Table 4-1. Nonsterile Maximum Beyond-Use Datesa
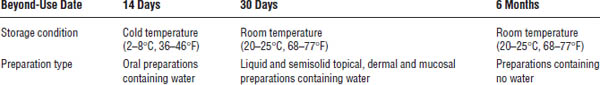
a. The BUD cannot be greater than the expiration date of any component used to compound the preparation. Inclusion of an antimicrobial agent should be considered, if appropriate. Dispense in a container that reduces exposure to light and moisture.
Quality Control Requirements
■ Accurate calculations
■ Accurate weights
■ Accurate measurements
■ Proper processing techniques
■ Proper packaging
■ Proper records
■ Proper labeling, including BUDs
■ Proper documentation of quality assurance, quality control, and preparation testing
Beyond-Use Dates
■ Pharmacists assign BUDs to compounded preparations to guide patients in the proper use and storage of the preparation.
■ The goal is to provide a BUD that will allow the patient enough time to fully use the amount of preparation dispensed but not enough time to allow the preparation to degrade, lose potency, or be stored for future use.
■ If the pharmacist does not have a reference on the stability of the specific dosage form compounded or sufficient experience with it, the section “General Guidelines for Assigning Beyond-Use Dates” in USP Chapter <795> is followed. Table 4-1 summarizes beyond-use dating.
4-8. Compounded Dosage Forms
Solutions
■ Definition: Solutions are chemically and physically homogenous mixtures of two or more substances.
■ Types: Examples include syrups, elixirs, aromatic waters, tinctures, and spirits. Solutions can be aqueous or nonaqueous.
■ Properties: Examples include hypertonic, isotonic, hypotonic, osmolar, and osmolal.
■ Stability: Examples of how the stability of solutions can be enhanced include adjusting pH, adding a preservative, and adding an antioxidant.
■ Rate of dissolution: Examples of how the rate of dissolution is enhanced include stirring, heating, and reducing particle size.
■ Beyond-use dates: Aqueous solutions have shorter BUDs than do nonaqueous solutions.
■ Testing: Organoleptic, pH, and other tests are performed.
An example of an isotonic aqueous solution follows:
Ephedrine sulfate | 1% |
Sodium chloride | qs |
Purified water, qs ad | 30 mL |
M.ft. isotonic nasal solution |
|
Steps in compounding are as follows:
- Calculate the required quantity of each component. The NaCl equivalent of ephedrine sulfate is 0.2.
- Accurately weigh or measure each component.
- Dissolve the solid components in about 25 mL of purified water.
- Add sufficient purified water to measure 30 mL.
- The BUD is a maximum of 30 days according to USP Chapter <795> guidelines.
An example of a nonaqueous solution follows:
Urea | 10 g |
Salicylic acid | 5 g |
Coal tar solution | 5 mL |
Propylene glycol, qs ad | 100 mL |
Steps in compounding are as follows:
- Accurately weigh or measure each component.
- Dissolve the urea and salicylic acid in about 75 mL of propylene glycol.
- Add the coal tar solution, and mix well.
- Add sufficient propylene glycol to measure 100 mL.
- The BUD is a maximum of 6 months according to USP Chapter <795> guidelines.
Note: Use of a mechanical stirrer can reduce the time needed to dissolve the urea and salicylic acid.
Suspensions
■ Definition: A suspension is a two-phased system containing a finely divided solid in a vehicle.
■ Requirement: The drug is uniformly dispersed throughout the vehicle.
■ Concentration: Suspending agents are typically used in a concentration of 0.5–6%.
■ Viscosity: The vehicle has enough viscosity to keep drug particles suspended separately.
■ Insolubility: The active pharmaceutical ingredient is insoluble in the vehicle.
■ Tip: Wet the insoluble powder with a vehicle-miscible liquid.
■ Advantage: A suspension allows the preparation of a liquid form of an insoluble drug.
■ Stability: Stability is enhanced by adding a preservative.
■ Testing: Organoleptic, pH, and other tests are performed.
Categories of suspending agents are as follows:
■ Natural hydrocolloids: Acacia, alginic acid, gelatin, guar gum, sodium alginate, tragacanth, and xanthan gum
■ Semisynthetic hydrocolloids: Ethylcellulose, methylcellulose, and sodium carboxymethylcellulose
■ Synthetic hydrocolloids: Carbomers (Carbopol), poloxamers (Pluronic), polyvinyl alcohol, and polyvinylpyrrolidone
■ Clays: Bentonite and magnesium aluminum silicate (Veegum)
An example of an oral suspension follows:
Progesterone, micronized | 1.2 g |
Glycerin | 3 mL |
Methylcellulose 1% solution | 30 mL |
Flavored syrup, qs ad | 60 mL |
Steps in compounding are as follows:
- Accurately weigh or measure each component.
- In a glass mortar, wet the progesterone with the glycerin to form a thick paste.
- Slowly add the methylcellulose solution while triturating.
- When mixed thoroughly, pour into a graduate.
- Add small amounts of syrup to the mortar, mix, and add to graduate until the desired volume is reached.
- The BUD is a maximum of 14 days refrigerated according to USP Chapter <795> guidelines.
Note: The methylcellulose 1% solution should be prepared before compounding the suspension.
The methylcellulose 1% solution can be prepared as follows:
Methylcellulose 1,500 CPS | 1% |
Sodium benzoate | 200 mg |
Purified water, qs ad | 100 mL |
- Calculate the amount of each component required.
- Accurately weigh or measure each component.
- Add methylcellulose to 50 mL boiling purified water, and mix well.
- Add sodium benzoate, and mix.
- Add cold purified water to bring to final volume. Stir until thick and uniform.
Emulsions
■ Definition: An emulsion is a two-phase system of two immiscible liquids, one of which is dispersed throughout the other as small droplets.
■ Components: An emulsion has an external, continuous phase or dispersion medium; an internal, discontinuous or dispersed phase; and an emulsifying agent.
■ Type: Types are oil in water (o/w) and water in oil (w/o), depending on which is the internal or external phase.
■ Emulsifying agents: Emulsifying agents can be natural gums (acacia, agar, chondrus, pectin, and tragacanth) or hydrophilic or lipophilic agents (the esters of sorbitan).
■ Lipophilic agents: Trade names for lipophilic agents include Arlacel and Span.
■ Hydrophilic agents: Trade names for hydrophilic agents include Myrj and Tween.
■ Hydrophilic–lipophilic balance: A lower hydrophilic–lipophilic balance (HLB) value favors a w/o emulsion; a higher HLB value favors an o/w emulsion. Agents with an HLB value of 1–10 are considered to be lipophilic, while agents with an HLB value of > 10 are considered to be hydrophilic. Emulsions with an HLB value of 3–8 are water in oil, while those with an HLB value of > 8 to 16 are oil in water.
■ Other agents: Other agents include bentonite, cholesterol, gelatin, lecithin, methylcellulose, soaps of fatty acids, sodium docusate, sodium lauryl sulfate, and triethanolamine.
■ Equipment: Equipment includes mortars and pestles, homogenizers, colloid mills, mechanical mixers, agitators, and ultrasonic vibrators.
■ Solids: Solid components should be dissolved before they are incorporated into the emulsion, or if a sizable quantity is added, a levigating or wetting agent may be needed.
■ Flavors or fragrances: Flavors or fragrances should generally be incorporated into the external phase.
■ Preservatives: Preservatives should be added in the aqueous phase but may also be added in the oily phase, if necessary.
■ Stability: Emulsions can either cream or crack.
■ Continental method: The continental or dry gum method of preparing an emulsion nucleus involves using the oil:water:dry gum emulsifier in a 4:2:1 ratio.
■ Advantages: An emulsion can be used to mask taste, improve palatability, increase absorption, and enhance bioavailability.
■ Testing: Organoleptic testing is performed.
An example of preparing an emulsion by the continental, dry gum (4:2:1) method follows:
Cod liver oil | 50 mL |
Acacia | 12.5 g |
Syrup | 10 mL |
Methyl salicylate | 0.4 mL |
Purified water, qs ad | 100 mL |
Steps in compounding are as follows:
- Accurately weigh or measure each component.
- Place the cod liver oil in a dry porcelain mortar.
- Sprinkle the acacia on the oil, and give it a very quick mix with the pestle.
- Add 25 mL of purified water, and immediately triturate rapidly to form the thick, white, homogenous emulsion nucleus.
- Add the methyl salicylate, and mix thoroughly.
- Add the syrup, and mix thoroughly.
- Add sufficient purified water to measure 100 mL.
- The BUD is a maximum of 14 days refrigerated according to USP Chapter <795> guidelines.
Capsules
■ Definition: This dosage form incorporates components into a shell called a capsule.
■ Procedure: Determine capsule size to fit total powder weight, triturate powders to reduce particle size, mix powders by geometric dilution, incorporate the diluent by geometric dilution if required, and clean the outside of the filled capsules.
■ Advantages: Capsules mask unpleasant taste; allow the mixture of components that could not be mixed in other vehicles; can alter the release rate of active pharmaceutical ingredients by adding hydroxypropyl methylcellulose (HPMC); allow incorporation of several components into one dosage form; provide an accurate dosage size for liquids, semisolids, and powders; and provide a dosage form that is easier to swallow and more acceptable to the patient.
■ Methods of filling: Hand punch from powder on an ointment slab or use a capsule-filling machine.
■ Sizing: Capsules available, listed from largest to smallest, include 000, 00, 0, 1, 2, 3, 4, and 5. Determining the size of capsule to use for a particular dosage involves assessing the density or fluffiness of the powder, comparing it to known weights of various reference powders with published capsule-size capacities, and then filling and weighing the capsule. If the requested dosage does not fill a specific size of capsule, a filler should be added.
■ Testing: Organoleptic, weight percent error, weight variance, and other tests are performed.
An example of an altered-release capsule follows:
Progesterone, micronized | 25 mg |
HPMC | 50% |
Lactose, qs ad per capsule size |
|
M.ft. capsules | 15 doses |
Steps in compounding are as follows:
- Select the appropriate capsule size, and calculate the required quantity of each component. The quantity of lactose needed depends on the capsule size required.
- Accurately weigh each component.
- If necessary, reduce particle size, and mix thoroughly by geometric dilution.
- Fill capsules.
- Weigh capsules.
- The BUD is a maximum of 6 months according to USP Chapter <795> guidelines.
Tablet Triturates
■ Definition: A tablet triturate is a small tablet that is made in a mold and intended for sublingual administration. The molded tablet usually weighs about 60 to 200 mg.
■ Advantages: A tablet triturate rapidly dissolves under the tongue, is rapidly absorbed, avoids the first pass through the liver, and provides a rapid therapeutic response.
■ Components: Tablet triturates consist of an active pharmaceutical ingredient and a base, which may consist of lactose, sucrose, dextrose, and mannitol.
■ Formulation: Molds that make 50 tablets are generally available in approximate 60, 100, and 200 mg tablet sizes. Formulations must be calculated to fit the size of mold that will be used. If this capacity is not known, the capacity must be determined by filling the mold holes with the tablet triturate base and weighing the resulting tablets. On the basis of the size of the mold holes, mix the active pharmaceutical ingredient with the base, which often consists of four parts lactose and one part sucrose. Thoroughly triturate powders, mix by geometric dilution, and then moisten with a wetting solution containing four parts 95% ethyl alcohol and one part purified water until the powder mixture is adhesive. Press into mold uniformly.
■ Testing: Organoleptic, weight percent error, weight variance, and other tests are performed.
■ Tip: Tablets may be flavored by adding a flavor to the wetting solution. Color may be added by adding a small amount of powdered color to the powder mixture.
An example of a tablet triturate follows:
Testosterone | 3 mg |
Base, qs ad per mold size |
|
M.ft. tabs | 50 doses |
Steps in compounding are as follows:
- The base may consist of a 1:4 mixture of sucrose and lactose.
- The wetting solution may consist of a 1:4 mixture of purified water and 95% ethyl alcohol.
- Select the size of tablet triturate mold to be used. The quantity of base needed depends on the size of the mold selected.
- Calibrate the mold for the base being used. Based on the weight of tablets it makes, calculate the required quantity of each component.
- Accurately weigh or measure each component.
- Reduce particle size, and mix components by geometric dilution.
- In a glass mortar, gradually moisten the powder mixture until it becomes adhesive. Drop the wetting solution onto the powder a few drops at a time, and triturate after each addition until the powder becomes moist and adhesive.
- Press moist powder evenly into all holes in the tablet triturate mold plate.
- Place the mold plate on the base plate, and press down until the tablets rest on top of the pegs.
- Let tablets air dry.
- Very gently remove dried tablets from pegs.
- The BUD is a maximum of 30 days according to USP Chapter <795> guidelines.
Troches, Lozenges, and Lollipops
■ Definition: Troches, lozenges, and lollipops or suckers are solid dosage forms intended to be slowly dissolved in the mouth for local or systemic effects.
■ Formulation: Troches, lozenges, and lollipops are composed of an active pharmaceutical ingredient and a base that may consist of (1) sugar and other carbohydrates that produce a hard preparation, (2) polyethylene glycols (PEGs) and other components that produce a softer preparation, or (3) a glycerin–gelatin combination that produces a chewable preparation.
• Formulations made in a mold complete with sticks are called lollipops or suckers.
• Formulations must be calculated to fit the size of mold that will be used. If this capacity is not known, the capacity must be determined by filling the mold cavities with the base and weighing the resulting troches, lozenges, or lollipops.
• Flavors and colors are added just before the molds are filled.
■ Advantages: Troches, lozenges, and lollipops are easy to administer, are convenient for patients who cannot swallow oral dosage forms, maintain a constant level of drug in the oral cavity and throat, and can have a pleasant taste.
■ Testing: Organoleptic, weight percent error, weight variance, and other tests are performed.
An example of a troche follows:
Gelatin | 2.62 g |
Glycerin | 9.36 mL |
Purified water | 1.3 mL |
Acacia | 0.28 g |
Bentonite | 0.28 g |
Benzocaine | 0.17 g |
Citric acid | 0.3 g |
Stevia | 0.15 g |
qs | |
Color | qs |
M. ft. troches | 12 doses |
Mold holds | 1.4 g. |
Note: With a specific gravity of 1.25, the 9.36 mL of glycerin weighs 11.7 g. The formula is written for 12 troches. Dividing the final formula weight by 12 determines the weight of a single troche.
Steps in compounding are as follows:
- Calibrate the mold for the base composed of gelatin, glycerin, and purified water to verify a troche weight of 1.4 g per cavity. If needed, based on the actual troche weight, recalculate the required quantity of each component.
- Accurately weigh or measure each component.
- Triturate and thoroughly mix, using geometric dilution, the acacia, bentonite, benzocaine, citric acid, and stevia powders.
- Heat the glycerin on a boiling water bath until warm.
- Add the water, and heat for a few minutes.
- While stirring, very slowly add the gelatin. The gelatin must be lump free; the mixture must be homogeneous.
- Add the powders to the warm liquid and mix thoroughly.
- Add flavor and color. Mix, pour into the mold, and let cool.
- The BUD is a maximum of 30 days according to USP Chapter <795> guidelines.
Transdermal Gels
■ Definition: Transdermal gels move medications through the skin in quantities sufficient to produce a therapeutic effect.
■ Components: Transdermal gels have the following components:
• Active pharmaceutical ingredients and other components
• Gelling agents: for example, the carbomers (e.g., Carbopol 934P), methylcellulose, the poloxamers (e.g., Pluronic F-127), and sodium carboxymethylcellulose
• Wetting or levigating agents: for example, propylene glycol and glycerin
• Penetration-enhancing agents: for example, alcohol, lecithin, dimethyl sulfoxide, isopropyl myristate, isopropyl palmitate, propylene glycol, and PEG
• Suspending or dispersing agents: for example, bentonite and silica gel
■ Testing: Organoleptic testing is performed.
■ Advantages: Transdermal gels are convenient, effective, and acceptable to patients. The gels avoid some problems that other dosage forms have, such as gastrointestinal irritation from oral dosages, pain from injections, and the undesirability of suppositories.
■ Formulation: Use proper techniques for creating the gel, adjust the pH for carbomer gels, respect the temperature for poloxamer gels, use small amounts of nonaqueous solvents, and, if possible, keep electrolyte components to a minimum.
■ Tip: Do not use transdermal gels for the systemic use of antibiotics, and do not try to get large molecules such as proteins through the skin by transdermal gels.
An example of a transdermal gel using carbomer as the base follows:
Ketoprofen | 5% |
Carbomer 934P | 2% |
Alcohol 95% | qs |
Triethanolamine | 2 mL |
Purified water, qs ad | 30 mL |
Steps in compounding are as follows:
- Calculate the required quantity of each component.
- Accurately weigh or measure each component.
- Triturate the carbomer 934P in a glass mortar.
- While triturating, gradually add about 18 mL of purified water.
- Be sure that the carbomer and water are thoroughly mixed and the mixture is homogenous.
- Dissolve the ketoprofen in about 10 mL 95% ethyl alcohol.
- While triturating, add the ketoprofen solution to the carbomer–water mixture and mix thoroughly.
- If necessary, add purified water to make about 28 mL, and pour into an ointment jar.
- Add triethanolamine, and stir quickly with a stirring rod until the gel is thoroughly formed.
- The BUD is a maximum of 30 days according to USP Chapter <795> guidelines.
Note: A trade name for carbomer 934P is Carbopol 934P, and for triethanolamine, it is Trolamine.
An example of a transdermal gel using pluronic lecithin organogel (PLO) as the base follows:
Ketoprofen | 5% |
Propylene glycol |



