20 Coronary heart disease
CHD kills over 6.5 million people worldwide each year.
Epidemiology
The UK has seen a steady decline in deaths from CHD of about 4.5% per annum since the late 1970s. A recent study indicated that both reductions in major risk factors and improvements in treatment have contributed to this reduction (Unal et al., 2004). While impressive, this rate of decline has not been as great as in other countries like Australia and Finland. In Eastern European countries, the death rates from CHD have increased significantly during the same period.
Risk factors
Traditionally, the main potentially modifiable risk factors for CHD have been considered to be hypertension, cigarette smoking, raised serum cholesterol and diabetes. More recently psychological stress and abdominal obesity have gained increased prominence (Box 20.1). Patients with a combination of all these risk factors are at risk of suffering a myocardial infarction some 500 times greater than individuals without any of the risk factors. Stopping smoking, moderating alcohol intake, regular exercise and consumption of fresh fruit and vegetables were associated independently and additively with reduction in the risk of having a myocardial infarction.
Aetiology
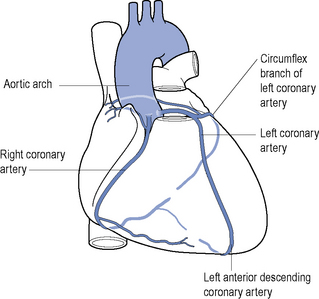
The vast majority of CHD occurs in patients with atherosclerosis of the coronary arteries (see Fig. 20.1) that starts before adulthood. The cause of spontaneous artherosclerosis is unclear, although it is thought that in the presence of hypercholesterolaemia, a non-denuding form of injury occurs to the endothelial lining of coronary arteries and other vessels. This injury is followed by subendothelial migration of monocytes and the accumulation of fatty streaks containing lipid-rich macrophages and T-cells. Almost all adults, and 50% of children aged 11–14 years, have fatty streaks in their coronary arteries. Thereafter, there is migration and proliferation of smooth muscle cells into the intima with further lipid deposition. The smooth muscle cells, together with fibroblasts, synthesise and secrete collagen, proteoglycans, elastin and glycoproteins that make up a fibrous cap surrounding cells and necrotic tissue, together called a plaque. The presence of atherosclerotic plaques results in narrowing of vessels and a reduction in blood flow and a decrease in the ability of the coronary vasculature to dilate and this may become manifest as angina. Associated with the plaque rupture is a loss of endothelium. This can serve as a stimulus for the formation of a thrombus and result in more acute manifestations of CHD, including unstable angina (UA) and myocardial infarction. Plaque rupture caused by physical stresses or plaque erosion may precipitate an acute reaction. Other pathological processes are probably involved, including endothelial dysfunction which alters the fibrin–fibrinolysis balance and the vasoconstriction–vasodilation balance. There is interest in the role of statins and angiotensin-converting enzyme (ACE) inhibitors in modifying endothelial function.
Measurement of acute phase inflammatory reactions, such as fibrinogen and CRP, has a predictive association with coronary events. High-sensitivity CRP assays have been used in populations without acute illness to stratify individuals into high-, medium- and low-risk groups. In patients with other risk factors, however, CRP adds little prognostic information. CRP is produced by atheroma, in addition to the major producer which is the liver, and is an inflammatory agent as well as a marker of inflammation. Evidence is emerging that drug therapy which reduces CRP in otherwise healthy individuals reduces the incidence of major cardiac events (Ridker, 2008).
Modification of risk factors
Common to all stages of CHD treatment is the need to reduce risk factors (Table 20.1). The patient needs to appreciate the value of the proposed strategy and to be committed to a plan for changing their lifestyle and habits, which may not be easy to achieve after years of smoking or eating a particular diet. Preventing CHD is important but neither instant nor spectacular. It may require many sessions of counseling over several years to initiate and maintain healthy habits. It may also involve persuasion of patients to continue taking medication for asymptomatic disorders such as hypertension or hyperlipidaemia. The general public, with government as its agent, need to agree that a reduction in the incidence of CHD is worth some general changes in lifestyle or liberty, for example, such as prohibiting the freedom to smoke in public. National campaigns to encourage healthy eating or exercise are expensive, as is the long-term medical treatment of hypertension or hyperlipidaemia, and such strategies must have the backing of governments to succeed. It has been argued that community-wide campaigns on cholesterol reduction have had measurable benefits in Finland, the USA and elsewhere, at least in high-risk, well-educated and affluent groups. It follows that the next challenge is to extend that success to poorer, ethnically diverse groups and to those portions of the population with mild-to-moderate risk.
Table 20.1 Effect of interventions on risk of myocardial infarction
| Intervention | Control | Benefit of intervention |
|---|---|---|
| Stopping smoking for ≥5 years | Current smokers | 50–70% lower risk |
| Reducing serum cholesterol | 2% lower risk for each 1% reduction in cholesterol | |
| Treatment of hypertension | 2–3% lower risk for each 1 mmHg decrease in diastolic pressure | |
| Active lifestyle | Sedentary lifestyle | 45% lower risk |
| Mild to moderate alcohol consumption (approx. 1 unit/day) | Total abstainers | 25–45% lower risk |
| Low-dose aspirin | Non-users | 33% lower risk in men |
| Postmenopausal oestrogen replacement | Non-users | 44% lower risk |
The quality of data associated with these interventions varies greatly and figures may not apply to all patient groups.
Clinical syndromes
Stable angina
Treatment of stable angina is based on two principles:
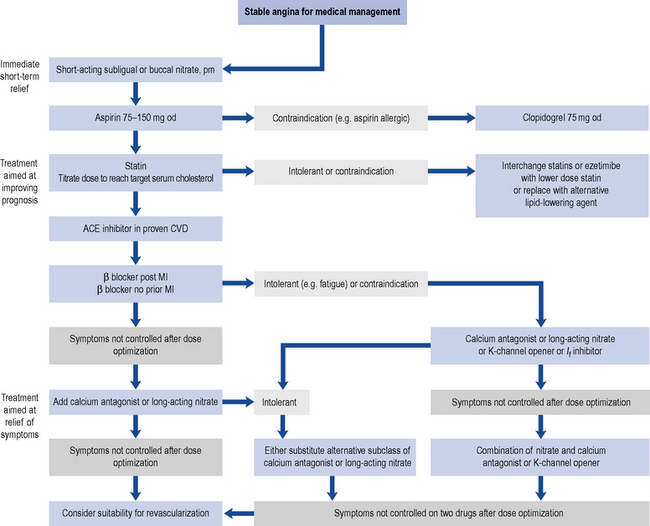
Pharmacological therapy can be considered a viable alternative to invasive strategies, providing similar results without the complications associated with percutaneous coronary intervention (PCI). An algorithm for addressing both these principles is outlined in Fig. 20.2. In addition, diabetes, hypertension and dyslipidaemia in patients with stable angina should be well controlled. Smoking cessation, without or with pharmacological support, and weight loss should be attempted.
Antithrombotic drugs
Clopidogrel
Clopidogrel inhibits ADP activation of platelets and is useful as an alternative to aspirin in patients who are allergic or cannot tolerate aspirin. Data from one major trial (CAPRIE Steering Committee, 1996) indicate that clopidogrel is at least as effective as aspirin in patients with stable coronary disease. The usual dose is 300 mg once, then 75 mg daily. Although less likely to cause gastric erosion and ulceration, gastro-intestinal bleeding is still a major complication of clopidogrel therapy. There is evidence that the combination of a proton pump inhibitor and aspirin is as effective as using clopidogrel alone in patients with a history of upper gastro-intestinal bleeding.
COX-2 inhibitors
The analgesic and anti-inflammatory action of non-steroidal anti-inflammatory drugs (NSAIDs) is believed to depend mainly on their inhibition of COX-2, and the unwanted gastro-intestinal effects of NSAIDs on their inhibition of COX-1. COX-2 inhibition reduces the production of prostacyclin, which has vasodilatory and platelet-inhibiting effects. Studies have raised concern about the cardiovascular safety of NSAIDs. Initially, the concern was focussed on the selective cyclo-oxygenase-2 inhibitors and a link to an increased cardiovascular risk. Recently, evidence has shown the more traditional non-selective NSAIDs increase cardiovascular risk in both patients with established CVD and in the healthy population (Fosbol et al., 2010). NSAIDs with high COX-2 specificity increase the risk of myocardial infarction and should be avoided where possible in patients with stable angina.
ACE inhibitors
The use of ACE inhibitors in patients without myocardial infarction or left ventricular damage is based on two trials: the HOPE study (Yusuf et al., 2000) which studied ramipril and the EUROPA (2003) study which used perindopril. These trials also identified an incidental delay in the onset of diabetes mellitus in susceptible individuals which may be of long-term benefit to them. The HOPE study, a secondary prevention trial, investigated the effect of an ACE inhibitor on patients over 55 years old who had known atherosclerotic disease or diabetes plus one other cardiovascular risk factor. The use of ramipril decreased the combined endpoint of stroke, myocardial infarction or cardiovascular death by approximately 22%. The benefits were independent of blood pressure reduction. This has major implications for the management of CHD patients, both for the decision to treat all and the choice of treatment. At present the use of ACE inhibitors in patients with coronary disease, but without myocardial infarction, has general acceptance and is recommended in European guidelines.
Statins
Earlier studies focused on patients with ‘elevated’ cholesterol, but all patients with coronary risk factors benefit from reduction of their serum cholesterol level. It is now clear that there is no ‘safe’ level of cholesterol for patients with CAD and that there is a continuum of risk down to very low cholesterol levels. Levels of LDL-C of <2 mmol/L and total cholesterol <4 mmol/L are recommended for patients with established CVD (NICE, 2008). Statins should be prescribed alongside lifestyle advice for both primary prevention of CVD and in those with established CVD (see Chapter 24 for more detail).
Symptom relief and prevention
β-Blockers
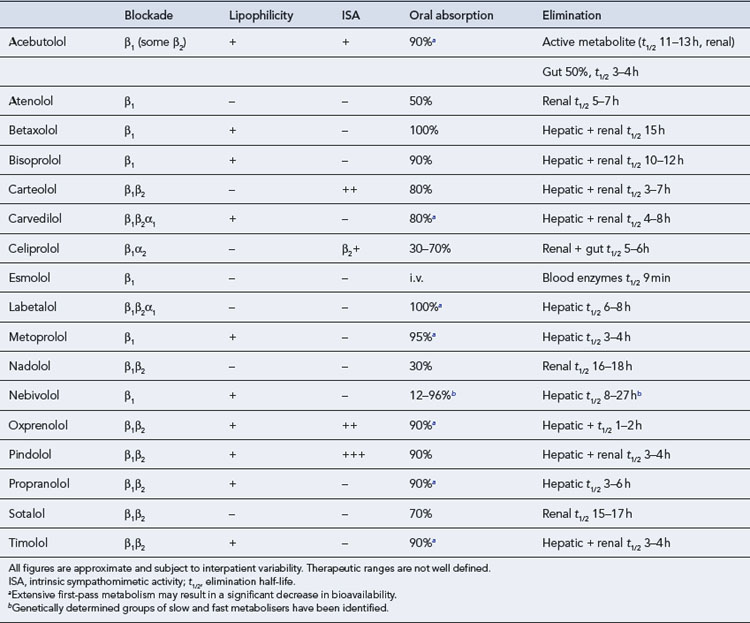
All β-blockers tend to reduce renal blood flow, but this is only important in renal impairment. Drugs eliminated by the kidney (Table 20.2) may need to be given at lower doses in the renally impaired or in the elderly, who are particularly susceptible to the CNS-mediated lassitude. Drugs eliminated by the liver have a number of theoretical interactions with other agents that affect liver blood flow or metabolic rate, but these are rarely of clinical significance since the dose should be titrated to the effect. Likewise, although there is theoretical support for the use of agents with high intrinsic sympathomimetic activity (ISA) to reduce the incidence or severity of drug-induced heart failure, there is no β-blocker that is free from this problem, and clinical trials of drugs with ISA have generally failed to show any extra benefit.