http://evolve.elsevier.com/Edmunds/NP/
 Key drug. Sublingual nitroglycerin is selected as the key drug because it is the simplest form of the drug.
Key drug. Sublingual nitroglycerin is selected as the key drug because it is the simplest form of the drug.
Patients with a history of angina should have sublingual nitroglycerin (NTG) available, and they should know how to use it. Medications other than nitrates used to treat coronary artery disease (CAD) include β-blockers (BBs), calcium channel blockers (CCBs), angiotensin-converting enzyme inhibitors (ACEIs), ACE II inhibitors (ARBs), and antihyperlipidemics. Ranolazine is used in combination with some of these agents for patients with chronic angina. Use of these agents in the treatment of CAD is discussed here. Details on individual drugs are discussed in their respective chapters (Table 18-1).
TABLE 18-1
Drugs Used for Coronary Artery Disease Discussed in Other Chapters
| Class | Chapter |
| β-Blockers | 20 |
| Calcium channel blockers | 21 |
| ACE inhibitors | 22 |
| ACE II inhibitors | 22 |
| Antihyperlipidemics | 24 |
Although the traditional recommendation is for patients to take up to 3 SL nitroglycerin doses over 15 minutes before accessing the emergency system, recent guidelines suggest an alternative strategy to reduce delays in emergency care. The 2004 ACC/AHA STEMI myocardial infarction guidelines recommend instructing a patient with a prior prescription for nitroglycerin to call 9-1-1 immediately if chest discomfort/pain is persistent or worsened 5 minutes after ONE dose of nitroglycerin. Self-treatment with nitrates has been identified as a factor resulting in delaying access to emergency care for patients with STEMI, including those with a history of MI or angina. The STEMI guidelines also note that for patients known to have frequent angina, physicians may provide individualized instructions for the use of SL nitroglycerin, based on the characteristics of the patient’s angina, time course, and response to treatment. The guidelines stress the importance of preventing delays in emergency evaluation due to self-medication. The patient should also chew a regular 325-mg aspirin on the way to emergency care.
Therapeutic Overview of Coronary Artery Disease
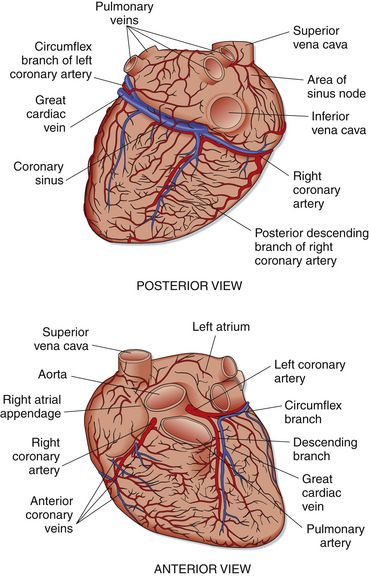
The myocardium receives its blood supply from the coronary arteries, a system of small arteries that branch from the aorta (Figure 18-1). The right coronary artery lies in a groove between the right atrium and the right ventricle and supplies the right ventricle. The left main coronary artery is divided shortly after its origin into two branches: the left anterior descending branch and the circumflex branch. The left anterior descending branch supplies blood to the anterior myocardium, apex, and anterior septum and is located on the surface of the anterior myocardium. The circumflex branch lies in a groove between the left atrium and the left ventricle and supplies blood to the left ventricle. Smaller branches arise from the large coronary vessels. In 90% of the population, a posterior descending artery arises from the right coronary artery, and in 10%, it arises from the circumflex branch of the left anterior descending artery.
Pathophysiology
Determinants in the pathogenesis of MI include atheromatous lesions, increased myocardial oxygen demand, and catecholamine release.
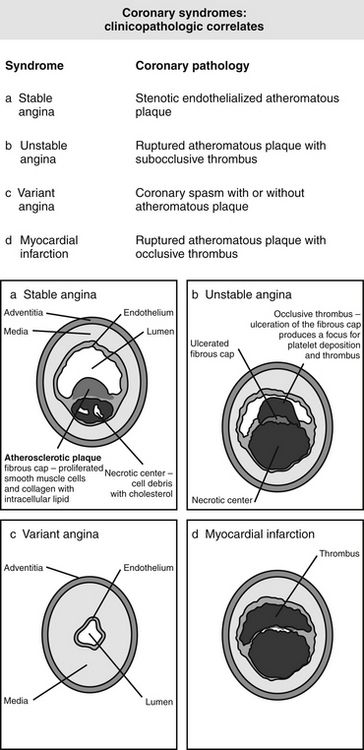
Atheromatous Lesions
The atherosclerotic process is the buildup of plaque in blood vessels. This process occurs throughout the body. The arteries most often affected are the coronary arteries (CAD), the cerebral vascular arteries (stroke), and the peripheral arteries (PVD). The first step in the process of atherosclerosis is deposition of the fatty streak. Lipid-laden foam cells derived from macrophages or smooth muscle cells accumulate on the subendothelial lining. The most important lipids in this step are the low-density lipoproteins (LDLs). Smooth muscle cells migrate into the lesion. At this step, the plaque does not affect circulation. Progression of these fatty streaks leads to the development of a collagen cap. The lesion becomes calcified, and the vessel lumen slowly becomes narrowed.
As the plaque grows, it may develop an internal hemorrhage, which then leaks to the surface. The body reacts by formation of a thrombus. Infarction occurs as the result of total occlusion of the artery by the thrombus (Figure 18-2).
Increased Myocardial Oxygen Demand
Myocardial ischemia can be brought on by increased myocardial oxygen requirements such as exercise, mental stress, or spontaneous fluctuations in heart rate and blood pressure. It also can be caused by decreased oxygen supply such as occurs with vasospasm, platelet plugging, or partial thrombosis. Oxygen supply to the myocardium depends on filling of the coronary arteries during diastole. Filling depends on coronary perfusion pressure and coronary vascular resistance. Coronary vascular resistance depends on the degree of collateralization and the patency of the coronary blood vessels. With exercise, the coronary blood flow may have to increase to as much as four to five times above resting level.
Catecholamine Release
Catecholamines are released in response to exertional and emotional stress or other activity. Catecholamines cause increased heart rate, blood velocity, and force of myocardial contraction, producing increased oxygen demand and ischemia. Increased heart rate decreases the length of diastole, which occurs when the coronary arteries perfuse the myocardium. Ischemia then stimulates further catecholamine release. If the myocardium does not receive enough oxygen, ischemia may result in pain (angina), arrhythmia, or left ventricular dysfunction (CHF). Ischemia can be either painful or pain free. Silent ischemia is as dangerous as painful ischemia.
Disease Process
Several large epidemiologic studies have identified certain habits and predisposing conditions that correlate with the development of CAD (Box 18-1). One can determine the 10-year coronary heart disease risk based on the Framingham study, as described by the National Cholesterol Education Program (NCEP) Expert Panel (see Chapter 24).
Added to the traditional risk factors is a new group of markers. C-reactive protein (CRP) and homocysteine are markers of inflammation. CRP is a highly sensitive marker for inflammation, but it lacks specificity. Data from more than 30 epidemiologic studies have shown a significant association between an elevated CRP level and the prevalence of underlying atherosclerosis, the risk of recurrent cardiovascular events among patients with established disease, and the incidence of first cardiovascular events among individuals at risk for atherosclerosis. Elevated levels may also be found in patients with metabolic syndrome, cigarette smoking, type 2 diabetes, and dyslipidemia. CRP can be decreased through the use of statins, fibrates, and cholesterol absorption inhibitors, as well as by weight loss, increased physical activity, smoking cessation, and the use of β-blockers but not aspirin, although the clinical benefit of lowering CRP is yet to be substantiated. The clinical benefit of merely altering or normalizing these surrogate markers is yet to be supported by rigorous evidence. Normalizing surrogate markers does not abolish risk.
Homocysteine produces a proinflammatory response and is associated with poor dietary folate, vitamin B6 and B12 deficiency, and renal insufficiency. Screening tests for these markers are readily available. Although early data on the relationship between elevated blood homocysteine concentrations and coronary heart disease (CHD) and stroke have been somewhat inconsistent, high homocysteine levels appear to be clearly associated with an increased risk of cardiovascular and cerebrovascular disease. However, homocysteine does not appear to be as important as other risk factors such as hypercholesterolemia, smoking, diabetes mellitus, and hypertension. Recommendations on the use of tests for homocysteine and CRP have not been established; these tests are not recommended for routine screening. They probably are best used with patients at elevated risk for CAD from other risk factors. Elevations in these test results may indicate the need for an aggressive preventative approach.
Additional risk factors include lipoprotein (a) [Lp(a)] and fibrinogen. Lp(a) possesses an atherogenic effect. Most patients with an elevated Lp(a) have diabetes or elevated LDL. Lipoprotein may be measured accurately, but a test is not commonly available. Fibrinogen is a plasma protein that plays an important role in thrombosis. Drugs known to lower fibrinogen include tamoxifen, anabolic steroids, ticlopidine, pentoxifylline, and fenofibrate. Measurement is not reliable. It is possible that these tests will be useful in patients with premature atherosclerosis or family history of premature CAD.
Collagen vascular disease is a recently identified risk factor. Patients with rheumatoid and systemic lupus erythematosus have increased risk of cardiovascular disease; this may be related to chronic inflammation or treatment of the disease with steroids and nonsteroidal antiinflammatory drugs (NSAIDs). Coronary artery calcification, as measured by electron beam computed tomography (EBCT), quantifies the amount of calcium in the coronary arteries and correlates well with angiographically defined CAD.
Other possible risk factors are now being explored. These include brain natriuretic peptide (BNP) and endothelial dysfunction, as well as infection (acute or chronic). BNP is a natriuretic hormone that was initially identified in the brain but is also present in the heart, particularly the ventricles. In heart failure, BNP is released in response to high ventricular filling pressures. The plasma concentrations of BNP in patients with asymptomatic and symptomatic left ventricular dysfunction permit their use in diagnosis. The usefulness of BNP in differentiating cardiac from noncardiac causes of dyspnea in difficult-to-assess patients remains uncertain. Levels of generalized and coronary endothelial dysfunction are important prognostic indicators of progression of coronary atherosclerosis and clinical cardiovascular events. Brachial reactivity is a noninvasive measure of endothelial dysfunction that can be obtained relatively cheaply, but its reliability and validity have not been tested. Erectile dysfunction may be related and may be a clinical marker.
Infection, both acute and chronic, may be implicated. Acute infections are associated with a transient higher incidence of CHD. Some theorize that chronic infections such as pneumonia, cytomegalovirus, and Helicobacter pylori may stimulate low-grade chronic inflammation and thus atherosclerosis. Trials with long-acting macrolides have not demonstrated benefit. BNP is released from myocardial cells in response to volume expansion and myocardial wall tension, and elevations are associated with the presence of heart failure. The Framingham Heart Study found BNP to be a predictor of cardiovascular disease (CVD) and death in subjects without heart failure. The significance of this remains to be elucidated.
Angina
Anginal ischemic myocardial pain has two major causes. By far the most common is arteriosclerotic heart disease, which was described previously. The other cause seen in primary care is coronary vasospasm with or without atherosclerotic CAD.
Definition of Disease
Myocardial ischemia occurs when myocardial oxygen demand exceeds oxygen supply. Increased demand usually occurs as the result of tachyarrhythmias, hypertension, and exercise, all of which increase cardiac workload. Decreased supply usually results from coronary artery stenosis. Angina pectoris is defined as chest pain, pressure, or discomfort caused by myocardial ischemia.
Classification
Assessment
The history is crucial to the diagnosis of CAD. Myocardial ischemia causes angina, a symptom of CAD. The sensation of angina is usually described as heavy substernal pressure or pain that may radiate to the left arm. It is brought on by exertion and is relieved by rest. The sensation may be described as tightness, squeezing, gas, indigestion, or a vague discomfort instead of as pain. The pain may occur anywhere from the lower jaw to the epigastrium. It may radiate to the right arm in addition to the left. If the patient identifies the site of pain by pointing to the area of the apical impulse with one finger, angina is unlikely. The episode may last 15 to 30 minutes, but substantial variation has been noted. Patients usually are most comfortable in a sitting position. They may feel short of breath. Occasionally, a patient may have myocardial ischemia with no other symptoms; silent ischemia will show up on ECG.
On physical examination, blood pressure may be elevated or lowered. An occasional extra sound or systolic murmur may be heard. ECG shows characteristic changes of ischemia in about 75% of patients with angina. The other 25% exhibit other abnormalities on ECG. The characteristic change is a horizontal or downsloping ST-segment depression that resolves as the angina resolves. T-wave flattening or inversion also may occur. Occasionally, ST-segment elevation occurs. Examination of the patient between episodes of angina may reveal normal findings, including those obtained via ECG.
Basic diagnostic studies include serum lipid levels, CBC, electrolytes, ECG, and exercise testing. Myocardial perfusion scintigraphy uses radionuclide uptake to identify areas of hypoperfusion. An echocardiogram is useful for assessing left ventricular function. Coronary angiography is the definitive diagnostic procedure for coronary disease. Newer imaging techniques include CT scanning and MRI, but their usefulness remains to be determined.
Mechanism of Action
Currently, three major classes of antianginal drugs are used in the medical management of angina pectoris: nitrates (short- and long-acting), β-blockers, and calcium channel blockers. (β-Blockers and calcium channel blockers are discussed in later chapters.)
A fourth option, ranolazine, is a new drug that should be used in conjunction with other agents, and its mechanism of action is unknown. Evidence suggests that ranolazine is an inhibitor of the late sodium current and that its use results in reduction of the intracellular sodium and calcium overload in ischemic cardiac myocytes. This agent does not demonstrate negative chronotropic or inotropic effects, and minimal effects on heart rate and blood pressure have been noted during clinical trials. Most commonly, a combination of these antianginal agents is used for management. In combination with β-blockers or calcium channel blockers, nitrates and ranolazine produce greater antianginal and antiischemic effects.
Nitrates relax vascular smooth muscle via stimulation of intracellular cyclic guanosine monophosphate production. The major effect of nitrates is to reduce myocardial oxygen demand, primarily by decreasing preload and to a lesser extent by decreasing afterload. Nitrates cause major dilation of the venous bed. Vasodilation results in venous pooling of blood, thereby decreasing venous return. Decreased venous return reduces ventricular end-diastolic volume. This reduction in preload results in reduced filling pressure (i.e., decreased pressure of blood against the wall of the heart). Reduced wall tension decreases myocardial oxygen demand.
A relatively minor effect of nitrates is the reduction in afterload achieved by arterial relaxation. Reduced afterload decreases myocardial work, which reduces oxygen consumption. Another relatively minor effect of nitrates is that they improve myocardial oxygen supply by optimizing blood delivery via dilation of coronary arteries. This may be an important mechanism in the prevention and treatment of patients with coronary vasospasm. Nitrates also increase the use of coronary collaterals so that perfusion of the inner layers of the myocardium is improved.
Treatment Principles
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree