COMMUNITY PHARMACY
Daniel Krinsky, MS, RPh, and Stacey Schneider, PharmD
CASE
L.B. is a pharmacy student starting his first day in a community pharmacy APPE rotation. His preceptor has told him that he will be spending the morning in the pharmacy doing routine tasks the pharmacist performs to dispense prescriptions. His afternoon will be spent doing a medication therapy management (MTM) visit with a previously scheduled patient, along with other patient-focused activities. As part of his morning routine, L.B. will be required to do a return-to-stock audit on previously filled prescriptions, answer and make physician phone calls, counsel patients on new prescriptions, address drug utilization review (DUR)/clinical issues during the filling process, and perform over-the-counter (OTC) consults. All of these tasks will require L.B. to review patient pharmacy records and obtain information as needed from other practitioners. L.B. has never worked in a community pharmacy and is nervous about his ability to complete these tasks.
WHY IT’S ESSENTIAL
Welcome to the world of community pharmacy—a continually changing arena in which to practice pharmacy. Finding ways to constantly balance the changing demands of the healthcare system and those of the retail market makes the community pharmacist position one of the most challenging and rewarding positions in the profession. The goal of the community pharmacy experiential rotation is to provide you with an opportunity to practice contemporary pharmacy in a community setting. Because a majority of graduates from pharmacy schools will practice in a community pharmacy setting, it is critical for you to obtain as much experience as possible in a structured learning environment prior to graduation to build skills, knowledge, and confidence.
Although we have numerous “controlled” simulation activities built into the on-campus curriculum, nothing compares to real-world experiences. Students typically learn the basic elements of how to practice and manage patients in the community pharmacy setting through these campus activities, their internship, and their IPPE rotations, but the APPE rotation brings everything together in 1 to 2 months and places the student on the front line. You see how a pharmacy staff manages everything from handling the prescription verification process and managing difficult patients to developing and delivering medication therapy–management services.
“What I experienced during my rotation was much more dynamic than what I do during my internship. I now see how I can apply what I’ve learned in school and what’s possible when I become a pharmacist.”—Student
“Don’t settle for the status quo. If you’re not being challenged by your preceptor, ask about ways to get more involved.”—Preceptor
ARRIVING PREPARED
The following is a checklist of recommended actions prior to day 1 of your APPE community pharmacy rotation:
- Contact the preceptor ahead of time and ask for information on required readings, disease states to review, and logistical information (parking, location, etc.).
- Obtain a general understanding of the types of personnel working and the basic layout of the pharmacy. These issues are discussed in more detail in the next section.
- Formulate your own personal objectives for the rotation and determine what goals you would like to accomplish; however, ensure they are consistent with the site’s objectives.
- Dress professionally; white coat and appropriate identification are mandatory at sites.
- Check with your preceptor to see if pocket reference guides or their electronic counterparts are allowed.
- Review pertinent topics prior to your first day, including drug therapy problems, patient interviewing, counseling skills, drug literature review, and statistical interpretation.
- Be familiar with the most recent treatment guidelines. These include, but are not limited to, the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7); the Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III, or ATP III); Standards of Medical Care in Diabetes from the American Diabetes Association (ADA); and Guidelines for Diagnosis and Management of Asthma from the National Heart Lung and Blood Institute (NHLBI).
- Become familiar with MTM services that might be offered. Additional detail is discussed in the MTM Consultation section later in this chapter.
- Understand the importance of the different types of communication that may be necessary.
- Be prepared for OTC consultations.
“Preceptors appreciate when students approach the rotation with a genuine interest in learning and participating, regardless of preconceived ideas, what they’ve heard, or where they feel they’ll end up practicing after graduation.”—Preceptor
A TYPICAL DAY
A typical day during your community pharmacy APPE rotation will involve dispensing, patient-focused activities, and work on projects.
Dispensing activities in the community pharmacy might encompass the following:
- Assisting with processing prescriptions
- Addressing DUR and clinical messages
- Patient counseling
- OTC consults
- Phone calls to physician offices to clarify prescriptions or obtain answers to questions
- Assisting with various audits
- Immunizations (where allowed by law)
Patient-focused activities in the community pharmacy might encompass the following:
- Comprehensive medication reviews (CMRs) with patients as part of an MTM visit—either in the pharmacy or through a home visit
- Wellness screening programs (inside and outside the pharmacy)
- Community outreach events, such as presentations to nursing home residents or community organizations
- Immunization clinics
- Physician office visits to promote pharmacy-specific products and services
Projects may include the following:
- Preparing for and delivering a journal club article
- Preparing for and delivering a case presentation
- Writing a newsletter article for healthcare professionals
- Developing a community-focused presentation
- Preparation for other patient care–focused activities
DISPENSING PROCESS
You will be expected to demonstrate effective pharmacy practice skills in order to assist with the dispensing process. This description is based on the authors’ experiences and discussions with other community pharmacists. Almost all community pharmacies employ the following types of individuals:
- Pharmacists: staff and management-level professionals could be in your pharmacy.
- Pharmacy technicians: some may be certified through the national Pharmacy Technician Certification Board (PTCB) and others via state requirements; some will not be certified at all. These individuals are trained to assist the pharmacist in many activities related to prescription processing and customer service.
- Clerks: entry-level staff that are not involved in any activities related to the processing of a prescription. These individuals are usually responsible for running the cash register or similar activities.
Each of these individuals plays an integral role in every activity that takes place within the pharmacy. It is imperative that tasks be matched as closely as possible to the various individuals in the pharmacy and that everyone works together, as the volume of work can be quite challenging to manage, even with optimal teamwork and workflow. Your preceptor should find ways to introduce you to the staff and integrate you into the workflow in the appropriate areas at the appropriate time.
L.B. would like to familiarize himself with prescription processing on his first day. Which of the pharmacy personnel would be the most appropriate to shadow?
Prescription Processing
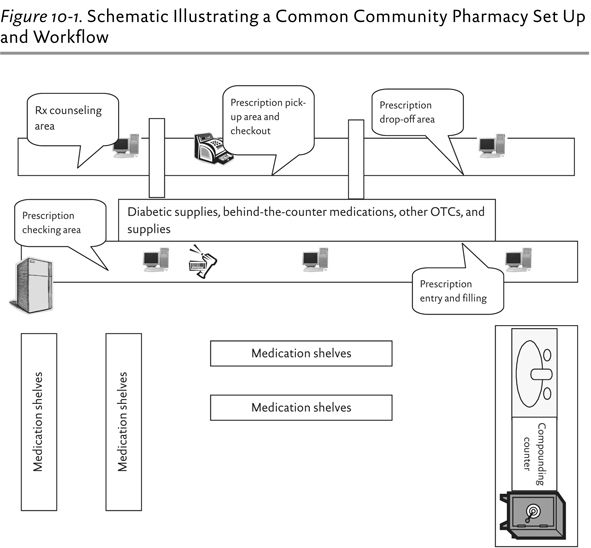
Most pharmacies are designed to facilitate optimal workflow and maximize work output with minimal movement throughout the physical structure. Figure 10-1 shows an example of a pharmacy layout, with all the critical sections needed for pharmacy activities, including the prescription drop off, a terminal for order entry, workspace for prescription assembly, a pharmacist’s verification terminal, and an area for patients to pick up prescriptions.
Prescription processing begins at a computer terminal with a software program for prescription entry and processing, label and patient advisory leaflet printing, and maintaining patient profiles and insurance information. The primary prescription entry station, often staffed by a student or technician (although sometimes staffed by a pharmacist), will be located close to the drop-off area. Prescriptions come into the pharmacy in various ways, such as by fax, phone call, voicemail message, e-prescribing, or patient drop-off. For patients who present prescriptions in person, you should also obtain information about allergies, insurance coverage, and contact information. Oftentimes, much of this information will be obtained from a prescriber’s office when prescriptions are phoned into the pharmacy. As a student, your ability to participate in taking phoned-in prescriptions and retrieving prescriptions from the voicemail system is state-specific. If you are involved with phoned-in prescriptions, be sure to follow the “repeat back” policy to verify every piece of information when speaking with a prescriber or prescriber’s agent. When listening to recorded messages, review the message at least twice to verify all information. Once all of the necessary information has been obtained, the prescription is ready to be entered into the pharmacy computer system by a pharmacist, student, or technician.
Close by, the prescription assembly area is where all the paperwork and prescription information is put together. This is where the medication is counted, the bottle is labeled, and all components are prepared for the pharmacist to check. A great deal of paperwork will have been generated by this time, including, where necessary the following:
- Hard-copy prescription
- Label for the bottle, including all auxiliary labels
- Sticker/tag that is adhered to the back of the hard-copy prescription that reflects all information entered in the patient profile and is part of the permanent pharmacy record
- Patient information leaflet
- Any clinical messages that still need to be addressed by a pharmacist (or student with pharmacist supervision)
- Any documents describing insurance/copay information the patient will want to review
- Supplemental marketing pieces that complement the other drug information
- Receipt that indicates copay or other prescription price
At this point, the prescription can be filled. Once the correct drug is selected from the shelf, it is counted and placed in a vial with the correct cap (child-proof unless a snap cap is requested by the patient) and the label is applied. In busy pharmacies, there may be enough technicians involved so that the filling technician double-checks the work of the entry technician. This helps to prevent errors or problems from being passed forward. The more trained eyes that can review a prescription, the less chance errors will be made or key information missed. Oftentimes, students will be placed in the role of secondary checker prior to the pharmacist’s final verification.
QUICK TIP
To help ensure that the proper medication is chosen from the shelves, the National Drug Code (NDC) on the prescription label should be matched to the NDC on the stock bottle.
Once everything is assembled, the items (documents, stock bottle, labeled prescription vial, and anything else) are given to a pharmacist for the final check. The final verification encompasses many steps to ensure the right drug gets to the right patient at the right dose and schedule to ensure optimal response. During this process, there are no shortcuts. Pharmacists are the last people in the healthcare system to assess the appropriateness of a prescription before it is dispensed to a patient. We must remain focused and use our training, skills, knowledge, and whatever technology is available to verify that everything about the prescription is perfect. As a student on your community pharmacy APPE rotation, you should ensure that you pay close attention to how your preceptor manages this complex process so that you will be well prepared to complete the tasks yourself once you become a pharmacist.
Managing Drug Utilization Review Messages
One of the first things to address during prescription verification is any DUR messages generated during the entry process. All pharmacy dispensing software systems include an application that screens for numerous clinical issues. This screening process may also be completed by software third-party payers use when claims are filed. The goal of these software programs is to provide pharmacies with information to support the safe dispensing of medications. Resolution of some or all of these problems could be performed by pharmacy students, depending on the student’s training and the preceptor’s comfort level with student involvement. Typically, you will be involved in addressing the more clinical (versus administrative) issues. Some of the common types of messages are included in Figure 10-2.
Figure 10-2. Examples of DUR Messages
- Allergy warnings
- Drug interaction alerts
- Adherence issues (such as refill too soon, refill too late)
- Therapy duplications
- Inability to screen alert (if the new drug is not recognized by the software program, a message is generated stating the screening process did not take place and a manual check is needed)
- Age warnings—often for pediatric and geriatric individuals
- Dosing frequency alerts—the dose prescribed is higher or lower, or the prescription directions called for more doses per day than what is typically prescribed
Source: Courtesy of the Indian Health Service and the U.S. Public Health Service.
There are many ways to manage these messages. If a pharmacist is entering prescriptions, they can be addressed immediately. If technicians are entering prescriptions, the best option is to generate a printed copy of the message and allow the checking pharmacist to manage the issue. Some messages are easily addressed (verifying a dose), although many require additional effort, which normally includes a phone call to the prescriber, conversation with the patient, research using a point-of-care reference database (such as Lexi-Comp Online™), PubMed database search, phone call to a manufacturer, or any combination of these. The ultimate goal is to resolve the issue so the prescribed drug can be dispensed, replace the prescribed drug with a safer option, or seek additional follow-up with a healthcare provider before the medication is dispensed. Regardless of the outcome, it is imperative that the pharmacist (or student) documents all actions either on the prescription and/or the patient’s computerized profile. Remember, if it is not documented, it never happened.
QUICK TIP
Getting students involved in addressing DUR messages is an excellent learning exercise. We do this frequently with our APPE students and include a practice exercise with previously generated DUR messages as an introductory activity during the first week of the rotation.
L.B. has addressed a drug-interaction DUR message by calling the prescribing physician and changing a patient’s medication. Now that the potential interaction has been addressed, how should L.B. document his intervention?
Patient Counseling
Another important aspect of the dispensing process is patient counseling. There are many ways pharmacists address this issue. Some have a staff member make the offer to counsel patients, others offer counseling to certain patients directly, and some counsel every patient regardless of whether their prescriptions are new or refills. The number of pharmacists providing medication counseling has doubled over the past 30 years, but as a profession, we are still coming up short. Not only can the counseling session be used to review a new prescription, but a quick review of the patient’s profile may also uncover additional issues to discuss, such as adherence to chronic medications, response to therapy, or home monitoring.
One of the main barriers to optimizing patient outcomes with drug therapy is adherence. Numerous studies have shown that pharmacists can play a critical role in helping to improve adherence, and one way to do this is through patient counseling. Our experience has shown that counseling at the first fill of a new prescription addresses many issues the patient had not considered nor had been discussed by anyone at the physician’s office. Counseling also helps establish the patient–pharmacist relationship and lets the patient know we care about him or her as a person, not just a customer.
One common approach to patient counseling is the “Three Prime Questions.”1 Figure 10-3 lists the three prime questions to ask when patients are receiving a new drug, along with some additional issues or questions that often arise. A number of other important factors must be considered when providing effective patient counseling, such as those listed in Figure 10-4. It is important to remember to focus on the positive attributes of the medication more than the negative. If all you do is mention side effects, the patient is not likely to want to take the drug.
Figure 10-3. Three Prime Questions Asked During a Counseling Session for a New Medication
“WHAT DID YOUR DOCTOR TELL YOU (INSERT MEDICATION NAME HERE) WAS BEING USED TO TREAT?”
Depending on the patient’s response, you may have to describe this if the use is obvious (such as an Epi-Pen®) or you may need to ask the patient more questions to better determine his or her condition for a medication with multiple uses (such as lisinopril, which has multiple indications).
“HOW DID YOUR DOCTOR TELL YOU TO TAKE (INSERT MEDICATION NAME HERE)?”
Depending on response, you may need to provide additional details, such as
- Number of times per day
- Time of day
- Amount to use per dose (eye drops, creams, etc.)
- Administration in relation to meals
- Administration in relation to other medications
- How long to use (i.e., cream for 7 days, antibiotic until gone, etc.)
- What to do about a missed dose
- Storage
“WHAT TYPE OF RESPONSE DID YOUR DOCTOR TELL YOU TO EXPECT FROM (INSERT MEDICATION NAME HERE)?”
Depending on response, you may need to provide additional details, such as
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree