves from the anterior segment; they enter the choroid, join with the choroidal nerves, then course to the back of the eye, where they leave as 6 to 10 short ciliary nerves (see Figure 12-3). The short ciliary nerves exit the sclera in a ring around the optic nerve in company with the short posterior ciliary arteries and enter the ciliary ganglion (see Figure 12-1). The sensory fibers do not synapse but pass through the ganglion, leaving as the sensory root of the ciliary ganglion, which then joins the nasociliary nerve. (The short ciliary nerves carry sympathetic and parasympathetic fibers in addition to sensory fibers.)
Thus, the nasociliary nerve is formed by the joining of the infratrochlear nerve, the anterior and posterior ethmoid nerves, the long ciliary nerves, and the sensory root of the ciliary ganglion (see Figure 12-1). The nasociliary nerve exits the orbit by passing through the oculomotor foramen within the common tendinous ring and the superior orbital fissure into the cranial cavity.
Clinical Comment: Herpes Zoster
HERPES ZOSTER is an acute CNS infection caused by the varicella-zoster virus. Signs and symptoms include pain and rash in the distribution area supplied by the affected sensory nerves.9 It is believed that the virus lies dormant in a sensory ganglion and, on becoming activated, migrates down the sensory pathway to the skin.10 An eruption of herpes zoster is more common in elderly persons but may occur at any age and may be related to a delayed hypersensitivity reaction.11 Approximately 10% of all cases affect the ophthalmic division of the trigeminal nerve.12 Involvement of the tip of the nose often indicates that the eye will also be involved, reflecting the distribution of the nasociliary branches. This association of ocular involvement with zoster affecting the tip of the nose is the Hutchinson sign.13
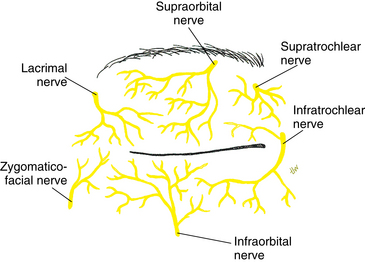
Frontal Nerve
Sensory fibers from the skin and muscles of the forehead and upper eyelid come together and form the supratrochlear nerve. This nerve enters the orbit by piercing the superior medial corner of the orbital septum (Figure 12-4).
Sensory fibers from the skin and muscles of the forehead and upper eyelid form a second nerve, the supraorbital nerve, lateral to the supratrochlear nerve. The supraorbital nerve enters the orbit as one or two branches: one branch enters through the supraorbital notch, accompanying the supraorbital artery. The supraorbital nerve joins the supratrochlear nerve midway in the orbit and forms the frontal nerve (see Figure 12-1). The frontal nerve courses back through the orbit between the levator muscle and the periorbita, exiting the orbit through the superior orbital fissure above the common tendinous ring.
Lacrimal Nerve
Sensory fibers from the lateral aspect of the upper eyelid and temple area come together and enter the lacrimal gland; they join the sensory fibers that serve the gland itself to form the lacrimal nerve. The lacrimal nerve leaves the gland and runs posteriorly along the upper border of the lateral rectus muscle (see Figure 12-1). It receives a branch from the zygomatic nerve containing the autonomic innervation of the lacrimal gland. The lacrimal nerve exits the orbit through the superior orbital fissure above the muscle cone.
Ophthalmic Nerve Formation
After exiting the orbit, the nasociliary nerve, the lacrimal nerve, and the frontal nerve join and form the ophthalmic division of the trigeminal nerve (see Figure 12-1). The ophthalmic nerve then enters the lateral wall of the cavernous sinus, coursing between the two dural layers.14 While in the wall of the sinus the nerve receives sensory fibers from the oculomotor, trochlear, and abducens nerves. Some of these fibers probably carry proprioceptive information from the extraocular muscles.15
Maxillary Division of Trigeminal Nerve
Infraorbital Nerve
The infraorbital nerve, formed by sensory fibers from the cheek, upper lip, and lower eyelid, enters the maxillary bone through the infraorbital foramen (Figure 12-5). It runs posteriorly through the infraorbital canal and groove; while it is in the maxillary bone, branches join from the upper teeth and maxillary sinus. As the nerve leaves the infraorbital groove it exits the orbit through the inferior orbital fissure and joins other fibers in forming the maxillary nerve.
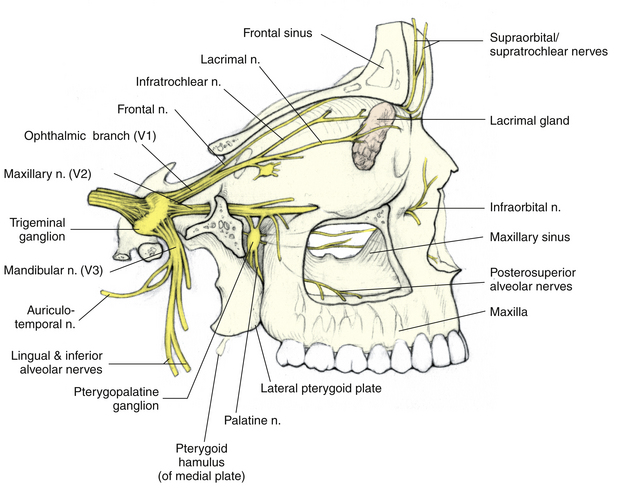
FIGURE 12-5 Three divisions of trigeminal nerve.
(From Mathers LH, Chase RA, Dolph J, et al: Clinical anatomy principles, St Louis, 1996, Mosby.)
Clinical Comment: Referred Pain
REFERRED PAIN is pain felt in an area remote from the actual site of involvement; however, the two areas usually are connected by a sensory nerve network. Frequently, the pathways of the trigeminal nerve are involved in referred pain. A common example is a momentary severe bilateral frontal headache sometimes experienced when an individual eats ice cream.5 An abscessed tooth can cause pain described by a patient as ocular pain and should be suspected when no orbital cause for the pain can be found. This situation likely occurs because the overload of sensation carried by the infraorbital nerve from the upper teeth is interpreted by the brain as coming from another area also served by the trigeminal nerve.
Zygomatic Nerve
Sensory fibers from the lateral aspect of the forehead enter the orbit through a foramen in the zygomatic bone as the zygomaticotemporal nerve. Fibers from the lateral aspect of the cheek and lower eyelid enter the orbit through a foramen in the zygomatic bone as the zygomaticofacial nerve.13 These two nerves join to become the zygomatic nerve and course along the lateral orbital wall, exiting the orbit through the inferior orbital fissure and joining with the maxillary nerve (see Figure 12-1).
Maxillary Nerve Formation
Having been formed by the joining of the infraorbital nerve, the zygomatic nerve, and nerves from the roof of the mouth, upper teeth and gums, and mucous membranes of the cheek, the maxillary nerve traverses the area between the maxilla and the sphenoid bone. As it passes near the pterygopalatine fossa, it receives some autonomic fibers from the pterygopalatine ganglion (see Figure 12-5). (These autonomic fibers are destined for the lacrimal gland and are discussed in Chapter 14.) The maxillary nerve enters the skull through the foramen rotundum.
Trigeminal Nerve Formation
As the ophthalmic and maxillary divisions enter the skull, they run posteriorly within the lateral wall of the cavernous sinus (Figure 12-6).16,17 The mandibular division lies just below the cavernous sinus. The sensory fibers from the three divisions enter the trigeminal ganglion (gasserian ganglion, semilunar ganglion), where they synapse. The ganglion, flattened and semilunar in shape, is located lateral to the internal carotid artery and the posterior portion of the cavernous sinus. The motor fibers of the mandibular division, which innervate the muscles of mastication, pass along the lower edge of the ganglion.18 Only the sensory fibers synapse within the ganglion.

FIGURE 12-6 Detailed cross section of cavernous sinus.
(From Mathers LH, Chase RA, Dolph J, et al: Clinical anatomy principles, St Louis, 1996, Mosby.)
The fibers leave the trigeminal ganglion and enter the lateral aspect of the pons as either the sensory root or the motor root of the trigeminal nerve. The sensory root carries information from the structures of the face and head, including all orbital structures. After entering the brain stem, these fibers form an ascending and a descending tract, both terminating in sensory nuclei of the trigeminal nerve (Figure 12-7). The ascending tract terminates in the principal sensory nucleus in the pons; it registers the sensations of touch and pressure.1 The descending tract, which carries pain and temperature sensations, courses through the pons and medulla to the elongated nucleus of the spinal tract.1 The tract extends into the second cervical segment of the spinal cord.19 Information from the trigeminal nuclei is relayed to the thalamus.
Clinical Comment: Oculocardiac Reflex
THE OCULOCARDIAC REFLEX consists of bradycardia (slowed heartbeat), nausea, and faintness and can be elicited by pressure on the globe or stretch on the extraocular muscles (e.g., during ocular surgery).20–22 Fibers from the trigeminal spinal nucleus project into the reticular formation near the vagus nerve nuclei and can activate vagus synapses, precipitating this reflex. The motor aspect of the reflex can be blocked by retrobulbar anesthesia or intravenous or intramuscular atropine.1,13,
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree