Common Skin Disorders
LEARNING OBJECTIVES
• INTRODUCTION
There are little data on the prevalence of dermatological disorders in various populations. Estimates and extrapolation of survey results reveal that anywhere from 12% to 31% of visits to physicians involve dermatological problems, depending on location, age, ethnicity, and type of medical provider. Pharmacists are routinely asked for assistance with diagnosis and treatment of many common skin conditions. Therefore, it is important for pharmacists to recognize common skin disorders, so they can make appropriate recommendations about self-care and referral.
• GLOSSARY
• ECZEMATOUS DISORDERS
Eczema is a general term to describe any lesion that is red, and has unclear margins and dry flaky skin. Severe cases can present with widespread lesions including cracks in the skin (fissures), weeping, and excoriation. Chronic forms of eczematous conditions become lichenified (thick, wrinkled skin) with multiple lesions.
Atopic Dermatitis (Atopic Eczema)
Atopic dermatitis is one of the most common skin conditions. It has several common characteristics that make the diagnosis relatively simple in most cases. First, it is associated with other allergic disorders. Most patients have a personal or family history of allergic rhinitis, asthma, or atopic dermatitis (aka atopic disease). Fifty percent of patients have allergic rhinitis, 60% have asthma, and 75% to 80% have a positive family history for one of the three disorders. In roughly 80% of patients, the atopic dermatitis is primarily IgE mediated and their complete blood count will reveal an eosinophilia. The second characteristic is intense itching, which many times precedes the appearance of the eczematous lesions. It is known as the “itch that rashes.” The intense itching causes patients to scratch their lesions, leading to an increased incidence of bacterial skin infections. The third characteristic is a common pattern of distribution, which varies by age. Lesions are symmetrical and in infants and toddlers the cheeks and face are the most common site. Many of the cute red-cheeked babies actually have atopic dermatitis (Figure 17.1). In children and many adults, the lesions are located in the fossae, cubital (inside of elbow), and popliteal (back of the knee) (Figure 17.2). Mild cases appear as dry, flaky, and pink skin. In patients with dark complexions, it may appear as lighter patches of skin that itch. Papules are a manifestation of moderate disease. Fortunately, most cases are mild and are amenable to successful treatment with nonprescription emollients and/or topical corticosteroids ointments.
FIGURE 17.1 An infant with atopic dermatitis on the face that has become superinfected. SOURCE: Reproduced from Usatine RP. A baby with pink cheeks. West J Med. 2000;172(4):226. With permission from BMJ Publishing Group Ltd.


FIGURE 17.2 A 20-year-old young woman with severe chronic atopic dermatitis showing lichenification and hyperpigmentation in the popliteal fossa. (Used with permission of Richard P. Usatine, MD. From Usatine RP, Smith MA, Mayeux EJ, Jr, Chumley H. The Color Atlas of Family Medicine. 2nd ed. McGraw-Hill, Inc; 2013.)
Irritant Contact Dermatitis
Irritant contact dermatitis is an accurate description of the raw, red, dry skin caused by prolonged contact with irritating/drying substances such as urine, feces, soapy water, or irritating chemicals. Diaper rash and “dishpan hands” are examples of common causes of irritant contact dermatitis (Figure 17.3). Protecting the skin from the irritating substance with zinc oxide ointment, frequent diaper changes, or the use of rubber gloves is very effective in preventing irritant contact dermatitis.

FIGURE 17.3 Occupational irritant contact dermatitis in a woman whose hands are exposed to chemicals while making cowboy hats in Texas. (Used with permission of Richard P. Usatine, MD. From Usatine RP, Smith MA, Mayeux EJ, Jr, Chumley H. The Color Atlas of Family Medicine. 2nd ed. McGraw-Hill, Inc; 2013.)
Allergic Contact Dermatitis
In contrast to atopic dermatitis, allergic contact dermatitis (ACD) is a T-cell-mediated immune reaction to a contact with specific substances. The appearance of the lesions varies from eczematous and papular red to vesicular lesions as seen with poison, oak, ivy, and sumac (Rhus or Toxicodendron). Chronic ACD appears as red lichenified areas. What is unique and diagnostic about ACD is the pattern of the rash is limited to the area of the skin that has been in contact with the allergens. ACD due to laundry detergent is limited to places that sweat or have forced contact (armpits, neck/chest, belt/underwear lines). Nickel is a common cause of ACD and since it is commonly found in jewelry the lesions occur where earrings, bracelets, or necklaces are worn (Figure 17.4). Also, leather is a common allergen and lesions are found only where the leather makes contact with the skin, i.e., the lesions of ACD due to leather watch bands are limited to a narrow area of the wrist (Figure 17.5 shows ACD to shoe leather). Latex is another common allergen causing ACD. Lesions are limited to areas of contact with latex such as waistbands of underwear, upper portions of men’s socks, and outline of latex gloves. ACD secondary to Rhus species can be linear where the plant touched the patient’s skin as they walked by (Figure 17.6). Finally, avoid recommending topical medications that cause ACD. Benzocaine, neomycin, and topical diphenhydramine can cause ACD in up to 25% of patients who use them. Since they do not impact the common skin flora (neomycin) or have very limited efficacy (diphenhydramine and benzocaine), use more effective and useful alternatives.
FIGURE 17.4 Patient moved up his ring to show the allergic contact dermatitis secondary to a nickel allergy to the ring. (With permission from Milgrom EC, Usatine RP, Tan RA, Spector SL. Practical Allergy. Philadelphia, PA: Elsevier; 2004. Copyright Elsevier.)

FIGURE 17.5 Allergic contact dermatitis from new shoes. This is the typical distribution found on the dorsum of the feet. (With permission from Milgrom EC, Usatine RP, Tan RA, Spector SL. Practical Allergy. Philadelphia, PA: Elsevier; 2004. Copyright Elsevier.)


FIGURE 17.6 Multiple lines of vesicles from poison oak on the arm. (With permission from Milgrom EC, Usatine RP, Tan RA, Spector SL. Practical Allergy. Philadelphia, PA: Elsevier; 2004. Copyright Elsevier.)
• SCALY DERMATOSES
Xerosis, also known as dry flaky skin, is easily treated with emollients. In keratosis pilaris old skin cells in hair follicles get stuck, forming a scaly, horny plug that is sometimes darker than surrounding skin or may be red in dry weather conditions. It occurs primarily on the outer aspects of the upper arms and occasionally the thighs and cheeks. It is easily treatable with several weeks of a mild keratolytic containing 5% to 12% lactic acid.
Seborrhea/Seborrheic Dermatitis
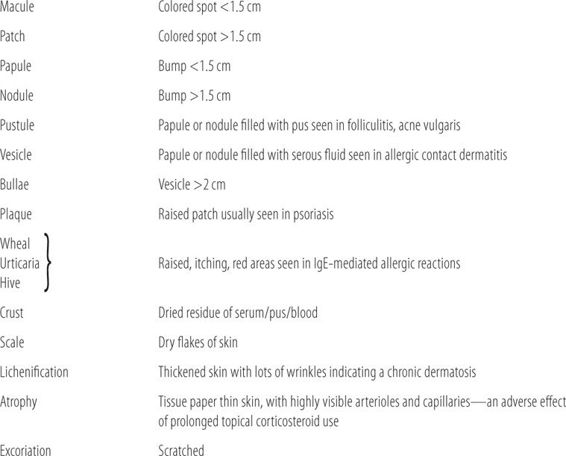
Both disorders are a result of a local immune reaction to substances produced by a yeast known as Malassezia furfur (previously known as Pityrosporum ovale). Seborrhea, aka dandruff, produces scales in the scalp. Seborrheic dermatitis appears as yellow, greasy scales over an eczematous-like lesion (Figure 17.7). The lesions occur primarily along the scalp line, nasolabial fold, eyebrows, eyelashes, ears, and over the sternum. It is associated with patients with Parkinson disease. These disorders are not curable, but can be easily controlled with shampoos and topical preparations containing selenium sulfide or zinc pyrithione. Shampooing the hair with selenium sulfide or zinc pyrithione at least weekly maintains remission. More severe cases of seborrheic dermatitis may require topical corticosteroids in addition to the antimalassezia products.
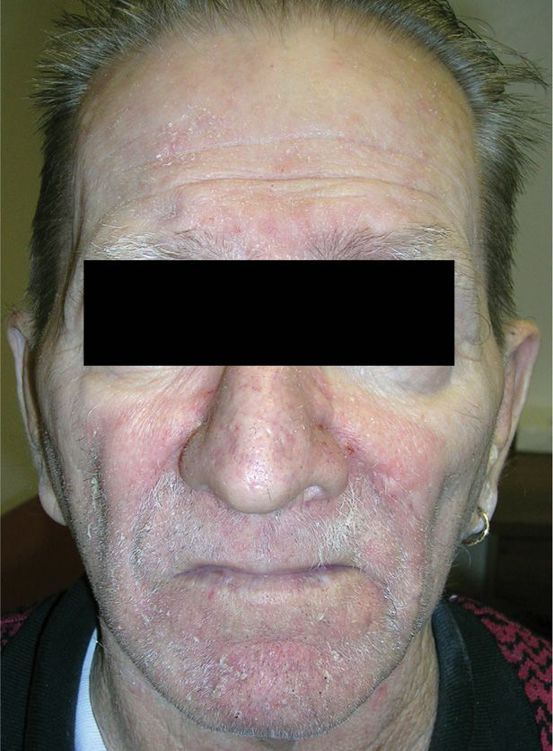
FIGURE 17.7 Seborrheic dermatitis following the typical distribution on the face of a 59-year-old man. Note the prominent scale and erythema on his forehead, glabella, and beard region. (Used with permission of Richard P. Usatine, MD. From Usatine RP, Smith MA, Mayeux EJ, Jr, Chumley H. The Color Atlas of Family Medicine. 2nd ed. McGraw-Hill, Inc; 2013.)
Psoriasis
Psoriasis is a complex immunological reaction involving T-cell proliferation and cytokine release. It presents with raised plaques with sharp margination. Many lesions have adherent silver/white scales that bleed if pulled off (Figure 17.8). The most common sites are the elbows and knees, but can occur anywhere on the body. As many as 10% of patients have an accompanying arthritis (psoriatic arthritis). Recently, psoriasis was found to be associated with an increased risk of cardiovascular disease. Only single, small, coin-sized lesions are potentially amenable to self-care. Most patients should be referred to a dermatologist for definitive therapy.

FIGURE 17.8 Typical plaque psoriasis on the elbow and arm. (Used with permission of Richard P. Usatine, MD. From Usatine RP, Smith MA, Mayeux EJ, Jr, Chumley H. The Color Atlas of Family Medicine. 2nd ed. McGraw-Hill, Inc; 2013.)
• BACTERIAL INFECTIONS
Bacterial infections of the skin usually involve normal skin flora. Normal flora include β-hemolytic Streptococcus pyogenes, several staphylococcal species including S. epidermidis, S. aureus, and the more antibiotic-resistant community-acquired methicillin-resistant Staphylococcus aureus (CA MRSA). Bacterial infections of the skin require a break in the skin to allow the opportunistic normal flora to gain entrance. Insect bites, minor trauma, lacerations, and abrasions, plus conditions favorable for bacterial growth are all that is required for a bacterial infection to start. Drastically lowering the bacterial count by immediate vigorous and thorough cleaning of even the smallest break in the skin with soap and water drastically reduces the incidence of bacterial infections. While many bacterial infections have separate and sometimes confusing names, even the most superficial infection, like impetigo, can progress to a larger infection involving surrounding soft-tissue known as cellulitis. Bacterial cellulitis is characterized by four to five symptoms. Lesions are swollen, very warm or hot to the touch, red in color, painful, and sometimes are associated with purulent material or pus (neutrophils used to fight the bacterial infection). Also they tend to spread or grow if untreated (Figure 17.9). Most bacterial skin infections require systemic antibiotic therapy. Bacterial skin infections can be confirmed with a complete blood count where the white blood cell differential count shows greater than 10,000 WBCs with more than 80% of the total WBC count consisting of mature and immature neutrophils (PMNs). Cellulitis can also be confirmed by marking the outer borders of the red swollen area with ink. If the red swollen area expands outside ink lines, then high likelihood of bacterial cellulitis exists.
FIGURE 17.9 Cellulitis of the foot of a diabetic person in which there is possible necrosis and gangrene of the second toe, requiring hospitalization and a podiatry consult. (Used with permission of Richard P. Usatine, MD. From Usatine RP, Smith MA, Mayeux EJ, Jr, Chumley H. The Color Atlas of Family Medicine. 2nd ed. McGraw-Hill, Inc; 2013.)

Impetigo
Impetigo is a superficial bacterial infection primarily caused by group A β-hemolytic Streptococcus pyogenes (GABHS). The role of staphylococcal species in classical impetgo is a controversial issue. It usually presents with a yellow or honey-colored crust of serosanguineous fluid (Figure 17.10).
FIGURE 17.10 Typical honey-crusted plaque on the lip of an adult with impetigo. (Used with permission of Richard P. Usatine, MD. From Usatine RP, Smith MA, Mayeux EJ, Jr, Chumley H. The Color Atlas of Family Medicine. 2nd ed. McGraw-Hill, Inc; 2013.)

Bullous Impetigo
Bullous impetigo is also a superficial lesion that presents with vesicles and bullae. Staphylococcus aureus is the causative agent (Figure 17.11).

FIGURE 17.11 Bullous impetigo secondary to methicillin-resistant Staphylococcus aureus (MRS) on the leg of an 11-year-old child. Note the surrounding cellulitis. Source: Reproduced with permission from Wolff KA, Johnson RA, Saavedra AP, eds. Fitzpatrick’s Color Atlas and Synopsis of Clinical Dermatology. 7th ed. New York: McGraw-Hill, Inc; 2013. Fig. 25-12. Copyright © McGraw-Hill Education LLC.
Folliculitis
Folliculitis is a mildly infected hair follicle with little or no cellulitis. It presents primarily as a pustule surrounding a single hair follicle (Figure 17.12, looks like bacterial folliculitis). Generally, these do not require systemic treatment.

FIGURE 17.12 Eosinophilic folliculitis on the back of an HIV-positive man. (Used with permission of Richard P. Usatine, MD. From Usatine RP, Smith MA, Mayeux EJ, Jr, Chumley H. The Color Atlas of Family Medicine. 2nd ed. McGraw-Hill, Inc; 2013.)
Furuncle
A furuncle, also known as a “boil,” is a local cellulitis, arising from a single hair follicle (a folliculitis gone wild), usually caused by Staphylococcus aureus (Figure 17.13). Some furuncles are abscess like, with a purulent center and relatively avascular core. Most furuncles do not require systemic antibiotics, but should be surgically drained or “lanced” (opening the avascular core to let the pus drain out) to clear up the infection.

FIGURE 17.13 Isolated single furuncle in an adult woman. (Used with permission of Richard P. Usatine, MD. From Usatine RP, Smith MA, Mayeux EJ, Jr, Chumley H. The Color Atlas of Family Medicine. 2nd ed. McGraw-Hill, Inc; 2013.)
Carbuncle
A carbuncle is a large furuncle with a larger area of local cellulitis that involves multiple hair follicles with connecting sinus tracts between follicles. Surgical drainage can be effective but depending on the size and location of the carbuncle, systemic antibiotic therapy may be required.
While the term cellulitis is a generic term for a soft tissue bacterial infection, several have been given specific names due to unique characteristics.
Paronychia is a minor cellulitis around a cuticle.
Erysipelas is a cellulitis on the face, which moves very rapidly along the fascia due to production of hyaluronidase produced by the causative agent group A β-hemolytic Streptococcus pyogenes. It produces little or no purulent material and is a medical emergency due to the close proximity of tracts near the eyes that provide a relatively easy access into the brain.
Necrotizing Fasciitis
Also known as “flesh-eating bacteria,” it is usually a multiorganism, mixed aerobe/anaerobe infection including group A β-hemolytic Streptococcus pyogenes but can be caused by GABHS alone. GABHS, which produces hyaluronidase allows the infection to move along the fascia, quickly destroying surrounding soft tissue. Failure to quickly identify and appropriately treat this condition can result in permanent loss of large amounts of soft tissue and extremities and may even be fatal. Immunocompromised patients and those with poor peripheral circulation such as patients with poorly controlled diabetes mellitus and a “diabetic foot” are most susceptible (Figure 17.14).

FIGURE 17.14 Necrotizing fasciitis with gangrene. Even with a radical hemipelvectomy this patient did not survive. (Used with permission of Fred Bongard, MD.)
Acneiform Lesions
Acne is defined as an inflammatory, follicular, papular, and pustular eruption involving the pilosebaceous apparatus. The term pustular implies bacterial etiology, hence its inclusion under bacterial infections. In reality, bacterial involvement in acneiform lesions is almost always secondary.
Acne Vulgaris Acne vulgaris is the technical name for typical teenage acne. While the primary pathological driver is testosterone, bacteria (Propionibacterium acnes) are a significant part of the overall pathological process and are one target in the treatment of this common disorder. It is a disease involving the vellus hair follicle, where the hair remains invisible inside the follicle. Comedone formation, plugging of the hair follicle, is an integral step in the pathological process (Figure 17.15 shows an advanced case of acne).
FIGURE 17.15 Severe nodulocystic acne with scarring in a 16-year-old boy. (Used with permission of Richard P. Usatine, MD. From Usatine RP, Smith MA, Mayeux EJ, Jr, Chumley H. The Color Atlas of Family Medicine. 2nd ed. McGraw-Hill, Inc; 2013.)

Acne Rosacea Acne rosacea, preferably called rosacea, occurs primarily on the face in adults. One version, the papulopustular type, has papular lesions and tiny pustule-like pimples, but its pathogenesis is totally different than acne vulgaris. It was thought to be a form of acne vulgaris because it responds to the same antibiotics that work in acne vulgaris; hence, it is still incorrectly classified as an acne. While the exact cause is unknown, it is an abnormality of the immune system that causes an inflammatory reaction. It occurs exclusively in adults and has two major presentations. The erythematotelangiectatic version presents as persistent erythema of the central face, with prolonged flushing, burning, or stinging, and is the most resistant to treatment (Figure 17.16). The papulopustular version mentioned above responds well to 1/10th of the dose of doxycycline used to treat acne vulgaris due to its anti-inflammatory properties. Rosacea symptoms are aggravated by exposure to sunlight, ingestion of ethanol, or exposure to windy conditions. It is more common in women and the pattern of the lesions usually differs by gender. The male pattern is more frequently vertical (forehead, nose, chin), while the female pattern tends to be more horizontal (cheeks under eyes, nose). Untreated rosacea can lead to excessive tissue growth around the nose (rhinophyma) (Figure 17.17).
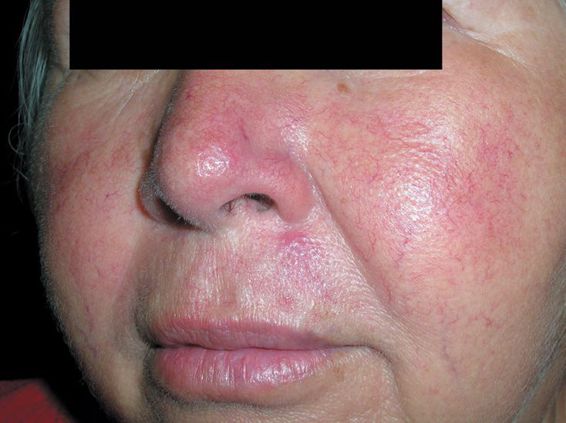
FIGURE 17.16 Erythematotelangiectatic subtype of rosacea in a middle-aged Hispanic woman. (Used with permission of Richard P. Usatine, MD. From Usatine RP, Smith MA, Mayeux EJ, Jr, Chumley H. The Color Atlas of Family Medicine. 2nd ed. McGraw-Hill, Inc; 2013.)
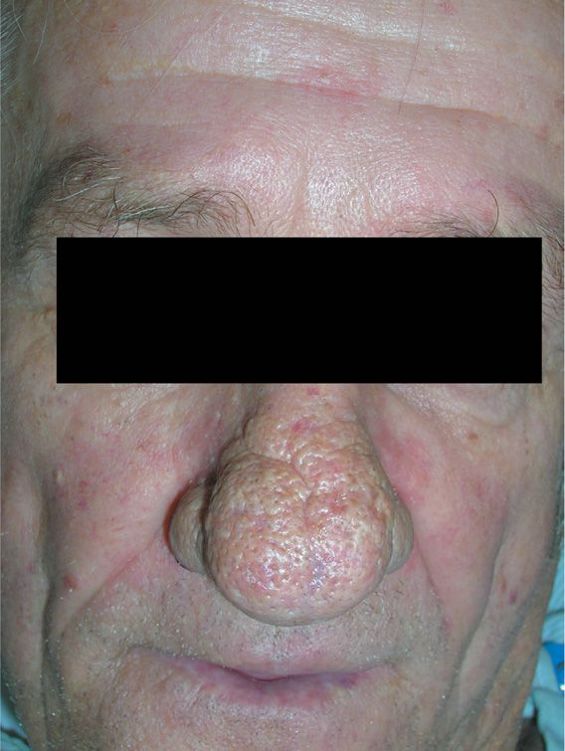
FIGURE 17.17 Rhinophymatous rosacea in an older man who does not drink alcohol. Although this is often called a WC Field nose, it is not necessarily related to heavy alcohol use. (Used with permission of Richard P. Usatine, MD. From Usatine RP, Smith MA, Mayeux EJ, Jr, Chumley H. The Color Atlas of Family Medicine. 2nd ed. McGraw-Hill, Inc; 2013.)
• VIRAL INFECTIONS
Verrucae (Warts)
Viral in etiology there are two main types of warts, both of which present as external growths of skin above the normal surface. Common warts can occur anywhere, are nonpainful, and are easily treated with nonprescription remedies (Figure 17.18). Plantar warts occur on the bottom of the foot, have significant tissue below the skin surface, can be painful, and are very resistant to treatment, usually requiring referral to a dermatologist or podiatrist (Figure 17.19).
FIGURE 17.18 Common warts on the hands of an 11-year-old girl. These periungual warts are particularly difficult to eradicate. (Used with permission of Richard P. Usatine, MD. From Usatine RP, Smith MA, Mayeux EJ, Jr, Chumley H. The Color Atlas of Family Medicine. 2nd ed. McGraw-Hill, Inc; 2013.)


FIGURE 17.19 Plantar warts. Note small black dots in the warts that represent thrombosed vessels. Large plantar warts such as these are called mosaic warts. (Used with permission of Richard P. Usatine, MD. From Usatine RP, Smith MA, Mayeux EJ, Jr, Chumley H. The Color Atlas of Family Medicine. 2nd ed. McGraw-Hill, Inc; 2013.)
Herpes Simplex
Herpes simplex episodically presents as painful vesicles located on the lips and face (type 1, fever blister, cold sore) (Figure 17.20) or on the genitals (type 2). It is usually a chronic, recurrent condition, with acute episodes occurring periodically and lasting 7 to 10 days. In between acute episodes, the virus resides asymptomatically in local sensory nerves. Multiple physical and emotional stresses are associated with acute attacks. The disease is contagious and can be transferred to others by contact with visible lesions.

FIGURE 17.20 Orolabial herpes simplex virus in an adult woman showing deroofed blisters (ulcer). (Used with permission of Richard P. Usatine, MD. From Usatine RP, Smith MA, Mayeux EJ, Jr, Chumley H. The Color Atlas of Family Medicine. 2nd ed. McGraw-Hill, Inc; 2013.)
Herpes Zoster
Herpes zoster causes chicken pox in children and a much more devastating disease, shingles in older adults. Once a patient has chicken pox as a child, the body’s immune system walls it off in sensory nerves. Any reduction in the immune control of the virus will result in the appearance of typical painful vesicular lesions. In shingles, rather than occurring in random patterns, the lesions appear in a linear fashion along skin dermatomes (Figure 17.21). The vesicular eruption is generally preceded by a prodrome involving pain and itching lasting several days. Shingles is predominantly a disease of patients 60 years of age or older. If untreated, lesions can last up to 5 to 8 weeks. The major complication with shingles is postherpetic neuralgia (PHN), which can last for months or even become permanent. Up to 40% of patients with shingles develop PHN. In about 10% of patients, it lasts a year or longer, PHN is a major cause for visits to pain specialists. Treatment with antivirals initiated within 72 hours of onset may reduce severity of the pain and increases the rate of healing of shingles lesions. While there have been few studies, it appears that treatment with antivirals does not prevent PHN, but does decrease its duration.
FIGURE 17.21 A 14-year-old boy with severe case of herpes zoster in a thoracic distribution. (Used with permission of Richard P. Usatine, MD. From Usatine RP, Smith MA, Mayeux EJ, Jr, Chumley H. The Color Atlas of Family Medicine. 2nd ed. McGraw-Hill, Inc; 2013.)

• FUNGAL INFECTIONS
Tineas
Fungal infections labeled as tineas are usually caused by dermatophytes such as Trichophyton and Microsporum species. Their medical names are determined by location. They have a common appearance regardless of location. They are sharply marginated, have central clearing, and are reddish-brown in color.
Tinea faciei is located on the face, aka ringworm.
Tinea corporis is located on the trunk and lesions are usually asymmetrical rather than circular (Figure 17.22).

FIGURE 17.22 Tinea corporis on the shoulder of this young girl. This is a very typical annular pattern and the cat on the sweatshirt might be a clue to an infected pet at home spreading a Microsporum dermatophyte to its owner. Note the concentric rings with scaling, erythema, and central sparing. (Used with permission of Richard P. Usatine, MD. From Usatine RP, Smith MA, Mayeux EJ, Jr, Chumley H. The Color Atlas of Family Medicine. 2nd ed. McGraw-Hill, Inc; 2013.)
Tinea pedis: Otherwise known as athlete’s foot, its presentation differs from those found on the face and trunk. There are three types of lesions: dry moccasin like scale on the soles and sides of the feet, interdigital (between the toes) (Figure 17.23), and the vesicular/bullous form.
FIGURE 17.23 Tinea pedis seen in the interdigital space between the fourth and fifth digits. This is the most common area to see tinea pedis. (Used with permission of Richard P. Usatine, MD. From Usatine RP, Smith MA, Mayeux EJ, Jr, Chumley H. The Color Atlas of Family Medicine. 2nd ed. McGraw-Hill, Inc; 2013.)

Tinea cruris: Also known as jock itch, tinea cruris, located in the groin and genital area, presents like lesions on the face and trunk and patients may contract it via autoinnoculation by pulling on their underwear over tinea pedis (Figure 17.24). Therefore, in order to treat jock itch, antifungals must be applied to the groin and the feet to prevent recurrence.

FIGURE 17.24 A 54-year-old man with tinea cruris and corporis for decades despite multiple treatments with oral antifungal medications. His cultures show T. rubrum sensitive to all the typical oral antifungal medications, but his tinea never completely clears. He does not have a known immunodeficiency but his immune system appears not to recognize the T. rubrum as foreign. (Used with permission of Richard P. Usatine, MD. From Usatine RP, Smith MA, Mayeux EJ, Jr, Chumley H. The Color Atlas of Family Medicine. 2nd ed. McGraw-Hill, Inc; 2013.)
Tinea Versicolor
Tinea versicolor is misnamed since it is caused by Malassezia species. Many references list it as pityriasis versicolor. While these lesions are a very pale reddish-brown, there is generally no central clearing (Figure 17.25). Sometimes it looks like patches of dry flaky skin on pale complected patients. In patients with darker complexions or suntans, they appear as white patches (Figure 17.26).
FIGURE 17.25 Large areas of pink tinea versicolor on the shoulder in a cape-like distribution. (Used with permission of Richard P. Usatine, MD. From Usatine RP, Smith MA, Mayeux EJ, Jr, Chumley H. The Color Atlas of Family Medicine. 2nd ed. McGraw-Hill, Inc; 2013.)


FIGURE 17.26 Patches of hypopigmentation across the back caused by tinea versicolor in a young Latino man. Vitiligo is on the differential diagnosis in this case. A KPH preparation confirmed tinea versicolor. (Used with permission of Richard P. Usatine, MD. From Usatine RP, Smith MA, Mayeux EJ, Jr, Chumley H. The Color Atlas of Family Medicine. 2nd ed. McGraw-Hill, Inc; 2013.)
FIGURE 17.27 Candida inguinal eruption in a 61-year-old man after a course of antibiotics for bronchitis. Note the satellite lesions. (Used with permission of Richard P. Usatine, MD. From Usatine RP, Smith MA, Mayeux EJ, Jr, Chumley H. The Color Atlas of Family Medicine. 2nd ed. McGraw-Hill, Inc; 2013.)

Candida
Fungal infections caused by Candida species (also known as Monilia) are easy to differentiate from other fungal skin infections. Lesions are usually fiery red, may appear shiny, and are found in moist or intertriginous areas, i.e., under the breasts, genitals, skin folds. In addition, candidal skin infections are not sharply marginated, but they have red, papular “satellite lesions” just outside the main red area (Figure 17.27). In addition, patients who develop candidiasis tend to have compromised immune systems or poorly controlled diabetes mellitus. All patients with candidal skin infections or vaginitis should be questioned and potentially tested for diabetes mellitus if not previously diagnosed, since that may be the initial presenting symptom of their diabetes mellitus.
• DRUG-INDUCED SKIN REACTIONS
Two Important Rules
When asked to evaluate a skin rash in a specific patient for medication etiology, remember two things. First, do not assume that all adverse dermatological reactions occur within 24 to 48 hours of medication administration. If this is a first-time exposure to the medication, the reaction may occur up to 2 weeks after the drug is stopped because it may take the body up to 14 days to fully react immunologically. For example, a patient completes a 7-day regimen of trimethoprim-sulfamethoxazole for a urinary tract infection. Four days later, the symptoms recur, and assuming resistance to the previous regimen, the patient is started on ciprofloxacin. Two days later, the patient develops urticaria. The natural assumption would be that the ciprofloxacin was the causative agent. However, if the initial prescription was the patient’s first exposure to a sulfonamide, the skin reaction could be just as easily due to the sulfonamide and not the ciprofloxacin. Second, other infections or autoimmune disorders can also cause these same drug reactions and must be ruled out before assuming the medication caused the reaction. For example, in a patient presenting with erythema nodosum in Southern Arizona, providers automatically think of valley fever (coccidioidomycosis) as the most likely diagnosis, since it is endemic to the area and erythema nodosum is a very common presentation of that infection. All patients in Southern Arizona will receive a diagnostic workup for coccidioidomycosis if they present with erythema nodosum, regardless of any medication they are taking.
Severe, Potentially Life-Threatening Reactions
There are two sequences of reactions that begin with skin rashes. If patients with that initial dermatological reaction are subsequently given that drug or one in the same pharmacological class, the next reaction may be more severe and even fatal. Patients should be warned never to take that class of medication again for concern over escalation to a more severe reaction in that group and its potentially lethal results. These two types of reactions are discussed in more detail.
IgE-Mediated Reactions
Urticaria Also known as hives, or wheals, urticaria is an IgE-mediated, type 1 immunological reaction. Urticaria presents as multiple pale pink or red raised areas of skin (wheals) that are intensely pruritic (itchy) (Figure 17.28). They may coalesce into larger lesions (Figure 17.29). Individual lesions last only 24 to 36 hours, but as long as the patient is still exposed to the allergen or is untreated, new wheals will continue to appear. Normally antihistamines and in some cases systemic corticosteroids will cause the lesions to stop erupting.

FIGURE 17.28 Urticaria that occurred within an hour after a boy was given ibuprofen to treat a high fever. (Used with permission of Richard P. Usatine, MD. From Usatine RP, Smith MA, Mayeux EJ, Jr, Chumley H. The Color Atlas of Family Medicine. 2nd ed. McGraw-Hill, Inc; 2013.)
FIGURE 17.29 Note the confluence of wheals with a well-demarcated border on the arm of the man with acute urticarial due to trimethoprim-sulfamethoxazole. (Used with permission of Richard P. Usatine, MD. From Usatine RP, Smith MA, Mayeux EJ, Jr, Chumley H. The Color Atlas of Family Medicine. 2nd ed. McGraw-Hill, Inc; 2013.)

Angioneurotic Edema Also known as angioedema, angioneurotic edema is the second in the sequence of serious IgE-mediated dermatological reactions. Wheals occur in deeper layers of the skin, usually the lips, face, tongue, and eyes, but can affect hands and feet as well (Figure 17.30). Usually nonpruritic, they can coexist with urticaria. Those occurring in the mouth and pharynx can cause local airway obstruction and in more severe cases require tracheostomy and intubation. Rarely the wheals can occur only in the gastrointestinal tract, causing initial manifestations of GI pain/discomfort, nausea and vomiting. Angiotensin converting enzyme inhibitors can cause angioedema. Patients should be warned to go immediately to the emergency room if any unusual swelling in the face occurs.
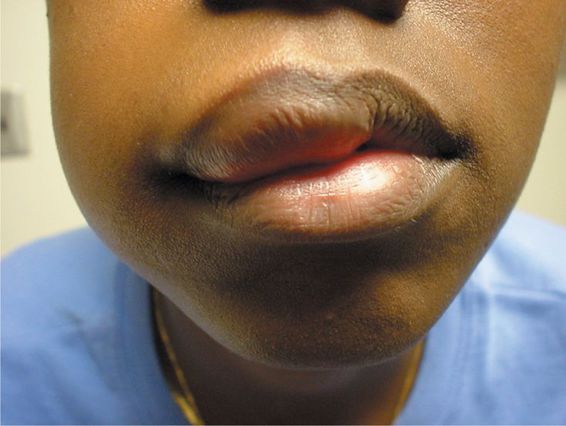
FIGURE 17.30 Young black woman with angioedema after being started on an angiotensin-converting-enzyme (ACE) inhibitor for essential hypertension. (Used with permission of Adrian Casillas, MD.)
Anaphylaxis The third and most serious reaction is anaphylaxis, which can be fatal. Therefore, patients with urticaria should be warned about the potentially more severe consequences if exposed to agent or the related agents in the future.
T-Lymphocyte-Mediated Reactions
Erythema Multiforme The term erythema multiforme (EM) indicates that it occurs in multiple forms and is used interchangeably with other stages of this T-lymphocyte-mediated reaction sequence, which makes it somewhat confusing. Patients may present with varying degrees of each reaction, e.g., many patients with toxic epidermal necrolysis syndrome (TENS) will also have oral involvement that is consistent with Stevens-Johnson syndrome.
Classic Erythema Multiforme Also called erythema multiforme minor, or mild to moderate erythema multiforme, it initially presents with a maculopapular/vesicular eruption on the trunk (Figure 17.31) that is usually accompanied by “target lesions” on the hands and forearms (Figure 17.32). This is like urticaria in the IgE-mediated sequence. The presence of target lesions puts the patient at high risk for potentially more severe reactions in the sequence that could result in fatality.

FIGURE 17.31 Target lesions on the back of a 14-year-old boy who received penicillin for pneumonia. (Used with permission of Dan Stulberg, MD.)

FIGURE 17.32 Erythema multiforme in a 43-year-old woman that recurs every time she breaks out with genital herpes. Target lesions on hand. (Used with permission of Richard P. Usatine, MD. From Usatine RP, Smith MA, Mayeux EJ, Jr, Chumley H. The Color Atlas of Family Medicine. 2nd ed. McGraw-Hill, Inc; 2013.)
Stevens-Johnson Syndrome Also known as erythema multiforme major, Stevens-Johnson syndrome presents as vesicular and bullous lesions of the mucous membranes including the mouth, eyes, and gastrointestinal tract (Figure 17.33). Like angioedema in the IgE sequence, it can be fatal in some cases.

FIGURE 17.33 Stevens-Johnson syndrome that evolved into toxic epidermal necrolysis in a human immunodeficiency viruspositive man with a CDR of 6. He presented to the emergency department with fever and rash on face, eyes, and mouth. Chest x-ray suggested pneumonia, so he was started on azithromycin, ceftriaxone, and trimethoprim-sulfamethoxazole. He developed bulla on skin and a skin biopsy confirmed toxic epidermal necrolysis, possibly secondary to one of the firmed toxic epidermal necrolysis, possibly secondary to one of the antibiotics. He was transferred to a burn unit and given intravenous γ-globulin 1 g/kg for 3 days. The patient survived. Oral lesion. (Used with permission of Robert T. Gilson, MD.)
Toxic Epidermal Necrolysis Also known as TENS (toxic epidermal necrolysis syndrome), it is the last and most dangerous reaction in this sequence. It presents as widespread epidermal necrosis, resembling a massive third-degree burn (Figure 17.34). There is a 20% to 30% mortality despite treatment. Patients are usually treated in a burn unit following treatment protocols used to manage third-degree burns.
FIGURE 17.34 Toxic epidermal necrolysis with desquamation of skin on the hand. (Used with permission of the University of Texas Health Sciences Center, Division of Dermatology.)

Erythema multiforme is like urticaria in that patients with the drug induced form of EM should be warned about the potentially more severe consequences if exposed to that agent or related agents in the future.
Drug Hypersensitivity Syndrome (DHS) For several decades, DHS was called anticonvulsant hypersensitivity syndrome because when initially described it was most frequently associated with anticonvulsant medication. It is characterized by an initial skin reaction followed by involvement of internal organ systems, including the liver, kidney, central nervous system, and hematopoietic system. Because of the high incidence of eosinophilia, it is also known as drug reaction with eosinophilia and systemic symptoms (DRESS). While it has been reported to be caused by many classes of medications, anticonvulsant drugs, sulfonamides and related drugs are the most frequent causes. DHS presents initially with a fever, followed by a widespread maculopapular-pustular rash on the trunk, arms, and legs. Eosinophilia occurs in 50% to 90% of cases. Abnormal lymphocytosis is found in 30% of patients and 20% have lymphadenopathy on physical examination. Headaches occur in 10% to 15% of patients and they can be confused with aseptic meningitis. Internal organ damage occurs last and most patients have elevated liver function tests and/or renal function tests. There is an 8% mortality rate in DHS. Rarely, there are posttreatment autoimmune disorders such as myocarditis, thyroiditis, or pancreatitis, which may manifest itself as type 1 diabetes mellitus.
• MISCELLANEOUS DERMATOLOGICAL DRUG REACIONS
Maculopapular Skin Rashes
These rashes usually occur on the trunk. When pressed, the lesions blanch or lose color.
Generally, they are nonimmunological and are not contraindications to future use of the expected causative drug. Examples include measles and the “ampicillin rash.”
Erythema Nodosum
Erythema nodosum is easy to diagnose because of its unusual presentation. It presents with red to reddish-brown circular lesions 1 to 2 cm in diameter that only occur from the knees to the feet, usually concentrated on the shins (Figure 17.35). When palpated, they are firm and painful.

FIGURE 17.35 Erythema nodosum secondary to a group A β-hemolytic Streptococcus in a young woman. (Used with permission of Richard P. Usatine, MD. From Usatine RP, Smith MA, Mayeux EJ, Jr, Chumley H. The Color Atlas of Family Medicine. 2nd ed. McGraw-Hill, Inc; 2013.)
Fixed Drug Eruptions
Like erythema nodosum fixed drug eruptions are easy to diagnose because of their unique presentation. Fixed drug reactions occur as red plaques, frequently associated with vesicles. They most frequently occur in the groin, inner thigh, and genitalia. They generally heal in 1 to 3 weeks, many times with hypopigmentation. They are called fixed drug eruptions because reexposure to the same agent causes the lesions to appear on the exact same spot that they occurred initially.
Photosensitivity Reactions
Photosensitivity reactions to chemicals and medications can be divided into two main categories: phototoxic and photoallergic reactions. Phototoxic reactions are nonimmunological reactions manifested by increased susceptibility to sunburn. Phototoxic reactions are by far the most common. While UVB light is the usual cause of sunburn, UVA light is the culprit in drug-induced phototoxic reactions. UVA light reacts with certain medications in the skin, increasing sensitivity to sunburn. It is concentration dependent, so everyone will have the reaction if the drug concentration in the skin is high enough. Lowering the dose will make the reaction less likely to occur. Sunburn sensitivity will occur for as long as there is sufficient concentration of the drug in the skin. Tetracyclines and sulfonamides and related drugs such as diuretics and sulfonylureas are common causes. The sunburn only occurs in areas that are exposed to sunlight. Even UVA rays coming through a window and fluorescent lights are enough to cause the reaction.
Photoallergic reactions are uncommon and are immunological in nature, a form of delayed hypersensitivity reaction induced by UVA light in people who have been previously sensitized to the agent. The reaction looks like allergic contact dermatitis and a large percentage of the reactions are due to topical agents and chemicals including those from plants. Mostly, they are limited to sun exposed areas but can spread to nearby areas. While phototoxic reactions end when skin concentrations of the medication fall below interactive levels, photoallergic reactions can persist for extended periods even though the drug is no longer present in the body.
Adverse Reactions to Long-Term Use of High-Potency Fluorinated Topical Corticosteroids
Fluorinated, high-potency topical corticosteroids when used for prolonged periods of time and/or in areas with thin skin, e.g., face and groin, can cause unwanted visible adverse effects. The use of fluorinated topical corticosteroids on the face or in the groin area should only be prescribed by a dermatologist, who is better able to judge the risk of adverse effects versus the potential benefit. Inappropriate use of topical corticosteroids can result in the development of striae, better known as stretch marks and/or atrophy of the skin. Atrophy is an extreme thinning of the skin so that it is tissue paper thin, enabling the easy visualization of arterioles, venules, capillaries, and sometimes nerves.
• KEY REFERENCES
1. de Bruin Weller MS, Rockman H, Knulst AC, Brunijnzeel-Koomen CA. Evaluation of the adult patients with atopic dermatitis. Clin Exp Allergy. 2012;43:279-291.
2. Usatine RP, Riojas M. Diagnosis and management of contact dermatitis. Am Fam Physician. 2010;82:249-255.
3. Schwartz JR, Messenger AG, Tosti A, et al. A comprehensive pathophysiology of dandruff and seborrheic dermatitis-towards a more precise definition of scalp health. Acta Derm Venereol. 2013;93:131-137.
4. Gupta AK, Batra R, Bluhm R, Boekhout T, Dawson TL. Skin diseases associated with Malassezia species. J Am Acad Dermatol. 2004;51:785-798.
5. Keller EC, Tomecki KJ, Chadi Alraies M. Distinguishing cellulitis from its mimics. Cleve Clin J Med. 2012;79:547-552.
6. Baldwin HE. Diagnosis and treatment of rosacea: state of the art. J Drugs Dermatol. 2012;11:725-730.
7. Varade RS, Burkemper NM. Cutaneous fungal infections in the elderly. Clin Geriatr Med. 2013;29:461-478.
8. Ahmed AM, Pritichard S, Reichenberg J. A review of cutaneuous drug eruptions. Clin Geriatr Med. 2013;29:527-545.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



