12 Congestive heart failure
Pathophysiology
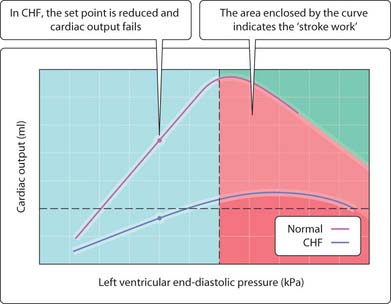
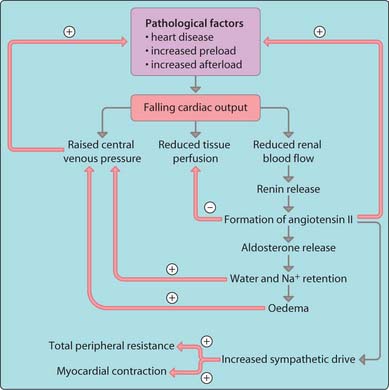
Congestive heart failure (CHF) is a failure of the ventricles to maintain adequate output and has many causes, including myocardial infarction, hypertension and cardiomyopathies. In backward failure, blood is not efficiently pumped out of the ventricles. This leads to an increase in ventricular filling pressure, giving rise to venous congestion and systemic oedema (Fig. 3.12.1). In forward failure, the fall in cardiac ouput means that less blood reaches the kidneys and this stimulates Na+ and water retention, which exacerbates further fluid retention and systemic oedema (see Fig. 1.13). Fluid retention in the lung owing to increased pressure in the veins in the lung results in shortness of breath and pulmonary oedema. Weakness and fatigue are symptoms associated with lower blood supply to other organs. The body attempts to compensate by stimulating extrahumoral (sympathetic) reflexes to restore cardiac output by increasing cardiac contractility and vasoconstriction (Fig. 3.12.2). The heart is forced to pump against an increasing resistance (afterload), which depresses cardiac output. The fall in blood supply to the kidney again increases venous return (preload) and tissue oedema. This increase in preload contributes to the incomplete emptying of the ventricles and a rise in end-diastolic pressure. This activates an intrinsic cardiac compensatory mechanism and as ventricular hypertrophy develops this may reduce tension generated by the muscle (Frank–Starling curve) and the heart eventually fails.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree